Podcast
Questions and Answers
What is the most common form of hip arthritis?
What is the most common form of hip arthritis?
- Osteoarthritis (correct)
- Pseudogout
- Gout
- Rheumatoid arthritis
Osteoarthritis of the hip is more common in younger individuals than older individuals.
Osteoarthritis of the hip is more common in younger individuals than older individuals.
False (B)
What type of pain can radiate to the buttocks or knee when experiencing hip osteoarthritis?
What type of pain can radiate to the buttocks or knee when experiencing hip osteoarthritis?
Pain in groin/thigh
The pain from hip osteoarthritis is often aggravated when the hip is ______.
The pain from hip osteoarthritis is often aggravated when the hip is ______.
Match the following factors with their association to hip osteoarthritis:
Match the following factors with their association to hip osteoarthritis:
Flashcards
Osteoarthritis of the Hip
Osteoarthritis of the Hip
A common condition affecting the hip joint, where articular cartilage breaks down due to wear and tear.
Pain Pattern in Osteoarthritis of the Hip
Pain Pattern in Osteoarthritis of the Hip
Pain in the groin and thigh that spreads towards the buttocks or knee, especially when the hip is used for a long time or in an awkward position.
Patrick's or FABER Test
Patrick's or FABER Test
A physical exam test to differentiate hip pain from lower back pain. It involves flexing, abducting and externally rotating the hip joint.
Hip Internal Rotation Limitation
Hip Internal Rotation Limitation
Signup and view all the flashcards
Risk Factors for Hip Osteoarthritis
Risk Factors for Hip Osteoarthritis
Signup and view all the flashcards
Study Notes
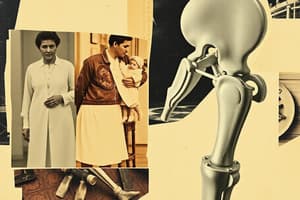
Hip Arthroplasty
- Hip arthroplasty is a surgical procedure to replace damaged hip joint surfaces with prosthetics
- The procedure is used to correct joint damage from conditions like osteoarthritis, rheumatoid arthritis, and avascular necrosis
- It's also used for congenital hip dislocations and certain femur fractures where open reduction isn't suitable
Hip Pain Patterns
- Pain location is used to help determine the source of hip pain (e.g., groin, trochanter, gluteal, low back, posterior thigh, or lateral thigh)
- Frequency percentages for different pain locations can vary
Differentiating Hip from Lumbar Pain
- Physical examination is key: observe for limp, groin pain, limited hip medial rotation, specific hip capsular movement patterns (e.g., medial rotation, abduction, flexion) and a positive “sign of the buttock.”
Osteoarthritis
- Osteoarthritis is the most common form of hip arthritis, often due to wear and tear of the articular cartilage leading to joint space loss
- Risk factors include advancing age, obesity, and prior hip damage/injury
- Symptoms can include pain in the groin/thigh radiating to the buttocks or knee, worsened by prolonged hip loading, cold weather, or certain movements
- In addition, a patient’s internal hip rotation may be less than 15 degrees, hip flexion may be less than 115 degrees, as well as morning stiffness less than 1 hour
Evaluation
- Pain in the groin/thigh radiating to the buttocks or knee gets worse when the hip is loaded, prolonged, and/or cold
- Positive Patrick's or FABER test (flexion, abduction, external rotation of the hip are indicative of hip problems)
- Limited internal hip rotation (under 15°), hip flexion less than 115°, and morning stiffness less than 1 hour
- Presence of osteophytes (bone spurs) on X-rays also suggests osteoarthritis
- Joint space narrowing visible on X-rays
Management
- Medical management focuses on treating symptoms:
- Patient education (especially in primary healthcare).
- Muscle strengthening
- Weight loss
- Avoiding high-impact activities
- Minimizing pain-aggravating activities
- Drugs like NSAIDs or corticosteroids (intra-articular injections)
- Total hip replacements are done in end-stage hip osteoarthritis
Total Hip Arthroplasty (THA)
- THA is a surgical procedure to replace both hip joint surfaces
- Indications: osteoarthritis, rheumatoid arthritis, avascular necrosis, congenital hip dislocations and/or dysplasia, and certain fractured femurs needing non-open reduction internal fixation (mostly displaced neck of femur fractures)
Contraindications
- Inadequate bone mass
- Severe medical risk factors
- Signs of hip infection
- Lack of patient motivation for precautions, rehab exercises, and follow up
Surgical Procedures
- The metal and plastic cup is fitted in the hip socket and new metal stem into the femur to replace damaged areas.
Prosthetics
- There are different types of hip implants
- Non-cemented prosthetics are more expensive, best for younger, active patients, and easier to replace when necessary
- Cemented prosthetics offer immediate weight support after surgery
- Hybrid prosthetics provide a mix of cemented and non-cemented components
Surgical Approaches
- Posterolateral approach (Gibson): accesses the hip between the gluteus maximus and medius muscles, preserving those and adjacent muscles for faster recovery and gait normalization.
- Anterolateral approach (Watson-Jones): uses the interval between the gluteus medius and tensor fascia lata muscles, offering better visibility and less risk of posterior dislocation; and may have less damage to hip musculature due to preserving muscle attachments
Complications
- Dislocation (less frequent in anterior approaches than posterolateral approaches)
- Abductor insufficiency (often after anterior approaches)
- Nerve injury (sciatic, superior gluteal, femoral, specific to the surgical approach)
- Wound infection
- Deep vein thrombosis (blood clots)
- Pulmonary emboli
- Leg length discrepancy
Postoperative Considerations
- Sleeping with a pillow between your legs to prevent dislocation
- Avoid crossing your legs, and 90° precaution for hip flexion/adduction/internal rotation
- Post-operative physical therapy and exercises like ankle pumps, heel slides, gluteal sets, isometric hip abductions, and quadriceps sets are crucial for a faster recovery in the hospital setting
Phase I (Preoperative Training):
- Focuses on teaching safe transfers and postoperative exercises/mobility before surgery to reduce post-operative hip dislocations
Phase IIa (Hospital):
- Goals include preventing complications, improving muscle control, and teaching THR precautions before moving on to a new phase
Phase IIb (Pre-Discharge):
- Goals include promoting transfers, gait independence and ensuring patient is comfortable to be discharged home
Phase III (Return Home):
- Focuses on evaluating the patient's home safety, planning return to work/community activities, and ensuring independence with transfers, exercises, gait, and stairs
- Key components of the prescription include exercises (such as the ones listed above), gait training, and bed mobility, and transfer training
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.