Podcast
Questions and Answers
What primarily triggers the development of pneumonia according to the described model?
What primarily triggers the development of pneumonia according to the described model?
- A macroaspiration event
- An inflammatory event leading to cytokine release (correct)
- A sterile space being invaded by microorganisms
- An epithelial injury due to a bacterial infection
Which bacteria are specifically mentioned as potentially promoted by the inflammatory response in pneumonia?
Which bacteria are specifically mentioned as potentially promoted by the inflammatory response in pneumonia?
- Haemophilus influenzae and Legionella pneumophila
- Staphylococcus aureus and Escherichia coli
- Streptococcus pneumoniae and Pseudomonas aeruginosa (correct)
- Klebsiella pneumoniae and Mycobacterium tuberculosis
What is pneumonia primarily defined as?
What is pneumonia primarily defined as?
- An infection of the cardiovascular system
- An infection of the pulmonary parenchyma (correct)
- An infection of the gastrointestinal tract
- An infection of the central nervous system
What role do cytokines and chemokines play in pneumonia development?
What role do cytokines and chemokines play in pneumonia development?
Which classification of pneumonia is not considered for those who have been hospitalized?
Which classification of pneumonia is not considered for those who have been hospitalized?
In cases of community-acquired pneumonia (CAP) and hospital-acquired pneumonia (HAP), which factor is often a trigger?
In cases of community-acquired pneumonia (CAP) and hospital-acquired pneumonia (HAP), which factor is often a trigger?
What significant issue is associated with the category of health care–associated pneumonia (HCAP)?
What significant issue is associated with the category of health care–associated pneumonia (HCAP)?
What phenomenon is described as a feedback loop in the context of pneumonia?
What phenomenon is described as a feedback loop in the context of pneumonia?
What is the main outcome of the innate and adaptive immune responses in pneumonia?
What is the main outcome of the innate and adaptive immune responses in pneumonia?
Which of the following risk factors is NOT associated with MRSA and Pseudomonas aeruginosa infections?
Which of the following risk factors is NOT associated with MRSA and Pseudomonas aeruginosa infections?
How might an aspiration pneumonia specifically be triggered?
How might an aspiration pneumonia specifically be triggered?
Why should the use of the HCAP category be discontinued?
Why should the use of the HCAP category be discontinued?
What defines aspiration pneumonia?
What defines aspiration pneumonia?
Which of the following describes pneumonia in relation to microorganisms?
Which of the following describes pneumonia in relation to microorganisms?
Which type of pneumonia has been misdiagnosed and underestimated despite its significant morbidity and mortality?
Which type of pneumonia has been misdiagnosed and underestimated despite its significant morbidity and mortality?
Which of the following is most relevant when assessing pneumonia risk factors?
Which of the following is most relevant when assessing pneumonia risk factors?
Which virus is known to complicate influenza virus infection?
Which virus is known to complicate influenza virus infection?
What is a potential serious consequence of infections caused by MRSA?
What is a potential serious consequence of infections caused by MRSA?
Which of the following is associated with aspiration pneumonia in individuals with poor dentition?
Which of the following is associated with aspiration pneumonia in individuals with poor dentition?
What are community-associated MRSA strains capable of doing?
What are community-associated MRSA strains capable of doing?
In which cases is a specific etiology often difficult to determine?
In which cases is a specific etiology often difficult to determine?
Which type of pneumonia is associated with those typically acquiring it in a hospital setting?
Which type of pneumonia is associated with those typically acquiring it in a hospital setting?
What is the estimated yearly cost of community-acquired pneumonia (CAP)?
What is the estimated yearly cost of community-acquired pneumonia (CAP)?
What percentage of hospitalized CAP patients are readmitted within one month of discharge?
What percentage of hospitalized CAP patients are readmitted within one month of discharge?
Which of the following is NOT a risk factor for community-acquired pneumonia?
Which of the following is NOT a risk factor for community-acquired pneumonia?
What is a specific risk factor for pneumonia caused by Legionella?
What is a specific risk factor for pneumonia caused by Legionella?
How many cases of CAP occur per 1000 persons per year among adults?
How many cases of CAP occur per 1000 persons per year among adults?
Which patient history increases the likelihood of CA-MRSA pneumonia?
Which patient history increases the likelihood of CA-MRSA pneumonia?
Which of these factors is associated with increased risk for pneumococcal pneumonia?
Which of these factors is associated with increased risk for pneumococcal pneumonia?
What clinical manifestation could indicate worsening severity of pneumonia?
What clinical manifestation could indicate worsening severity of pneumonia?
What are some typical symptoms that are compatible with a diagnosis of Community-Acquired Pneumonia (CAP)?
What are some typical symptoms that are compatible with a diagnosis of Community-Acquired Pneumonia (CAP)?
What is the sensitivity of physical examination findings in diagnosing CAP?
What is the sensitivity of physical examination findings in diagnosing CAP?
Why might chest radiography be necessary in the diagnosis of CAP?
Why might chest radiography be necessary in the diagnosis of CAP?
What findings on a chest radiograph may indicate increased severity of pneumonia?
What findings on a chest radiograph may indicate increased severity of pneumonia?
When is clinical and radiologic assessment usually sufficient for treatment of pneumonia?
When is clinical and radiologic assessment usually sufficient for treatment of pneumonia?
Which rapid test can influence initial management decisions in suspected pneumonia cases?
Which rapid test can influence initial management decisions in suspected pneumonia cases?
What does a CT scan help diagnose in cases of suspected pneumonia?
What does a CT scan help diagnose in cases of suspected pneumonia?
Which of the following is NOT a reliable indicator for the etiologic diagnosis of pneumonia?
Which of the following is NOT a reliable indicator for the etiologic diagnosis of pneumonia?
Flashcards are hidden until you start studying
Study Notes
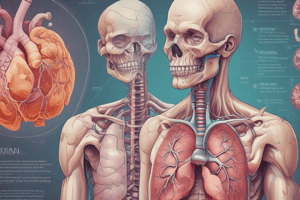
Definition of Pneumonia
- Pneumonia is an infection of the pulmonary parenchyma, linked to high morbidity and mortality rates despite often being misdiagnosed and mistreated.
- Common classifications include community-acquired pneumonia (CAP), hospital-acquired pneumonia (HAP), and ventilator-associated pneumonia (VAP).
- Health care–associated pneumonia (HCAP) includes cases with multidrug-resistant (MDR) pathogens, typically linked to HAP, but its predictive value for resistant infections is poor.
- Risk factors for infection with MRSA and Pseudomonas aeruginosa encompass previous isolation of the organism, hospitalization, and antibiotic treatment within the past 90 days.
- Aspiration pneumonia occurs due to macroaspiration of oropharyngeal or gastric contents and exists along a continuum between CAP and HAP.
Pathogenesis
- Pneumonia results from inflammatory events causing epithelial or endothelial injury, leading to the release of cytokines, chemokines, and catecholamines that promote bacterial growth.
- Inflammatory responses can enhance nutrient availability and bacterial growth, potentially creating positive feedback loops that exacerbate the infection.
- Community-acquired pneumonia may be triggered by viral infections along with microaspiration of oropharyngeal organisms.
Risk Factors
- CAP causes over 55,000 deaths annually and contributes to 1.2 million hospitalizations, with 70% of patients treated as outpatients and 30% hospitalized.
- The incidence rate among adults is approximately 16–23 cases per 1,000 persons per year, peaking at age extremes.
- Risk factors include alcoholism, asthma, immunosuppression, and age over 70 years. In the elderly, decreased cough/gag reflexes heighten pneumonia risk.
- Specific risk factors for pneumococcal pneumonia include dementia, heart failure, COPD, and HIV infection.
- CA-MRSA pneumonia risks are higher in those with skin colonization or following viral infections, while Enterobacteriaceae targets patients with recent hospitalization or antibiotic use.
Clinical Manifestations
- Symptoms of pneumonia range from mild to severe, including cough, fever, sputum production, and dyspnea, necessitating a thorough patient history for accurate diagnosis.
- Chest radiography is critical for confirming CAP, with findings that may indicate severity (e.g., cavitation, multilobar disease) and occasionally suggest specific pathogens.
- Radiographic results may also highlight conditions like S.aureus infections (pneumatoceles) or upper-lobe cavitating lesions due to tuberculosis.
Diagnosis and Treatment
- Diagnosis often requires comprehensive clinical assessment and radiologic evaluation, as the sensitivity and specificity of physical exams for pneumonia are relatively low (58% and 67% respectively).
- Rapid point-of-care tests, like those for influenza, can influence treatment decisions by prompting targeted interventions and secondary prevention.
- Laboratory results are typically not available in time to inform initial management for outpatients; thus, clinical and radiologic findings drive early treatment.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.