Podcast
Questions and Answers
What series of structures will bile salt travel through in order to emulsify fats in the small intestine?
What series of structures will bile salt travel through in order to emulsify fats in the small intestine?
- i, iii, vii, viii (correct)
- ii, iii, vii, viii
- ii, vi, vii, viii
- ii, iv, v, ix
- i, iv, v, viii
What series of structures will blood travel through in order to supply the liver with oxygen and leave the liver with carbon dioxide?
What series of structures will blood travel through in order to supply the liver with oxygen and leave the liver with carbon dioxide?
- ii, iii, vi, vii, ix (correct)
- iii, vi, v, viii, ix
- ii, iii, v, vii, ix
- iii, v, vi, vii, ix
- ii, v, vi, vii, ix
Name the two types of blood circulation that occur in the liver.
Name the two types of blood circulation that occur in the liver.
Hepatic artery and hepatic portal vein
The liver is composed of four lobes.
The liver is composed of four lobes.
What are the two main functions of the hepatocytes?
What are the two main functions of the hepatocytes?
The liver can store glycogen in the fed state.
The liver can store glycogen in the fed state.
The liver can synthesize glucose from noncarbohydrates like amino acids, glycerol, and lactic acid.
The liver can synthesize glucose from noncarbohydrates like amino acids, glycerol, and lactic acid.
The liver can synthesize lipoproteins.
The liver can synthesize lipoproteins.
The liver can synthesize bile.
The liver can synthesize bile.
What is the main function of kupffer cells?
What is the main function of kupffer cells?
The liver is involved in the interconversion of essential amino acids into nonessential amino acids.
The liver is involved in the interconversion of essential amino acids into nonessential amino acids.
The liver converts ammonia into urea
The liver converts ammonia into urea
The liver converts unconjugated bilirubin into conjugated bilirubin.
The liver converts unconjugated bilirubin into conjugated bilirubin.
Cholecalciferol, a steroid intermediary produced by exposure to ultraviolet light is metabolized to vitamin D by the hepatocytes.
Cholecalciferol, a steroid intermediary produced by exposure to ultraviolet light is metabolized to vitamin D by the hepatocytes.
The liver detoxifies toxic medications and compounds absorbed by the Gl tract.
The liver detoxifies toxic medications and compounds absorbed by the Gl tract.
The liver is responsible for the half-life of hormones by breaking them down.
The liver is responsible for the half-life of hormones by breaking them down.
The liver only stores glycogen.
The liver only stores glycogen.
What are the two main characteristics used to assess liver function?
What are the two main characteristics used to assess liver function?
Elevated serum liver enzymes is indicative of liver damage.
Elevated serum liver enzymes is indicative of liver damage.
What are the two enzymes that catalyze the transamination of their respective amino acids?
What are the two enzymes that catalyze the transamination of their respective amino acids?
The half-life of a compound is the amount of time taken to remove half the concentration of a compound from the blood.
The half-life of a compound is the amount of time taken to remove half the concentration of a compound from the blood.
AST and ALT have relatively short half-lifes.
AST and ALT have relatively short half-lifes.
The AST:ALT ratio can help diagnose the condition or stage of liver disease.
The AST:ALT ratio can help diagnose the condition or stage of liver disease.
An AST:ALT ratio below one (<1) is indicative of non-alcoholic fatty liver disease or late-stage viral hepatitis.
An AST:ALT ratio below one (<1) is indicative of non-alcoholic fatty liver disease or late-stage viral hepatitis.
An AST:ALT ratio above two (>2) is indicative of alcohol-related liver damage.
An AST:ALT ratio above two (>2) is indicative of alcohol-related liver damage.
An AST:ALT ratio above five (>5) is indicative of a condition unrelated to the liver, like myocardial infarction or rhabdomyolysis.
An AST:ALT ratio above five (>5) is indicative of a condition unrelated to the liver, like myocardial infarction or rhabdomyolysis.
Albumin and prothrombin can also act as proxies for liver health, whereby drops in either protein indicate liver dysfunction.
Albumin and prothrombin can also act as proxies for liver health, whereby drops in either protein indicate liver dysfunction.
Name the three indicators of the liver's excretory capacity.
Name the three indicators of the liver's excretory capacity.
Unconjugated bilirubin is a byproduct of heme breakdown.
Unconjugated bilirubin is a byproduct of heme breakdown.
The liver takes up unconjugated bilirubin and converts it into conjugated bilirubin, a more soluble form.
The liver takes up unconjugated bilirubin and converts it into conjugated bilirubin, a more soluble form.
Elevated levels of unconjugated bilirubin (without a rise in conjugated bilirubin) might indicate hemolysis.
Elevated levels of unconjugated bilirubin (without a rise in conjugated bilirubin) might indicate hemolysis.
Elevated levels of conjugated bilirubin (without a rise in unconjugated bilirubin) might indicate cholestasis.
Elevated levels of conjugated bilirubin (without a rise in unconjugated bilirubin) might indicate cholestasis.
Serum gamma-glutamyltransferase (GGT) is elevated in cholestasis, viral hepatitis, and non-alcoholic liver disease.
Serum gamma-glutamyltransferase (GGT) is elevated in cholestasis, viral hepatitis, and non-alcoholic liver disease.
Alkaline phosphatase is a membrane enzyme on hepatocytes lining the biliary ductules.
Alkaline phosphatase is a membrane enzyme on hepatocytes lining the biliary ductules.
Flashcards
Hepatic circulation routes
Hepatic circulation routes
Blood reaches the liver through two pathways: the hepatic artery (oxygenated blood), and the hepatic portal vein (deoxygenated blood with absorbed compounds).
Hepatic artery
Hepatic artery
Carries oxygenated blood to the liver.
Hepatic portal vein
Hepatic portal vein
Carries deoxygenated blood to the liver, carrying absorbed nutrients & hormones.
Portal system
Portal system
Signup and view all the flashcards
Liver lobules
Liver lobules
Signup and view all the flashcards
Sinusoids
Sinusoids
Signup and view all the flashcards
Hepatocytes
Hepatocytes
Signup and view all the flashcards
Carbohydrate metabolism
Carbohydrate metabolism
Signup and view all the flashcards
Gluconeogenesis
Gluconeogenesis
Signup and view all the flashcards
Lipid metabolism
Lipid metabolism
Signup and view all the flashcards
Ketosis
Ketosis
Signup and view all the flashcards
Lipoproteins
Lipoproteins
Signup and view all the flashcards
Protein Metabolism
Protein Metabolism
Signup and view all the flashcards
Bilirubin
Bilirubin
Signup and view all the flashcards
Kupffer cells
Kupffer cells
Signup and view all the flashcards
Vitamin D metabolism
Vitamin D metabolism
Signup and view all the flashcards
Liver function tests
Liver function tests
Signup and view all the flashcards
AST:ALT ratio
AST:ALT ratio
Signup and view all the flashcards
Albumin and prothrombin
Albumin and prothrombin
Signup and view all the flashcards
Serum bilirubin
Serum bilirubin
Signup and view all the flashcards
Serum γ-glutamyltransferase (GGT)
Serum γ-glutamyltransferase (GGT)
Signup and view all the flashcards
Alkaline phosphatase
Alkaline phosphatase
Signup and view all the flashcards
Cholestasis
Cholestasis
Signup and view all the flashcards
Study Notes
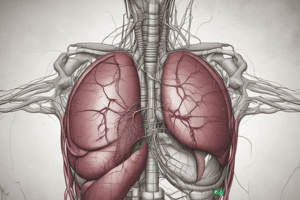
Hepatic Circulation
-
Blood circulates to the liver via two routes.
-
Oxygenated blood from the hepatic artery (branch of the cephalic trunk/arteries) supplies the liver.
-
Superior and inferior mesenteric arteries, and other branches, oxygenate the stomach, pancreas, small intestine, and large intestine.
-
Blood from these GI organs is collected and carried via the hepatic portal vein, containing absorbed nutrients and hormones.
-
A portal system involves blood passing through two organs before returning to venous circulation.
-
Blood is circulated through the liver sinusoids, a type of capillary with large gaps.
-
Blood is drained into the central vein of liver lobules, then into the hepatic vein, and finally the inferior vena cava.
Liver Lobules and Lobes
- The liver is composed of lobes further divided into hexagonal lobules.
- Each lobule corner is vascularized by a portal vein branch, hepatic artery branch, and a bile duct.
- Oxygenated blood from the hepatic artery and deoxygenated (absorbed nutrient-rich) blood from the hepatic portal vein converge to form sinusoids.
- Blood moves toward a centrally placed central vein.
- Hepatocytes contact sinusoids and bile canaliculi.
- Hepatocytes absorb compounds from the blood and detoxify others, also secreting bile into the bile canaliculi.
- Kupffer cells (phagocytes) line the sinusoid walls and remove defective blood cells, bacteria, and other foreign materials.
Hepatocyte Functions
-
Metabolism:
- Carbohydrate: Stores glucose as glycogen, breaks down glycogen into glucose, forms glucose from noncarbohydrates (gluconeogenesis), and makes triglycerides from glucose (lipogenesis) in the fed state.
- Lipid: Metabolizes fatty acids to ketones in the fasting state; synthesizes lipoproteins for triglyceride and cholesterol transport; produces bile.
- Protein: Synthesizes plasma proteins (albumin, globulins, fibrinogen), clotting factors; interconverts amino acids; converts ammonia to urea; recycles heme (bilirubin conversion).
- Miscellaneous: Metabolizes Vitamin D; detoxifies compounds; contributes to hormone half-life.
-
Storage: Stores glycogen, fat-soluble vitamins (A, D, K).
Assessing Liver Function
- Liver health is monitored by evaluating protein synthesis and excretory capacity.
- Serum liver enzymes (AST, ALT) are indicative of liver damage.
- AST:ALT ratios can distinguish various liver conditions or stages (e.g. non-alcoholic fatty liver disease, viral hepatitis).
- Indicators of excretory capacity include serum bilirubin, y-glutamyltransferase (GGT), and alkaline phosphatase. Elevated levels can indicate conditions like cholestasis or liver diseases.
Review Questions: Bile Salt Pathway
- Bile salts travel through hepatocytes, bile canaliculi, bile ducts, and finally the small intestine lumen to emulsify fats.
Review Questions: Blood Supply to Liver
- Blood flows through the hepatic artery, sinusoids, central vein, hepatic vein, and vena cava to supply oxygen and remove CO2.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.