Podcast
Questions and Answers
Cal é un dos factores de risco principais para a infección por virus zoster?
Cal é un dos factores de risco principais para a infección por virus zoster?
- Idade superior a 60 anos (correct)
- Sexo masculino
- Idade inferior a 30 anos
- Episodios previos de herpes simples
Que tipo de vacina é o Zostavax?
Que tipo de vacina é o Zostavax?
- Vacina sintética
- Vacina viva atenuada (correct)
- Vacina recombinante
- Vacina inactivada
Cal é un dos tratamentos recomendados para a dor asociada ao virus zoster?
Cal é un dos tratamentos recomendados para a dor asociada ao virus zoster?
- Antibióticos
- Esteroides orais
- Antihistamínicos
- Antidepresivos tricíclicos (correct)
Cando debería derivarse a un paciente a un oftalmólogo en relación ao virus zoster?
Cando debería derivarse a un paciente a un oftalmólogo en relación ao virus zoster?
Cal é a función dos parches de lidocaína 5% no tratamento do herpes zoster?
Cal é a función dos parches de lidocaína 5% no tratamento do herpes zoster?
Que antibiótico endovenoso é recomendado para o tratamento de MRSA?
Que antibiótico endovenoso é recomendado para o tratamento de MRSA?
Cal é a principal característica da foliculite profunda?
Cal é a principal característica da foliculite profunda?
Cales son os antibióticos tópicos recomendados para a foliculite?
Cales son os antibióticos tópicos recomendados para a foliculite?
Que patoloxía non forma parte do diagnóstico diferencial mencionado?
Que patoloxía non forma parte do diagnóstico diferencial mencionado?
Cal é a principal medida para corrigir a foliculite?
Cal é a principal medida para corrigir a foliculite?
Que bacteria é responsable do impetigo vulgar?
Que bacteria é responsable do impetigo vulgar?
Cal é a localización máis frecuente do impetigo ampollar?
Cal é a localización máis frecuente do impetigo ampollar?
Que tipo de lesión cutánea é característico do impetigo vulgar?
Que tipo de lesión cutánea é característico do impetigo vulgar?
Cal é o tratamento tópico recomendado para o impetigo?
Cal é o tratamento tópico recomendado para o impetigo?
Que sinal clínico indica a presenza do síndrome de pel escaldada estafilocócica (SPEE)?
Que sinal clínico indica a presenza do síndrome de pel escaldada estafilocócica (SPEE)?
Cal é un dos antibióticos sistémicos indicados para pacientes alérxicos á penicilina?
Cal é un dos antibióticos sistémicos indicados para pacientes alérxicos á penicilina?
Que condición cutánea pode aparecer como consecuencia da difusión da toxina epidermolítica en impetigo ampollar?
Que condición cutánea pode aparecer como consecuencia da difusión da toxina epidermolítica en impetigo ampollar?
Cal é o tratamento adecuado para o eccema en casos graves?
Cal é o tratamento adecuado para o eccema en casos graves?
Cal é a característica das ampollas en impetigo ampollar?
Cal é a característica das ampollas en impetigo ampollar?
Que factores predispoñen á infección por S. aureus?
Que factores predispoñen á infección por S. aureus?
Onde é máis común a localización das infeccións por S. aureus?
Onde é máis común a localización das infeccións por S. aureus?
Que tipo de tratamento é indicado para o ectima asociado a unha úlcera crónica?
Que tipo de tratamento é indicado para o ectima asociado a unha úlcera crónica?
Que carácter ten a lesión na erisipela en comparación coa celulite?
Que carácter ten a lesión na erisipela en comparación coa celulite?
Que síntomas clínicos son característicos desta infección por estreptococos do grupo A?
Que síntomas clínicos son característicos desta infección por estreptococos do grupo A?
Que tratamento é recomendado para casos graves de infección por estreptococos do grupo A?
Que tratamento é recomendado para casos graves de infección por estreptococos do grupo A?
Cales son as características da placa eritematosa asociada a esta infección?
Cales son as características da placa eritematosa asociada a esta infección?
Que antibiótico pode usarse como alternativa se o paciente é alérxico á penicilina?
Que antibiótico pode usarse como alternativa se o paciente é alérxico á penicilina?
Cal é a semellanza entre a erisipela e a celulitis?
Cal é a semellanza entre a erisipela e a celulitis?
Que características distinguen a erisipela da celulitis?
Que características distinguen a erisipela da celulitis?
Cal é a duración típica do tratamento antibiótico sistémico para esta infección?
Cal é a duración típica do tratamento antibiótico sistémico para esta infección?
Cual destes organismos é menos probable que cause infección por estreptococos do grupo A?
Cual destes organismos é menos probable que cause infección por estreptococos do grupo A?
Flashcards are hidden until you start studying
Study Notes
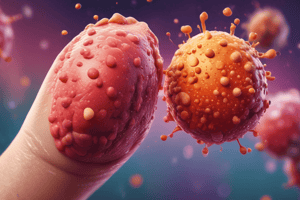
Herpes Zoster (Shingles)
-
Risk Factors:
- Age (50% over 60 years old)
- Female sex
- Prodromal pain
- Severe pain
- Severe, disseminated rash
-
Treatment:
- General: Loose cotton clothing, maintain social activities
- Tricyclic antidepressants
- Gabapentin/Pregabalin
- Opioids
- Lidocaine 5% patches
- Referral to pain specialists
-
Prevention and Referral:
- Zostavax Vaccine: Live attenuated virus, more concentrated than varicela vaccine
- Shingrix Vaccine: Recombinant zoster virus
- No longer in use
- Can be given to immunosuppressed individuals
- Referral necessary for:
- Patients over 500 years old
- More than 1 dermatome
- Hemorrhagic or necrotic lesions
- Involvement of the ophthalmic branch (refer to ophthalmologist, leave ointment)
- Disseminated lesions
- Immunocompromised patients
Impetigo Vulgar
- Caused by: Staphylococcus aureus and Streptococcus pyogenes
- Commonly seen in: Exposed areas (face), periorificial (around the mouth and nose)
- Stages:
- Erythematous macula (red spot)
- Vesicle (small fluid filled blister)
- Pustule (pimple with pus)
- Erosion (loss of surface tissue)
- Characteristics: Superficial, covered with a yellowish crust (honey-like)
- Differential Diagnosis: Herpes simplex, eczema, insect bites, varicella (chickenpox)
Treatment for Impetigo Vulgar
- Local care: Cleansing and crust removal
- Topical Antibiotics:
- Mupirocin 2% 3 times a day
- Fusidic acid 2% twice a day for 1 week
- Chloramphenicol
- Systemic Antibiotics:
- First-generation cephalosporin (Cefadroxil) 30 mg/kg/day divided every 12 hours for 10 days
- Flucloxacillin 50 mg/kg/day divided every 8 hours
- Penicillin allergy:
- Erythromycin 30-50 mg/kg/day divided every 6 hours
- Azithromycin 10 mg/kg/day for 5 days
Impetigo Bullosa (Bulla)
-
More common in: Skin folds. Frequent in young children.
-
Caused by: Staphylococcus aureus
-
Commonly seen in: Face and body. Seen in infants and newborns, especially in diaper areas.
-
Characteristics:
- Vesicles rapidly change into flaccid, transparent blisters (bullae).
- Blisters have sharp margins with no erythematous halo.
- Blisters are surrounded by scales.
- Blisters rupture easily, leaving a dry, shiny erosion, covered with a thin crust.
- Heals faster than Impetigo Vulgar.
-
Complications: If epidermolytic toxin spreads hematogenously, it can lead to Staphylococcal Scalded Skin Syndrome (SSSS), a generalized form of bullous impetigo.
SSSS (Staphylococcal Scalded Skin Syndrome)
- Signs and Symptoms:
- General malaise: Sudden onset, irritability, and fever
- Macular erythema: Begins on the face (periorificial) and in skin folds
- Sensitive skin
- Generalized rash
- Nikolsky Sign (positive): Skin peels off with gentle friction
- Wrinkled skin
- 24-48 hours: Flaccid blisters appear, detach, and leave large erosive areas.
- Erosive areas become moist, then dry and form a thin crust.
- Desquamation (shedding skin) occurs in 3-5 days, involving hands, feet, and perineum.
- Perioral crusts and fissures: Indicates keratinocyte necrosis.
SSSS Treatment
- Eradicate infectious focus:
- Intravenous antibiotics (Cloxacillin, Vancomycin if MRSA)
- Skin and fluid electrolyte management
- Diagnose and manage carriers (Mupirocin nasal ointment)
SSSS Differential Diagnosis
- Scarlet fever
- Kawasaki disease
- Staphylococcal toxic shock syndrome
- TEN: Toxic Epidermal Necrolysis (caused by medications)
Folliculitis
-
Superficial Folliculitis:
- Location: Distal portion of the hair follicle.
- Appearance: Papules or pustules (1-4 mm diameter)on an erythematous base.
- Symptoms: Pruritis (itchiness)
-
Deep Folliculitis:
- Location: Extends to surrounding tissue
- Appearance: Erythematous, sensitive papules, larger in size with central pustules
- Possible complications: Can progress to furuncle (boil)
Folliculitis Differential Diagnosis
- Treatment:
- Address predisposing factors.
- Wash with antibacterial soaps (Triclosan or Chlorhexidine 1%)
- Topical antibiotics:
- Mupirocin 2%
- Fusidic acid for 7-10 days
- Oral antibiotics:
- Flucloxacillin (for extensive, resistant, or recurrent cases)
Abscess, Furuncle, Anthrax
- Abscess: Occurs in any area.
- Furuncle: Involves the hair follicle.
- Anthrax: Multiple furuncles.
Furuncle
- Commonly seen in: Adolescents and young adults.
- Caused by: S. aureus. Anaerobic bacteria can be present in the groin.
- Most commonly affected areas: Areas of friction (face, neck (nape), axillae, buttocks, thighs, and perineum)
- Predisposing factors: S. aureus carriage, diabetes, obesity, immunosuppression, tight clothing, hyperhidrosis, poor hygiene.
Anthrax
- Involves: Subcutaneous tissue.
- Appearance: Firm swelling with multiple drainage points on the surface.
- Commonly seen in: The nape, back, and thighs.
- Signs and Symptoms: Cervical lymphadenopathy (swollen lymph nodes in the neck), pain.
- Complications: Scarring.
- Increased risk in: Diabetes.
Furuncle/Anthrax Treatment
- Local heat and drainage.
- Systemic antibiotics:
- Cloxacillin or Flucloxacillin
- First-generation cephalosporin
- Amoxicillin-clavulanate
- Penicillin allergy: Macrolides/Clindamycin
Ecthyma
- Ulcerative form of non-bullous impetigo.
- Involves: Epidermis and dermis.
- Commonly seen in: Lower extremities (dorsum of feet and anterior legs)
- Characteristic: Few lesions.
- Treatment:
- Localized:
- Macrolides or Clindamycin
- Severe or Facial: Hospitalization and intravenous antibiotics
- Penicillin sodium 2-4 million units every 6 hours + Cloxacillin 1 g every 6 hours
- or
- First-generation cephalosporin (Cefazolin) 1-2 g every 8 hours
- After 72 hours of good response: Cefadroxil 1 g every 12 hours (orally)
- Penicillin allergy: Lincomycin intravenously, then orally
- Chronic Ulcers:
- Cover anaerobic and gram-negative bacteria
- Metronidazole + Ciprofloxacin
- Recurrences:
- Benzathine penicillin 1.2 million units monthly for 6 months
- Erythromycin 250 mg every 12 hours for 3 months.
- Localized:
Erysipelas
- Infections of the dermis and superficial lymphatic plexus.
- Superficial to Cellulitis.
- Caused by: Streptococcus pyogenes (beta-hemolytic group A), less frequently by S. aureus, S. pneumoniae, and H. influenzae.
- Clinical Presentation:
- Acute onset: Fever, chills, and cervical lymphadenopathy.
- Appearance: Erythematous, shiny, edematous, hot, and tender plaque that spreads rapidly.
- "Orange-peel skin".
- Edges: Well defined and palpable (unlike cellulitis, which has diffuse, non-palpable edges).
- May have vesicles, blisters, bullae, pustules, or superficial purpuric lesions.
Erysipelas Treatment
- Systemic antibiotics for 10 days:
- Flucloxacillin or Cefadroxil
- Penicillin allergy: Macrolides or Clindamycin
- Severe or Facial: Hospitalization and intravenous antibiotics
- Penicillin sodium 2-4 million units every 6 hours
- No response after 48 hours: Add Cloxacillin
- First-generation cephalosporin 1-2 g every 8 hours
- Favorable response after 72 hours: Cefadroxil 1 g every 12 hours orally
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.