Podcast
Questions and Answers
What initiates the secretion of FSH and LH at puberty?
What initiates the secretion of FSH and LH at puberty?
- Increased secretion of GnRH (correct)
- Decrease in testosterone levels
- Suppression of Sertoli cell activity
- Increase in inhibin levels
Which hormone primarily stimulates Leydig cells to produce testosterone?
Which hormone primarily stimulates Leydig cells to produce testosterone?
- FSH
- GnRH
- LH (correct)
- Inhibin
What role does FSH play in spermatogenesis?
What role does FSH play in spermatogenesis?
- Stimulates Leydig cells to secrete testosterone
- Suppresses testosterone secretion
- Inhibits production of androgen-binding protein
- Acts on Sertoli cells to promote spermatogenesis (correct)
What is the function of androgen-binding protein (ABP) in the testes?
What is the function of androgen-binding protein (ABP) in the testes?
How does the negative feedback mechanism control testosterone production?
How does the negative feedback mechanism control testosterone production?
What is the most common disorder associated with primary congenital male hypogonadism?
What is the most common disorder associated with primary congenital male hypogonadism?
Which condition is classified as a secondary cause of male hypogonadism?
Which condition is classified as a secondary cause of male hypogonadism?
What triggers Sertoli cells to release inhibin?
What triggers Sertoli cells to release inhibin?
What is the primary role of testosterone in spermatogenesis?
What is the primary role of testosterone in spermatogenesis?
What happens to blood testosterone levels when they become excessively high?
What happens to blood testosterone levels when they become excessively high?
What effect do high levels of oestrogen have on the release of GnRH, LH, and FSH?
What effect do high levels of oestrogen have on the release of GnRH, LH, and FSH?
What hormonal changes occur after the formation of the corpus albicans?
What hormonal changes occur after the formation of the corpus albicans?
Which is one of the primary actions of oestrogen in the hormonal birth control context?
Which is one of the primary actions of oestrogen in the hormonal birth control context?
How does progesterone function in hormonal birth control?
How does progesterone function in hormonal birth control?
Which phase is primarily associated with low levels of oestrogen and progesterone?
Which phase is primarily associated with low levels of oestrogen and progesterone?
What hormonal feedback effect occurs during the pre-ovulatory phase?
What hormonal feedback effect occurs during the pre-ovulatory phase?
What is the primary purpose of the combined pill in hormonal birth control?
What is the primary purpose of the combined pill in hormonal birth control?
What is one consequence of high levels of oestrogen during the menstrual cycle?
What is one consequence of high levels of oestrogen during the menstrual cycle?
What effect does the progesterone-only pill have on the menstrual cycle?
What effect does the progesterone-only pill have on the menstrual cycle?
What is the primary hormone secreted by Leydig cells found in the testes?
What is the primary hormone secreted by Leydig cells found in the testes?
Which statement accurately describes the function of Sertoli cells?
Which statement accurately describes the function of Sertoli cells?
Which hormone is primarily responsible for the regulation of spermatogenesis alongside testosterone?
Which hormone is primarily responsible for the regulation of spermatogenesis alongside testosterone?
What role does inhibin play in male reproductive physiology?
What role does inhibin play in male reproductive physiology?
Which hormone is known as interstitial cell-stimulating hormone (ICSH) in males?
Which hormone is known as interstitial cell-stimulating hormone (ICSH) in males?
What is the function of 5 alpha-reductase in the male reproductive system?
What is the function of 5 alpha-reductase in the male reproductive system?
Which of the following hormones is NOT involved in the hormonal regulation of the male reproductive system?
Which of the following hormones is NOT involved in the hormonal regulation of the male reproductive system?
Which of the following is a function of FSH in the male reproductive system?
Which of the following is a function of FSH in the male reproductive system?
What is the primary mechanism by which levonorgestrel inhibits ovulation?
What is the primary mechanism by which levonorgestrel inhibits ovulation?
During which stage of gestation does the process of organogenesis primarily occur?
During which stage of gestation does the process of organogenesis primarily occur?
Thalidomide, when used during pregnancy, is particularly associated with which of the following effects on the fetus?
Thalidomide, when used during pregnancy, is particularly associated with which of the following effects on the fetus?
Which teratogenic drug is characterized by its role as a vitamin K antagonist?
Which teratogenic drug is characterized by its role as a vitamin K antagonist?
Systemic use of aminoglycosides during pregnancy is primarily associated with which outcome for the fetus?
Systemic use of aminoglycosides during pregnancy is primarily associated with which outcome for the fetus?
Which drug is known to cause vaginal adenosis in female foetuses when administered during pregnancy?
Which drug is known to cause vaginal adenosis in female foetuses when administered during pregnancy?
What is a significant effect of retinoids such as etretinate when exposure occurs during pregnancy?
What is a significant effect of retinoids such as etretinate when exposure occurs during pregnancy?
What is the primary role of follicle-stimulating hormone (FSH) in the female reproductive cycle?
What is the primary role of follicle-stimulating hormone (FSH) in the female reproductive cycle?
Which of the following treatments is an antiandrogen used in prostate cancer therapy?
Which of the following treatments is an antiandrogen used in prostate cancer therapy?
What mechanism does sildenafil utilize to treat erectile dysfunction?
What mechanism does sildenafil utilize to treat erectile dysfunction?
What hormone is primarily secreted by the corpus luteum to prepare the endometrium for implantation?
What hormone is primarily secreted by the corpus luteum to prepare the endometrium for implantation?
What is the consequence of GnRH release inhibition by ovarian hormones?
What is the consequence of GnRH release inhibition by ovarian hormones?
Which hormone is responsible for inducing relaxation of the uterus during pregnancy?
Which hormone is responsible for inducing relaxation of the uterus during pregnancy?
What common condition affects one-third of males over age 60 related to the prostate?
What common condition affects one-third of males over age 60 related to the prostate?
What hormonal change triggers ovulation in the menstrual cycle?
What hormonal change triggers ovulation in the menstrual cycle?
What best describes the role of inhibin in the female reproductive system?
What best describes the role of inhibin in the female reproductive system?
What is a primary characteristic of benign prostatic hyperplasia?
What is a primary characteristic of benign prostatic hyperplasia?
Which event occurs during the pre-ovulatory phase of the menstrual cycle?
Which event occurs during the pre-ovulatory phase of the menstrual cycle?
What triggers the release of GnRH during the post-ovulatory phase when fertilization does not occur?
What triggers the release of GnRH during the post-ovulatory phase when fertilization does not occur?
Which medication is known to prevent estrogen production and is used in the treatment of endometriosis?
Which medication is known to prevent estrogen production and is used in the treatment of endometriosis?
What is the primary consequence of high oestrogen levels prior to ovulation?
What is the primary consequence of high oestrogen levels prior to ovulation?
Which treatment option has been linked to an increased risk of endometrial cancer among women using hormone replacement therapy?
Which treatment option has been linked to an increased risk of endometrial cancer among women using hormone replacement therapy?
Which hormonal level change occurs during the transition from the post-ovulatory phase to menstruation?
Which hormonal level change occurs during the transition from the post-ovulatory phase to menstruation?
What effect does combined hormonal contraceptive have on follicle development?
What effect does combined hormonal contraceptive have on follicle development?
What is the role of low oestrogen levels after the corpus albicans is formed?
What is the role of low oestrogen levels after the corpus albicans is formed?
How does progesterone function within the combined pill context?
How does progesterone function within the combined pill context?
What feedback effect predominates during the pre-ovulatory phase of the menstrual cycle?
What feedback effect predominates during the pre-ovulatory phase of the menstrual cycle?
Which aspect of hormonal birth control aims to make the endometrium unsuitable for implantation?
Which aspect of hormonal birth control aims to make the endometrium unsuitable for implantation?
Which physiological changes occur during ovulation as a result of hormonal signals?
Which physiological changes occur during ovulation as a result of hormonal signals?
What is the primary hormone responsible for stimulating ovulation in the female reproductive cycle?
What is the primary hormone responsible for stimulating ovulation in the female reproductive cycle?
Which hormone functions to relax the uterus during pregnancy by inhibiting contractions of the myometrium?
Which hormone functions to relax the uterus during pregnancy by inhibiting contractions of the myometrium?
Which condition is classified as a teratogenic effect observed when certain drugs are used during pregnancy?
Which condition is classified as a teratogenic effect observed when certain drugs are used during pregnancy?
In the female reproductive cycle, what triggers the surge in LH that leads to ovulation?
In the female reproductive cycle, what triggers the surge in LH that leads to ovulation?
What hormonal change occurs after the corpus luteum forms post-ovulation?
What hormonal change occurs after the corpus luteum forms post-ovulation?
Which mechanism describes how hormonal birth control primarily functions to prevent ovulation?
Which mechanism describes how hormonal birth control primarily functions to prevent ovulation?
What excess hormone is associated with negative feedback that inhibits the release of GnRH, LH, and FSH?
What excess hormone is associated with negative feedback that inhibits the release of GnRH, LH, and FSH?
What condition is commonly seen in males over 60 years old that relates to the prostate?
What condition is commonly seen in males over 60 years old that relates to the prostate?
How does sildenafil treat erectile dysfunction through its physiological mechanism?
How does sildenafil treat erectile dysfunction through its physiological mechanism?
Flashcards
Leydig Cells
Leydig Cells
Cells that are found in the space between the seminiferous tubules of the testes and secrete the male hormone testosterone.
Sertoli Cells
Sertoli Cells
Large cells located in the seminiferous tubules of the testes, responsible for nourishing developing sperm cells, forming a barrier between the blood and sperm, and responding to hormones like FSH and testosterone.
GnRH (Gonadotropin-Releasing Hormone)
GnRH (Gonadotropin-Releasing Hormone)
A hormone produced by the hypothalamus that triggers the release of LH and FSH from the pituitary gland.
FSH (Follicle-Stimulating Hormone)
FSH (Follicle-Stimulating Hormone)
Signup and view all the flashcards
LH (Luteinizing Hormone)
LH (Luteinizing Hormone)
Signup and view all the flashcards
Testosterone
Testosterone
Signup and view all the flashcards
Inhibin
Inhibin
Signup and view all the flashcards
5-Alpha Reductase
5-Alpha Reductase
Signup and view all the flashcards
What triggers the start of sperm production?
What triggers the start of sperm production?
Signup and view all the flashcards
What happens when GnRH is released?
What happens when GnRH is released?
Signup and view all the flashcards
What is the role of LH in sperm production?
What is the role of LH in sperm production?
Signup and view all the flashcards
How is testosterone made?
How is testosterone made?
Signup and view all the flashcards
How is testosterone production regulated?
How is testosterone production regulated?
Signup and view all the flashcards
What does FSH do during sperm production?
What does FSH do during sperm production?
Signup and view all the flashcards
What is the role of Sertoli cells?
What is the role of Sertoli cells?
Signup and view all the flashcards
Why is testosterone important for sperm development?
Why is testosterone important for sperm development?
Signup and view all the flashcards
How is sperm production regulated?
How is sperm production regulated?
Signup and view all the flashcards
What is male hypogonadism?
What is male hypogonadism?
Signup and view all the flashcards
What is Kallman's syndrome?
What is Kallman's syndrome?
Signup and view all the flashcards
What is benign prostatic hyperplasia (BPH)?
What is benign prostatic hyperplasia (BPH)?
Signup and view all the flashcards
What is prostate cancer?
What is prostate cancer?
Signup and view all the flashcards
What is a PDE5 inhibitor?
What is a PDE5 inhibitor?
Signup and view all the flashcards
What is the female reproductive cycle?
What is the female reproductive cycle?
Signup and view all the flashcards
What is GnRH?
What is GnRH?
Signup and view all the flashcards
What is FSH?
What is FSH?
Signup and view all the flashcards
What is LH?
What is LH?
Signup and view all the flashcards
What is progesterone?
What is progesterone?
Signup and view all the flashcards
What is relaxin?
What is relaxin?
Signup and view all the flashcards
Levonorgestrel
Levonorgestrel
Signup and view all the flashcards
Teratogens
Teratogens
Signup and view all the flashcards
Teratogenic drugs
Teratogenic drugs
Signup and view all the flashcards
Alcohol (ethanol)
Alcohol (ethanol)
Signup and view all the flashcards
Pre-ovulatory Phase
Pre-ovulatory Phase
Signup and view all the flashcards
Ovulation
Ovulation
Signup and view all the flashcards
Post-ovulatory Phase
Post-ovulatory Phase
Signup and view all the flashcards
Positive Feedback (Estrogen)
Positive Feedback (Estrogen)
Signup and view all the flashcards
Negative Feedback (Estrogen)
Negative Feedback (Estrogen)
Signup and view all the flashcards
Negative Feedback (Low estrogen, progesterone)
Negative Feedback (Low estrogen, progesterone)
Signup and view all the flashcards
Combined Pill (Hormonal Birth Control)
Combined Pill (Hormonal Birth Control)
Signup and view all the flashcards
Progesterone-only Pill (Hormonal Birth Control)
Progesterone-only Pill (Hormonal Birth Control)
Signup and view all the flashcards
How Hormonal Birth Control Works
How Hormonal Birth Control Works
Signup and view all the flashcards
Hormones in Menstrual Cycle
Hormones in Menstrual Cycle
Signup and view all the flashcards
Kallman's Syndrome
Kallman's Syndrome
Signup and view all the flashcards
Benign Prostatic Hyperplasia (BPH)
Benign Prostatic Hyperplasia (BPH)
Signup and view all the flashcards
Prostate Cancer
Prostate Cancer
Signup and view all the flashcards
PDE5 Inhibitor
PDE5 Inhibitor
Signup and view all the flashcards
Ovarian Cycle
Ovarian Cycle
Signup and view all the flashcards
Uterine (Menstrual) Cycle
Uterine (Menstrual) Cycle
Signup and view all the flashcards
Gonadotropin-Releasing Hormone (GnRH)
Gonadotropin-Releasing Hormone (GnRH)
Signup and view all the flashcards
Estrogen
Estrogen
Signup and view all the flashcards
Progesterone
Progesterone
Signup and view all the flashcards
Relaxin
Relaxin
Signup and view all the flashcards
Menstrual Phase
Menstrual Phase
Signup and view all the flashcards
Menstruation
Menstruation
Signup and view all the flashcards
Study Notes
Reproductive Endocrinology
- Recommended Reading:
- Rang and Dales Pharmacology - Chapter 34
- Tortora and Derrickson's Anatomy and Physiology - Chapter 28
- Practice MCQ questions: Available on Moodle.
- Topics to cover:
- Hormonal regulation of the male reproductive system
- Hormonal regulation of the female reproductive system
- Contraceptive pill
- Reproductive pathology and treatment
- Pregnancy/birth/lactation
- Teratogens
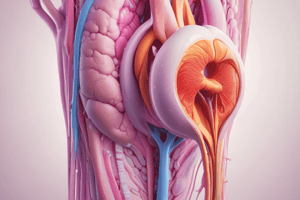
Male Reproductive System
-
Cells of the testes:
- Leydig cells: located between seminiferous tubules, secrete testosterone.
- Sertoli cells: embedded in the tubules, form the blood-testis barrier, nourish spermatocytes, mediate testosterone/FSH effects on spermatogenesis, phagocytose excess spermatids, and secrete inhibin.
-
Hormone control of Spermatogenesis:
- GnRH (gonadotrophin-releasing hormone): controls the release of FSH and LH, its release is inhibited by high testosterone levels.
- FSH (follicle-stimulating hormone): stimulates spermatogenesis.
- LH (luteinising hormone): stimulates testosterone secretion (also called interstitial cell-stimulating hormone (ICSH)).
- Testosterone and DHT (dihydrotestosterone): essential for spermatogenesis, development of external genitalia, and prostate function. 5-alpha-reductase converts testosterone to DHT.
-
Inhibin: regulates sperm production by inhibiting FSH.
-
Control of Testosterone Production:
- Negative feedback system regulates testosterone levels.
- Hypothalamus receptors detect increased testosterone levels. This inhibits GnRH secretion
- Reduced LH secretion from the anterior pituitary.
- Leydig cells produce less testosterone, returning blood levels to normal.
-
Male Hypogonadism:
- Primary congenital: Testicular agenesis (failure to develop), Klinefelter's syndrome (47XXY).
- Primary acquired: Bilateral orchitis (inflammation of testes), mumps, irradiation, or cytotoxic drugs.
- Secondary: Pituitary disorders, hypothalamic disorders (e.g., Kallman's syndrome — GnRH deficiency).
-
Aging in the male reproductive system:
- Enlargement of prostate (benign hyperplasia): common in men over 60. Symptoms include frequent urination, decreased force of stream, bed wetting, and sensation of incomplete emptying.
-
Prostate Cancer:
- Leading cause of male cancer death.
- Blood test for prostate-specific antigen (PSA).
- Antiandrogens (e.g., flutamide or cyproterone) used in treatment to block testosterone/DHT actions, preventing prostate cancer cell growth.
-
Erectile Dysfunction (Treatment):
- Viagra (Sildenafil citrate) – PDE5 inhibitor.
- Nitric oxide (NO) released by nerves diffuses into smooth muscle cells. Activates guanylate cyclase, increasing cGMP. cGMP activates protein kinase G, reduces [Ca2+], leading to vasodilation, and increased blood flow to the penis. Sildenafil is a selective inhibitor of PDE5.
Female Reproductive System
-
The Female Reproductive Cycle:
- Ovarian cycle: cyclic changes in ovaries, including the maturation of oocytes.
- Uterine (menstrual) cycle: concurrent changes in the uterine endometrium to prepare for fertilization.
-
Hormonal control (female):
- GnRH (gonadotropin-releasing hormone): secreted by hypothalamus, stimulates FSH and LH release from anterior pituitary. Its release is continuous but may be pulsatile.
- FSH (follicle-stimulating hormone): initiates follicular growth, stimulates ovarian follicles to secrete estrogens.
- LH (luteinising hormone): stimulates further ovarian follicle development, triggers ovulation, promotes corpus luteum formation, and produces estrogens, progesterone, relaxin and inhibin.
- Estrogens: main estrogen is β-estradiol. Promotes female reproductive structures and secondary sex characteristics, increases protein anabolism (bone building), lowers blood cholesterol and inhibits GnRH, LH and FSH release.
- Progesterone: primarily secreted by corpus luteum. Works with estrogens to prepare and maintain endometrium for implantation and mammary glands for milk production. Inhibits GnRH and LH secretion.
- Relaxin: produced by corpus luteum. Relaxes uterus during pregnancy, increasing pubic symphysis and uterine cervix flexibility.
- Inhibin: secreted by granulosa cells. Inhibits FSH and LH secretion.
-
Phases of the female reproductive cycle:
- Menstrual phase
- Pre-ovulatory phase (follicular stage)
- Ovulation
- Post-ovulatory phase (luteal phase)
-
Corpus luteum:
- If oocyte is not fertilized, the corpus luteum degenerates into corpus albicans reducing progesterone and estrogen levels, initiating menstruation.
- If oocyte is fertilized, the corpus luteum produces high levels of progesterone and estrogen to support pregnancy. Human chorionic gonadotropin (hCG) produced by the embryo maintains corpus luteum function during early pregnancy.
-
Hormonal interactions:
- Levels of estrogen and progesterone fluctuate throughout the cycle. These fluctuations initiate negative and positive feedback mechanisms, regulating GnRH, LH and FSH release and ovulation.
-
Causes of female hypogonadism:
- Primary congenital: problems in the ovaries, including Turner's or Noonan's syndromes.
- Primary acquired: damage to ovaries (e.g., chemotherapy, irradiation).
- Secondary: problems that stem from pituitary or hypothalamic disorders.
-
Aging in the female reproductive system:
- Menopause is associated with several symptoms: hot flashes, copious sweating, headache, vaginal dryness, depression, weight gain, and emotional fluctuations.
-
Endometriosis:
- Growth of endometrial tissue outside of the uterus.
-
Breast Cancer:
- Common cause of cancer in women
- Two genes increase susceptibility to breast cancer (BRCA1, BRCA2).
- Mutations of BRCA1 and BRCA2 also increase risk of ovarian cancer.
- Treatment involves hormone therapy, surgery (lumpectomy or mastectomy) radiation treatment, and chemotherapy.
-
Hormonal birth control:
-
Combined Pill: Oestrogen and progesterone inhibit FSH and follicle development. Progesterone prevents ovulation and makes cervical mucus inhospitable to sperm, and together they make the endometrium less receptive to implantation.
- Progesterone-only Pill: Levonorgestrel. Makes cervical mucus inhospitable to sperm, inhibits ovulation (by downregulating LH release).
- Morning-after Pill: Effective in preventing pregnancy if taken within 72 hours of unprotected intercourse.
-
Teratogens:
- Agents that cause birth defects.
- Include chemicals, drugs, cigarette smoking, and irradiation.
- Teratogens affect different processes depending on the stage of fetal development.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.