Podcast
Questions and Answers
What is the primary function of the gallbladder?
What is the primary function of the gallbladder?
- To concentrate and store bile. (correct)
- To secrete insulin.
- To produce bile.
- To filter bilirubin.
Which type of bilirubin is water-soluble and can be excreted in bile?
Which type of bilirubin is water-soluble and can be excreted in bile?
- Bilirubinogen.
- Unconjugated bilirubin.
- Indirect bilirubin.
- Conjugated bilirubin. (correct)
Which of the following cell types produces insulin?
Which of the following cell types produces insulin?
- Alpha cells.
- Delta cells.
- Beta cells. (correct)
- Acini cells.
What gives stool its characteristic brown color?
What gives stool its characteristic brown color?
Which of the following is NOT a component of the biliary tract?
Which of the following is NOT a component of the biliary tract?
What is the primary cause of Crigler-Najjar syndrome?
What is the primary cause of Crigler-Najjar syndrome?
Which of the following is a consequence of excessive accumulation of bilirubin in the brain?
Which of the following is a consequence of excessive accumulation of bilirubin in the brain?
Besides explaining the procedure to the patient, what else mentioned is a nursing responsibility regarding to liver biopsy?
Besides explaining the procedure to the patient, what else mentioned is a nursing responsibility regarding to liver biopsy?
A patient's liver function tests reveal elevated levels of AST and ALT, while total and direct bilirubin levels are within normal limits. Which condition is LEAST likely to be the primary cause of these results, assuming the trends are consistent and persistent?
A patient's liver function tests reveal elevated levels of AST and ALT, while total and direct bilirubin levels are within normal limits. Which condition is LEAST likely to be the primary cause of these results, assuming the trends are consistent and persistent?
A researcher is investigating novel treatments for Crigler-Najjar syndrome. Which of the following therapeutic approaches would be the MOST direct and theoretically effective in addressing the underlying cause of the disease, considering current understanding?
A researcher is investigating novel treatments for Crigler-Najjar syndrome. Which of the following therapeutic approaches would be the MOST direct and theoretically effective in addressing the underlying cause of the disease, considering current understanding?
Which structure transports bile out of the liver?
Which structure transports bile out of the liver?
What is the approximate weight of the liver in an average adult?
What is the approximate weight of the liver in an average adult?
The conversion of amino acids and fatty acids to glucose by the liver is known as:
The conversion of amino acids and fatty acids to glucose by the liver is known as:
Which of the following vitamins is NOT stored in the liver?
Which of the following vitamins is NOT stored in the liver?
The liver's detoxification process primarily involves:
The liver's detoxification process primarily involves:
What is the end-product of the breakdown of hemoglobin that the liver processes?
What is the end-product of the breakdown of hemoglobin that the liver processes?
Which of the following metabolic functions is NOT performed by the liver?
Which of the following metabolic functions is NOT performed by the liver?
What is the collective name for the phagocytic cells contained in the hepatic sinusoids that remove foreign particles from blood?
What is the collective name for the phagocytic cells contained in the hepatic sinusoids that remove foreign particles from blood?
If the liver excretes approximately 1 liter of bile per day, and assuming that the rate of bile excretion is constant, approximately how many $\text{cm}^3$ of bile would the liver excrete in 1 hour? (Note: 1 liter = 1000 $\text{cm}^3$)
If the liver excretes approximately 1 liter of bile per day, and assuming that the rate of bile excretion is constant, approximately how many $\text{cm}^3$ of bile would the liver excrete in 1 hour? (Note: 1 liter = 1000 $\text{cm}^3$)
A patient presents with ascites, jaundice, and elevated ammonia levels. Based on your understanding of liver function, which of the following impaired hepatic processes is MOST likely contributing to these clinical signs?
A patient presents with ascites, jaundice, and elevated ammonia levels. Based on your understanding of liver function, which of the following impaired hepatic processes is MOST likely contributing to these clinical signs?
Flashcards
Liver
Liver
The largest organ in the body, weighing about 3 lbs in adults and located under the diaphragm.
Hepatic Sinusoids Function
Hepatic Sinusoids Function
Phagocytic cells in the liver that remove foreign particles from the blood.
Hepatic Duct
Hepatic Duct
The duct that transports bile out of the liver.
Common Hepatic Duct
Common Hepatic Duct
Signup and view all the flashcards
Cystic Duct
Cystic Duct
Signup and view all the flashcards
Common Bile Duct
Common Bile Duct
Signup and view all the flashcards
Gluconeogenesis
Gluconeogenesis
Signup and view all the flashcards
Glycogenesis
Glycogenesis
Signup and view all the flashcards
Glycogenolysis
Glycogenolysis
Signup and view all the flashcards
Bilirubin
Bilirubin
Signup and view all the flashcards
Jaundice
Jaundice
Signup and view all the flashcards
Icterus
Icterus
Signup and view all the flashcards
Kernicterus
Kernicterus
Signup and view all the flashcards
Crigler-Najjar Syndrome
Crigler-Najjar Syndrome
Signup and view all the flashcards
Gallbladder Function
Gallbladder Function
Signup and view all the flashcards
Gallbladder
Gallbladder
Signup and view all the flashcards
Acini Cells
Acini Cells
Signup and view all the flashcards
Islets of Langerhans
Islets of Langerhans
Signup and view all the flashcards
Liver Function Tests (LFTs)
Liver Function Tests (LFTs)
Signup and view all the flashcards
Liver Biopsy
Liver Biopsy
Signup and view all the flashcards
Study Notes
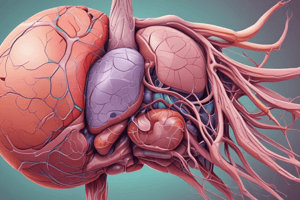
Hepatobiliary-Pancreatic system overview
- The hepatobiliary-pancreatic system includes the liver, biliary tract, and pancreas.
Hepatic system - Liver
- The liver weighs approximately 3 lbs (1.37 kg) in an adult.
- The liver is the largest organ in the body.
- The liver is located directly beneath the diaphragm at the right epigastric region.
- The falciform ligament divides the liver into two lobes, where the right lobe is larger.
- The liver can repair itself and regenerate damaged tissue to a certain extent.
- Hepatic sinusoids contain phagocytic cells to remove foreign particles from the blood.
- The central vein is at the center of each lobule.
- Mixed blood flows toward the central vein, forming hepatic veins.
Liver Ducts
- Hepatic ducts transport bile out of the liver.
- The common hepatic duct is formed from the left and right hepatic ducts.
- The cystic duct joins the common hepatic duct, and originates from the gallbladder.
- The common bile duct is formed from the common hepatic duct and cystic duct.
Major Functions of the Liver
- Metabolic functions include carbohydrate, protein, and fat metabolism, detoxification, and steroid metabolism.
- In carbohydrate metabolism, the liver converts amino acids and fatty acids to glucose through gluconeogenesis.
- Glycogenesis, or glycogen synthesis, is the conversion of glucose to glycogen.
- Glycogenolysis, or glycogen hydrolysis, is the process of breaking down glycogen into glucose.
- In protein metabolism, the liver converts NH3 ammonia to urea.
- In fat metabolism, the liver synthesizes fatty acids from amino acids and glucose.
- The liver breaks down triglycerides.
- Detoxification involves inactivation of drugs and harmful substances.
- Steroid metabolism involves excretion of gonadal and adrenal corticosteroid.
- Bile synthesis happens through bile production by hepatocytes.
- The liver excretes about 1 L of bile per day.
- Storage: The liver stores glucose in the form of glycogen, and Vitamins A, D, E, and K.
- Phagocytic system: The liver breaks down RBCs, WBCs, and bacteria.
- The liver breaks down hemoglobin to bilirubin.
Bilirubin Metabolism
- Bilirubin is a waste product of the breakdown of the hemoglobin molecule.
- Aged RBC-> Hemoglobin -> Heme and Globin
- Bilirubin (insoluble) -> Attached to albumin -> Unconjugated bilirubin (indirect bilirubin) - insoluble
- Liver -> Unconjugated bilirubin combines with glucuronic acid (glucuronide) -> Conjugated bilirubin (direct bilirubin) – soluble
- Excreted in the bile -> Intestine (bilirubin reduced to urobilinogen and stercobilinogen by intestinal bacteria)
- Stercobilinogen gives brown color to stool
- Urobilinogen goes in systemic circulation and excreted in urine
Bilirubin Disorders
- Jaundice is the yellow pigmentation of the skin and sclera.
- Icterus is the yellow coloration in the sclera of the eye.
- Kernicterus is excessive accumulation of bilirubin in the brain that causes brain damage.
- Crigler-Najjar disease is a recessive inherited disorder characterized by the inability to conjugate bilirubin.
- The Crigler-Najjar disease leads to severe neurological impairments, and these patients have a life expectancy of one year or less.
Biliary Tract
- The biliary tract is composed of the gallbladder, common bile duct, cystic duct, and hepatic duct that drain bile.
- The gallbladder is a pear-shaped sac located below the liver.
- The gallbladder concentrates and stores bile.
- It can hold approximately 40 – 70 ml of bile.
Pancreas
- The pancreas is a long, thin glandular organ essential for digestion and metabolism.
- There are two major cell types: Exocrine and Endocrine
- Exocrine cells
- Acini cells produce pancreatic enzymes.
- Endocrine cells - Islets of Langerhans.
- Alpha cells produce glucagon.
- Beta cells produce insulin.
- Delta cells produce somatostatin.
Diagnostic Tests
- Liver Function Tests (LFT) include Albumin, total and direct bilirubin, alkaline phosphatase, Aspartate Transaminase (AST) / Serum Glutamic-Oxaloacetic Transaminase (SGOT), and Alanine Aminotransferase (ALT) / Serum Glutamic Pyruvic Transaminase (SGPT).
- A Liver biopsy procures a small sample of liver tissue to diagnose liver pathology. It is an invasive sterile procedure, performed under local anesthesia.
Nursing Responsibilities for Liver Biopsy
- Explain the procedure to the patient
- Place the patient on NPO for 12 hours prior to biopsy
- Ensure that prothrombin and hemoglobin results are available
Potential Complications for Liver Biopsy
- Bleeding, puncture of the kidney or intestine, puncture of the lungs with subsequent pneumothorax, puncture of the gallbladder, and peritonitis are potential complications of a liver biopsy.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
- The ERCP visually and radiographically inspects the liver, gallbladder, and pancreas.
- A fiberoptic duodenoscope is inserted orally under general anesthesia into the duodenum.
- Radiographic dye is introduced to visualize the liver, gallbladder, pancreas, and the different ducts.
Potential Complications for ERCP
- A perforation of the stomach, duodenum and other ducts, pancreatitis, an anaphylactic reaction to the contrast dye, aspiration of gastric contents, or a reaction to anesthesia are potential complications of ERCP.
Nursing Responsibilities for ERCP
- Confirm the signed consent form.
- Ensure a patent IV line
- Check that X-rays are available
- Keep the patient NPO for 12 hours before procedure.
- After the test: NPO until gag reflex returns.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.