Podcast
Questions and Answers
A patient presents with hallux varus, and upon examination, the MPJ exhibits supination/varus rotation, adductus, and hyperextension, accompanied by HIPJ hyperflexion. Which plane(s) of deformity does this encompass?
A patient presents with hallux varus, and upon examination, the MPJ exhibits supination/varus rotation, adductus, and hyperextension, accompanied by HIPJ hyperflexion. Which plane(s) of deformity does this encompass?
- Sagittal plane only
- Transverse plane only
- Frontal and transverse planes
- Triplanar: frontal, transverse, and sagittal planes (correct)
What anatomical abnormality is most closely associated with congenital hallux varus?
What anatomical abnormality is most closely associated with congenital hallux varus?
- Abnormal insertion of the abductor hallucis muscle (correct)
- Rupture of the plantar fascia
- Absence of the flexor hallucis brevis tendon
- Calcification within the extensor hallucis longus tendon
Following a hallux valgus correction, a patient develops iatrogenic hallux varus. Which surgical miscalculation is the most likely cause?
Following a hallux valgus correction, a patient develops iatrogenic hallux varus. Which surgical miscalculation is the most likely cause?
- Overcorrection of the intermetatarsal angle (IMA) (correct)
- Failure to resect the fibular sesamoid
- Inadequate medial capsulorrhaphy
- Insufficient lateral release
During a hallux valgus correction, a surgeon reduces the intermetatarsal angle (IMA) to a negative value. What potential complication is the patient at highest risk for developing?
During a hallux valgus correction, a surgeon reduces the intermetatarsal angle (IMA) to a negative value. What potential complication is the patient at highest risk for developing?
Which of the following scenarios during or after hallux valgus surgery increases the risk of developing hallux varus?
Which of the following scenarios during or after hallux valgus surgery increases the risk of developing hallux varus?
Flashcards
Hallux Valgus
Hallux Valgus
Deformity where the big toe deviates laterally towards the other toes.
Hallux Varus
Hallux Varus
Deformity where the big toe deviates medially, away from the other toes.
Hallux Varus Triplanar Deformity
Hallux Varus Triplanar Deformity
Supination/varus rotation, adductus, hyperextension at the MPJ, and hyperflexion at the HIPJ.
Hallux Varus Causes
Hallux Varus Causes
Signup and view all the flashcards
Iatrogenic Hallux Varus
Iatrogenic Hallux Varus
Signup and view all the flashcards
Study Notes
- Hallux Varus is discussed by Christina Pratt, DPM for Podiatric Surgery II (PM791) at Samuel Merritt University.
Terminology
- Hallux Valgus refers to lateral deviation of the great toe.
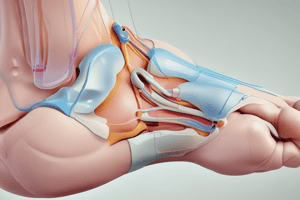
- Hallux Varus, technically a triplanar deformity, involves the medial deviation of the great toe.
- Triplanar deformity includes:
- MPJ supination/varus rotation (frontal plane).
- MPJ adductus (transverse plane).
- MPJ hyperextension (sagittal plane).
- HIPJ hyperflexion (sagittal plane).
Etiology of Hallux Varus
- Causes can be:
- Idiopathic
- Iatrogenic
- Trauma
- Congenital defects.
- Underlying systemic conditions
- Primary congenital hallux varus consists of varus as the only deformity.
- Secondary congenital hallux varus involves varus with met adductus and hindfoot equinovarus or clubfoot, potentially linked to systemic neuromuscular conditions like polio.
- Systemic conditions that can cause Hallux Varus:
- Rheumatoid arthritis (chronic inflammation causing joint weakening/subluxation).
- Psoriatic arthritis.
- Charcot Marie Tooth Disease.
Role of the Abductor Hallucis
- It is implicated in congenital hallux varus.
- Abnormal insertion of the Abductor Hallucis.
- It remains on the medial side of the foot in some patients.
- Typical insertion is at the plantar medial base of the proximal phalanx, along with the Flexor Hallucis Brevis (FHB).
- Altered insertion changes the directional pull across the MPJ, leading to:
- More adduction.
- Less stabilization and flexion.
Iatrogenic Etiology of Hallux Varus
- Includes:
- Overcorrecting the Intermetatarsal Angle (IMA).
- Staking of the metatarsal head.
- Excision of the fibular sesamoid.
- Aggressive lateral release.
- Aggressive medial capsulorraphy.
- Tight/aggressive bandaging post-op.
- Most iatrogenic causes are associated with prior Hallux Abducto Valgus (HAV) surgery.
Overcorrecting IMA
- It is the most common reason for iatrogenic hallux varus after HAV surgery (80%).
- Normal IMA is 8-10°.
- Some surgeons reduce IMA to < 8°.
- Negative IMA is more likely to result in varus.
- Evidence of overcorrection:
- IMA <8°.
- Tibilal sesamoid position (TSP) 1-3.
Staking of the Metatarsal Head
- It involves resection of the medial eminence is performed in most HAV procedures.
- Violation of the sagittal groove.
- The Medial proximal phalanx base travels in this groove.
- Problems can arise when too much is resected.
- Evidence of staking:
- Intra-op violation of the sagittal groove.
- Intra-op instability/subluxation of MPJ.
- Tibial peek.
Excision of the Fibular Sesamoid
- The McBride procedure involves the excision fibular sesamoid.
- Severing the lateral head of FHB.
- The medial head of FHB gains mechanical advantage.
- The Modified McBride leaves the fibular sesamoid intact with adductor tendon release or transfer.
Aggressive Lateral Release
- Involves the release of 4 structures at the lateral MPJ.
- Requires careful, meticulous dissection and identification.
- Some surgeons resect/remove more structures, like the "interspacectomy".
- Includes release of the:
- Lateral capsule
- Lateral head FHB
- You should not cut both the lateral head of the FHB and adductor hallucis tendon
- This would allow the medial structures to overpower.
- The Lateral Release includes:
- DTIL
- Fibular suspensory ligaments
- Fibular sesamoid (possible excision)
- Adductor tendon
Aggressive Medial Capsulorraphy
- Tightens down the medial capsule following HAV correction.
- Removing too much tissue can overtighten the medial side.
- this leads to medial deviation
Tight/Aggressive Bandaging Post-Op
- Bandaging/dressings are not always benign.
- It is common to bandage the hallux in an overcorrected position.
- Prolonged position can allow for adaptive soft tissue changes.
- In combination with other mistakes, exacerbates deformity.
Hallux Varus Clinical Evaluation.
- HPI includes:
- Prior HAV surgery.
- Pain with footwear
- History of neuromuscular disorders and ligamentous laxity.
- Investigate details of prior HAV surgery.
- What procedures were done?
- What was the look of the toe after surgery?
- How did the post-op recover?
- Were there any issues of being compliant?
- PE is similar to HAV evaluation and includes:
- Degree of MPJ ROM.
- Pain with MPJ ROM.
- Crepitus.
- Reducible deformity or rigid deformity.
- Hallux toe purchase (often non-purchasing).
- Lesser digit adduction (following the hallux).
- Medial hallux callusing.
- Transfer metatarsalgia callusing.
- Nail changes.
Hallux Varux Imaging Evaluation
- X-Rays show:
- Adduction of the hallux.
- MPJ position.
- Deviated / subluxed / dislocated.
- Arthritic changes to MPJ.
- Flattening of base proximal phalanx.
- Asymmetric joint space narrowing.
- Peri-articular osteophytes.
- Subchondral sclerosis.
- Erosive/cystic changes.
- Long or short 1st metatarsal.
- Fibular sesamoid present.
- TSP (medial position).
- IMA (negative).
- HAA (negative).
- Medial eminence staking (if h/o HAV surgery).
- Adduction of the hallux.
Joint Alignment Terminology
- Congruous/Rectus are parallel/close.
- Deviated refers to it's instersection outside of the joint.
- Subluxed refers to it's intersection within the joint.
- Dislocated is a lack of joint contact.
Hallux Varus Conservative Management
- There are minimal options.
- Footwear changes (wide toebox) and taping (if reducible) may help.
- Splinting hallux out of varus position is helpful if recognized very quickly post-op.
- There is Variable long-term outcome.
Hallux Varus Surgical Management
- Includes:
- Soft tissue procedures.
- Osseous procedures.
- Combination of both.
- What caused it and can the cause be surgically reversed are important questions to ask.
Soft Tissue Procedures
- EHL Tendon Transfer:
- Resect from the distal phalanx insertion.
- Insert into the lateral base proximal phalanx.
- Performed with HIPJ arthrodesis.
- It may avoid need for HIPJ arthrodesis, but it is often too thin a tendon for this.
- Abductor Hallucis release:
- Lengthening or transfer consists of resecting from insertion at plantar medial base proximal phalanx (with FHB).
- Relieves the adductory pull on the hallux.
- Better results are achieved in cases of a medial insertion.
- Must have little to no joint (osseous) adaptive changes.
- Assess if it provides enough correction.
- The tendon may also be too short to transfer.
- Tibial sesamoidectomy:
- Uncommon as the primary surgical option.
- Release of the medial head of FHB relieves medial structure dominance.
- Lateral capsular tensioning:
- Newer fixation options allow for recreation of lateral capsular strutures.
- There is ability to tension as appropriate to achieve position.
Osseous Procedures
- Keller resection arthroplasty:
- Described by Keller (1904) for hallux valgus correction.
- It is now commonly used (still not first choice) in hallux limitus.
- Involves the resection of 1/3 of the base proximal phalanx.
- Can also apply to hallux varus correction, but with caution in an already unstable MPJ complex.
- May perform with soft tissue work.
- Reverse Chevron osteotomy:
- Common joint salvage option in cases of staking of the met head.
- Performed using the same technique as a traditional chevron osteotomy.
- The capital fragment is pushed medially instead.
- Reverse Reverdin osteotomy has been described in "reverse correction".
- Reverse osteotomy procedures:
- Reverdin
- Chevron.
- Scarf.
- OBWO.
- CBWO.
- 1st MPJ Arthrodesis:
- Very common in hallux varus correction of multiple etiologies.
- Severe loss of ROM with DJD is the only option.
- Allows for correction of triplanar components of deformity.
- Predictable position
- Reliable outcome.
Botox for Hallux Varus
- Some literature supports the use of neurotoxin.
- Requires repeated injections.
- Limited success.
Hallux Varus Pearls
- Accurately determine the cause of hallux varus.
- The status of the MPJ is critical to procedure selection.
- There are limited conservation options
- Soft tissue procedures are often adjunct to osseous correction
- 1st MPJ arthrodesis is the standard to correct all aspects of the deformity.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Hallux Varus, a triplanar deformity, involves medial deviation of the great toe, including MPJ supination/varus rotation, adductus, and hyperextension, plus HIPJ hyperflexion. Etiologies range from idiopathic to iatrogenic, trauma, congenital defects, and systemic conditions like rheumatoid arthritis.