Podcast
Questions and Answers
What is the normal pathway of blood flow from the spleen, small intestines, pancreas, and stomach?
What is the normal pathway of blood flow from the spleen, small intestines, pancreas, and stomach?
- Portal vein to hepatic sinusoids to caudal vena cava (correct)
- Systemic circulation to portal vein to hepatic sinusoids
- Hepatic sinusoids to portal vein to caudal vena cava
- Caudal vena cava to portal vein to hepatic sinusoids
What is the function of the ductus venosus in the fetal liver?
What is the function of the ductus venosus in the fetal liver?
- To increase oxygenation of the liver
- To bypass hepatic circulation and direct blood to the caudal vena cava (correct)
- To decrease blood flow to the liver
- To increase hepatic metabolism and detoxification
What is the result if the ductus venosus remains patent after birth?
What is the result if the ductus venosus remains patent after birth?
- Portosystemic shunt (correct)
- Decreased hepatic function
- Patent subhepatic shunt
- Increased hepatic function
What is the clinical sign associated with the origin of blood bypassing the liver in PSS?
What is the clinical sign associated with the origin of blood bypassing the liver in PSS?
How does the portal vein branch in the dog?
How does the portal vein branch in the dog?
Where do the portal vein branches eventually empty into?
Where do the portal vein branches eventually empty into?
What is the most common type of portosystemic shunt?
What is the most common type of portosystemic shunt?
Which breed of dog is more commonly associated with intrahepatic portosystemic shunts (IHPSS)?
Which breed of dog is more commonly associated with intrahepatic portosystemic shunts (IHPSS)?
What is the role of bile acids in the small intestine?
What is the role of bile acids in the small intestine?
What is the significance of elevated postprandial bile acids in dogs and cats?
What is the significance of elevated postprandial bile acids in dogs and cats?
What is the cause of persistent bile acid concentration elevations in animals with PSS?
What is the cause of persistent bile acid concentration elevations in animals with PSS?
What is the purpose of measuring 6-hour postprandial blood ammonia concentrations?
What is the purpose of measuring 6-hour postprandial blood ammonia concentrations?
What is the typical characteristic of ascites in animals with PSS?
What is the typical characteristic of ascites in animals with PSS?
What is the common coagulation abnormality in dogs with PSS?
What is the common coagulation abnormality in dogs with PSS?
What is the typical ultrasound finding in animals with EHPSS?
What is the typical ultrasound finding in animals with EHPSS?
What is the gold standard for PSS diagnosis?
What is the gold standard for PSS diagnosis?
What is the significance of protein C levels in differentiating between PSS and MVD?
What is the significance of protein C levels in differentiating between PSS and MVD?
What is the typical histopathological finding in the liver of animals with PSS?
What is the typical histopathological finding in the liver of animals with PSS?
What is the typical history of dogs with PSS?
What is the typical history of dogs with PSS?
Which breed is overrepresented for MVD/PVH?
Which breed is overrepresented for MVD/PVH?
What is the common cause of ascites in HAVM?
What is the common cause of ascites in HAVM?
What is the common complication of PSS in large breed dogs?
What is the common complication of PSS in large breed dogs?
What is the result of defective iron transport mechanism in dogs with PSS?
What is the result of defective iron transport mechanism in dogs with PSS?
What is the common finding in dogs with PSS?
What is the common finding in dogs with PSS?
What is the result of deficient hepatic urea cycle in dogs with PSS?
What is the result of deficient hepatic urea cycle in dogs with PSS?
What is the common site of stones formation in dogs with PSS?
What is the common site of stones formation in dogs with PSS?
What is the common feature of animals with PVH/MVD?
What is the common feature of animals with PVH/MVD?
What is the reason portovenography during laparotomy is not commonly utilized?
What is the reason portovenography during laparotomy is not commonly utilized?
What is the main goal of medical management in dogs with HE?
What is the main goal of medical management in dogs with HE?
What is the effect of lactulose administration in dogs with HE?
What is the effect of lactulose administration in dogs with HE?
Why is Supplement K administration important in dogs with HE?
Why is Supplement K administration important in dogs with HE?
What is the purpose of antibiotic therapy in dogs with HE?
What is the purpose of antibiotic therapy in dogs with HE?
What is the benefit of using milk and vegetable proteins in dogs with HE?
What is the benefit of using milk and vegetable proteins in dogs with HE?
What is the role of SAMe in medical management of dogs with HE?
What is the role of SAMe in medical management of dogs with HE?
What is the goal of surgical management in dogs with PSS?
What is the goal of surgical management in dogs with PSS?
What is a potential complication of complete shunt attenuation?
What is a potential complication of complete shunt attenuation?
What is the reported survival time in dogs with IHPSS medically managed?
What is the reported survival time in dogs with IHPSS medically managed?
What is the reported complication rate following ameroid constrictor placement for EHPSS?
What is the reported complication rate following ameroid constrictor placement for EHPSS?
What is a potential benefit of using ameroid constrictors compared to suture ligation?
What is a potential benefit of using ameroid constrictors compared to suture ligation?
What is a characteristic of cellophane band material?
What is a characteristic of cellophane band material?
What is a potential complication of IHPSS in dogs?
What is a potential complication of IHPSS in dogs?
What is a reported outcome in dogs with incomplete shunt attenuation after ameroid constrictor placement?
What is a reported outcome in dogs with incomplete shunt attenuation after ameroid constrictor placement?
What is a characteristic of HAVM?
What is a characteristic of HAVM?
What is a goal of post-operative care?
What is a goal of post-operative care?
What is a reported outcome in cats following suture ligation for PSS?
What is a reported outcome in cats following suture ligation for PSS?
What is a potential treatment for HAVM?
What is a potential treatment for HAVM?
What is a reported median survival time in dogs following ameroid constrictor placement for EHPSS?
What is a reported median survival time in dogs following ameroid constrictor placement for EHPSS?
Flashcards are hidden until you start studying
Study Notes
Hepatic Vascular Anomalies
Introduction
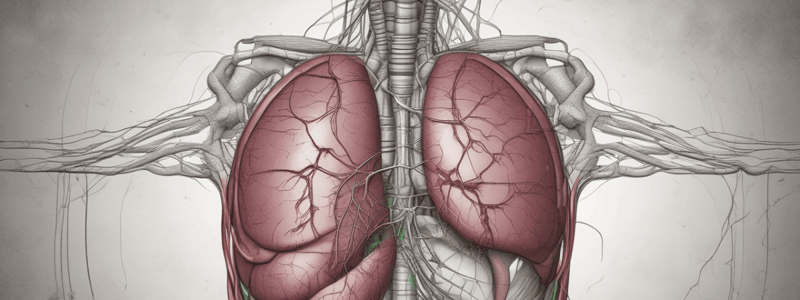
- Hepatic vascular anomalies, such as portosystemic shunts (PSS), connect the portal vein to the systemic circulation, bypassing the hepatic sinusoids.
- Normally, blood from the spleen, small intestines, pancreas, and stomach enters the portal vein, perfuses the liver through the sinusoids, and then drains into the hepatic veins and caudal vena cava.
Anatomy and Classification
- Blood from the GI tract, pancreas, and spleen is drained by respective veins, which empty into the portal vein.
- In dogs, the portal vein enters the liver and branches into left and right branches.
- In cats, there are central, right, and left branches of the portal vein.
- PSS can be classified as congenital intrahepatic or congenital extrahepatic shunts.
- Congenital extrahepatic PSS with a single portocaval shunt are most common (66-75% of shunts).
Clinical Signs
- Clinical signs associated with volume and origin of blood bypassing the liver, including:
- Impaired hepatic function
- Hepatic encephalopathy (HE)
- Chronic GI signs
- Lower urinary signs if stones form
- Coagulopathies
- Delayed growth
Hepatic Encephalopathy (HE)
- Most clinical signs seen with PSS are due to HE.
- HE is caused by the inability of the liver to detoxify ammonia and other toxins.
Evaluation
- Congenital EHPSS are more common in small breeds, such as Yorkies, Pugs, and Havanese.
- IHPSS are more common in large breeds, such as Labradors, Wolfhounds, and Golden Retrievers.
- Common symptoms:
- Failure to thrive
- Polyuria and polydipsia (PU/PD)
- Bizarre behavior due to HE
- GI signs
- Dysuria due to ammonium urate calculi formation
- Ascites in HAVM cases
Clinicopathologic Findings
- Mild to moderate microcytic, normochromic nonregenerative anemia
- Leukocytosis associated with poor clearance of bacterial endotoxin
- Low albumin and BUN levels
- Hypocholesterolemia
- Hypoglycemia
- Elevated ALP and ALT levels
- Hyposthenuric or isosthenuric urine and ammonium biurate crystalluria
Liver Function Tests
- 12-hour fasting and 2-hour postprandial bile acids
- Bile acid levels aid in diagnosing PSS.
Treatment
- Medical management:
- Manage HE with lactulose, oral antibiotics, and protein restriction
- Correct coagulopathies and hypoglycemia
- Supplement potassium and vitamin K
- Surgical management:
- Attenuate the abnormal vessel to reestablish blood flow through the hepatic parenchyma
- Goal is to improve clinical signs and control HE
- Surgery may not be possible in all cases, and medical management may be necessary
Prognosis
- Prognosis is dependent on the type of shunt, severity of clinical signs, and response to treatment.
- In some cases, medical management alone can lead to a good prognosis.
- Surgery can improve outcomes, but complications can occur.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.