Podcast
Questions and Answers
What percentage of liver function is required to sustain life?
What percentage of liver function is required to sustain life?
- 50%
- 10% to 20% (correct)
- 30%
- 80%
How many tasks does the liver perform?
How many tasks does the liver perform?
- More than 500 (correct)
- 100
- 200
- 1000
What is the function of the hepatic duct?
What is the function of the hepatic duct?
- To transport bile produced by the liver cells to the gallbladder and duodenum (correct)
- To store bile
- To supply oxygenated blood to the liver
- To filter nutrient-rich blood from the intestine
What is the relative size of the right lobe to the left lobe of the liver?
What is the relative size of the right lobe to the left lobe of the liver?
How much blood circulates through the liver every minute?
How much blood circulates through the liver every minute?
What are the two sources of blood supply to the liver?
What are the two sources of blood supply to the liver?
What happens to bilirubin in the liver?
What happens to bilirubin in the liver?
What does an increase in unconjugated bilirubin indicate?
What does an increase in unconjugated bilirubin indicate?
What is the name of the test that measures conjugated bilirubin?
What is the name of the test that measures conjugated bilirubin?
What is the characteristic of fulminant hepatitis?
What is the characteristic of fulminant hepatitis?
What is the duration of chronic hepatitis?
What is the duration of chronic hepatitis?
What is the main mode of transmission of hepatitis A and E?
What is the main mode of transmission of hepatitis A and E?
What are the four phases of acute viral hepatitis?
What are the four phases of acute viral hepatitis?
What is the complication of fulminant hepatitis?
What is the complication of fulminant hepatitis?
What is a characteristic of severe advanced liver disease?
What is a characteristic of severe advanced liver disease?
What is the accumulation of fat droplets in hepatocytes likely to lead to?
What is the accumulation of fat droplets in hepatocytes likely to lead to?
What is Non-Alcoholic Fatty Liver Disease (NAFLD) characterized by?
What is Non-Alcoholic Fatty Liver Disease (NAFLD) characterized by?
What is the major route of oxidation of alcohol?
What is the major route of oxidation of alcohol?
What is the result of the formation of lactic acid in the liver?
What is the result of the formation of lactic acid in the liver?
What is the characteristic of Alcoholic Hepatitis?
What is the characteristic of Alcoholic Hepatitis?
What is the main treatment for Alcoholic Hepatitis?
What is the main treatment for Alcoholic Hepatitis?
What is the result of the increase in NADH in the liver?
What is the result of the increase in NADH in the liver?
What is the primary reason for using MCTs in the treatment of pancreatic disorders?
What is the primary reason for using MCTs in the treatment of pancreatic disorders?
What is the primary goal of medical nutrition therapy (MNT) in chronic pancreatitis?
What is the primary goal of medical nutrition therapy (MNT) in chronic pancreatitis?
What is the characteristic of severe acute pancreatitis (AP)?
What is the characteristic of severe acute pancreatitis (AP)?
What is the recommended treatment for steatorrhea in patients with pancreatic disorders?
What is the recommended treatment for steatorrhea in patients with pancreatic disorders?
What is the characteristic of hepatorenal syndrome?
What is the characteristic of hepatorenal syndrome?
What is the recommended nutrition approach for patients with mild to moderate acute pancreatitis?
What is the recommended nutrition approach for patients with mild to moderate acute pancreatitis?
What is the primary purpose of lactulose in the treatment of hepatic encephalopathy?
What is the primary purpose of lactulose in the treatment of hepatic encephalopathy?
What is the main contribution of branched-chain amino acids to the body?
What is the main contribution of branched-chain amino acids to the body?
What is the result of muscle proteolysis in ESLD?
What is the result of muscle proteolysis in ESLD?
What is the effect of high levels of aromatic amino acids on the brain?
What is the effect of high levels of aromatic amino acids on the brain?
What percentage of patients with cirrhosis can tolerate mixed-protein diets up to 1.5 g/kg of body weight?
What percentage of patients with cirrhosis can tolerate mixed-protein diets up to 1.5 g/kg of body weight?
What is the role of rifaximin in the treatment of hepatic encephalopathy?
What is the role of rifaximin in the treatment of hepatic encephalopathy?
What is the effect of the altered plasma amino acid ratio on the development of hepatic encephalopathy?
What is the effect of the altered plasma amino acid ratio on the development of hepatic encephalopathy?
What is another suggested mechanism that contributes to neuronal inhibition in hepatic encephalopathy?
What is another suggested mechanism that contributes to neuronal inhibition in hepatic encephalopathy?
Flashcards are hidden until you start studying
Study Notes
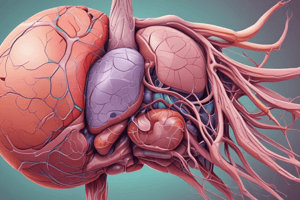
Structure of the Liver
- The liver is the largest gland in the body, divided into right and left lobes.
- 1500 mL of blood/min circulates through the liver and exits via the hepatic veins into the inferior vena cava.
- Bile is formed in the liver and exits through a system of ducts.
Physiology and Functions of the Liver
- The liver is integral to most body functions, performing over 500 tasks.
- The liver has the ability to regenerate, but only 10% to 20% of its function is needed to sustain life.
The Liver
- The right lobe is 6 times the size of the left lobe.
- Both lobes are made up of thousands of lobules connected to small ducts that form the hepatic duct.
- The hepatic duct transports bile produced by liver cells to the gallbladder and duodenum.
- The liver has two blood supplies: the hepatic artery, which provides oxygenated blood, and the hepatic portal vein, which provides nutrient-rich blood from the intestine.
Bile Production
- The liver produces bile, which is then stored in the gallbladder and transported to the duodenum through the biliary tract.
- Bilirubin is conjugated with glucoronic acid in the liver and then excreted in bile.
- Increased levels of bilirubin indicate liver disease.
Diseases of the Liver
- Acute viral hepatitis: widespread inflammation caused by viruses A, B, C, D, E, and G.
- Fulminant hepatitis: severe liver dysfunction accompanied by hepatic encephalopathy.
- Chronic hepatitis: lasting at least 6 months, caused by auto-immune, viral, metabolic, or medicine-induced factors.
- Non-alcoholic steatohepatitis (NASH): accumulation of fat droplets in hepatocytes leading to fibrosis and cirrhosis.
- Alcoholic liver disease: caused by alcohol metabolism, leading to fatty liver, alcoholic hepatitis, and cirrhosis.
Acute Viral Hepatitis
- Symptoms are divided into 4 phases: prodromal, preicteric, icteric, and convalescent.
- Viruses A and E are spread orally, while B, C, and D are spread through blood and body fluids.
Fulminant Hepatitis
- Defined by the absence of existing liver disease, with viral hepatitis accounting for 75% of cases.
- Complications include cerebral edema, coagulopathy, renal failure, and electrolyte imbalances.
Chronic Hepatitis
- Characterized by fatigue, sleep disturbances, difficulty concentrating, and right upper quadrant pain.
- Advanced disease is marked by jaundice, muscle wasting, edema, ascites, and encephalopathy.
Non-Alcoholic Fatty Liver Disease
- Accumulation of fat droplets in hepatocytes leads to fibrosis and cirrhosis.
- May be caused by inborn errors of metabolism, diabetes, obesity, or lipodystrophy.
Alcoholic Liver Disease
- Metabolism of alcohol leads to fatty acid accumulation, causing fatty liver and hyperlipidemia.
- Acetaldehyde causes cell membrane damage and necrosis.
- NADH replaces fatty acid as a fuel, promoting triglyceride accumulation.
Hepatic Encephalopathy
- Lactulose and rifaximin are used to treat encephalopathy by reducing ammonia production in the gut.
- Other hypotheses suggest the role of GABA receptors, altered neurotransmitters, and branched-chain amino acid imbalance in the development of encephalopathy.
Renal Insufficiency and Hepatorenal Syndrome
- Renal failure due to severe liver disease, characterized by low urine sodium levels.
- Treatment involves dextrose-based solutions, somatostatin, and H2 receptor antagonists.
Chronic Pancreatitis
- Recurrent attacks of epigastric pain, precipitated by meals, accompanied by nausea, vomiting, and diarrhea.
- Treatment involves avoiding large meals and alcohol, pancreatic enzyme replacement, and medium-chain triglycerides.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.