Podcast
Questions and Answers
What percentage of cardiac output is received by the kidneys?
What percentage of cardiac output is received by the kidneys?
- 25-30%
- 15-20%
- 20-25% (correct)
- 30-35%
What is the primary function of the distal tubule and collecting ducts in the nephron?
What is the primary function of the distal tubule and collecting ducts in the nephron?
- Reabsorption of essential nutrients
- Secretion of hormones
- Filtration of blood
- Fine tuning of water and acid/base for homeostasis (correct)
What is the term for the sudden onset of kidney injury?
What is the term for the sudden onset of kidney injury?
- End-stage renal disease
- Renal insufficiency
- Acute kidney injury (correct)
- Chronic kidney disease
Which of the following is a measure of the volume of blood filtered through the kidney per minute?
Which of the following is a measure of the volume of blood filtered through the kidney per minute?
What is the normal range of glomerular filtration rate (GFR) per day?
What is the normal range of glomerular filtration rate (GFR) per day?
What is the benefit of using cystatin C to estimate GFR?
What is the benefit of using cystatin C to estimate GFR?
What is the primary difference between a 24-hour urine and a spot urine test?
What is the primary difference between a 24-hour urine and a spot urine test?
What is the term for the presence of protein in the urine?
What is the term for the presence of protein in the urine?
What is the term for the abnormally high levels of waste products in the blood?
What is the term for the abnormally high levels of waste products in the blood?
What is the location of the adrenal glands in relation to the kidneys?
What is the location of the adrenal glands in relation to the kidneys?
What is the most likely cause of proteinuria exceeding 1-2 g/day?
What is the most likely cause of proteinuria exceeding 1-2 g/day?
What is the term for proteinuria caused by stressors such as acute illness, exercise, and orthostatic proteinuria?
What is the term for proteinuria caused by stressors such as acute illness, exercise, and orthostatic proteinuria?
What is the term for proteinuria resulting from faulty reabsorption of normally filtered proteins in the proximal tubule?
What is the term for proteinuria resulting from faulty reabsorption of normally filtered proteins in the proximal tubule?
What is the minimum number of RBCs per HPF required to consider hematuria clinically significant?
What is the minimum number of RBCs per HPF required to consider hematuria clinically significant?
What is the likely cause of hematuria in a patient with a history of anthracycline use?
What is the likely cause of hematuria in a patient with a history of anthracycline use?
What is the term for kidney injury caused by impaired perfusion?
What is the term for kidney injury caused by impaired perfusion?
What is the characteristic BUN:creatinine ratio in prerenal azotemia?
What is the characteristic BUN:creatinine ratio in prerenal azotemia?
What is the most common cause of AKI?
What is the most common cause of AKI?
What is the term for the sudden onset of kidney injury?
What is the term for the sudden onset of kidney injury?
What percentage of AKI cases are due to renal causes?
What percentage of AKI cases are due to renal causes?
What is the primary goal of treatment for prerenal AKI?
What is the primary goal of treatment for prerenal AKI?
What is the most common cause of postrenal AKI?
What is the most common cause of postrenal AKI?
What is the primary difference between nephritic and nephrotic syndrome?
What is the primary difference between nephritic and nephrotic syndrome?
When should a patient with AKI be referred to a urologist?
When should a patient with AKI be referred to a urologist?
What is the most common cause of AKI in patients with COVID-19?
What is the most common cause of AKI in patients with COVID-19?
What is the primary goal of treatment for COVID-19-related AKI?
What is the primary goal of treatment for COVID-19-related AKI?
What is the term for the sudden increase in urinary output after relief of obstruction?
What is the term for the sudden increase in urinary output after relief of obstruction?
What is the benefit of bladder catheterization and ultrasonography in patients with suspected postrenal AKI?
What is the benefit of bladder catheterization and ultrasonography in patients with suspected postrenal AKI?
What is the term for the damage to the kidney tissue itself, including the tubules, interstitium, vasculature, and glomeruli?
What is the term for the damage to the kidney tissue itself, including the tubules, interstitium, vasculature, and glomeruli?
What is the primary reason for hospitalization in patients with AKI?
What is the primary reason for hospitalization in patients with AKI?
What is the primary goal of the initial approach to kidney disease?
What is the primary goal of the initial approach to kidney disease?
What is the characteristic of Acute Kidney Injury (AKI) that distinguishes it from Chronic Kidney Disease (CKD)?
What is the characteristic of Acute Kidney Injury (AKI) that distinguishes it from Chronic Kidney Disease (CKD)?
What is the significance of oliguria in distinguishing between AKI and CKD?
What is the significance of oliguria in distinguishing between AKI and CKD?
What is the primary purpose of examining urine within one hour of collection?
What is the primary purpose of examining urine within one hour of collection?
What is the significance of protein on dipstick examination?
What is the significance of protein on dipstick examination?
What is the characteristic of granular casts in urinary sediment?
What is the characteristic of granular casts in urinary sediment?
What is the definition of proteinuria?
What is the definition of proteinuria?
What is the significance of WBCs in urinary sediment?
What is the significance of WBCs in urinary sediment?
What is a characteristic of chronic kidney disease (CKD) that makes it difficult to diagnose in its early stages?
What is a characteristic of chronic kidney disease (CKD) that makes it difficult to diagnose in its early stages?
What is a major risk factor for the development of chronic kidney disease (CKD)?
What is a major risk factor for the development of chronic kidney disease (CKD)?
What is a common manifestation of uremic syndrome?
What is a common manifestation of uremic syndrome?
Which of the following is a consequence of chronic kidney disease (CKD) leading to end-stage disease?
Which of the following is a consequence of chronic kidney disease (CKD) leading to end-stage disease?
What is a complication of chronic kidney disease (CKD) that may occur in patients taking insulin for diabetes?
What is a complication of chronic kidney disease (CKD) that may occur in patients taking insulin for diabetes?
What is a characteristic of chronic kidney disease (CKD) that distinguishes it from acute kidney injury (AKI)?
What is a characteristic of chronic kidney disease (CKD) that distinguishes it from acute kidney injury (AKI)?
What is a risk factor for cardiovascular disease (CVD) in patients with chronic kidney disease (CKD)?
What is a risk factor for cardiovascular disease (CVD) in patients with chronic kidney disease (CKD)?
What is a consequence of the destruction of nephrons in chronic kidney disease (CKD)?
What is a consequence of the destruction of nephrons in chronic kidney disease (CKD)?
What is the primary complication of CKD that tends to be progressive and salt-sensitive?
What is the primary complication of CKD that tends to be progressive and salt-sensitive?
What is the primary indicator of chronic scarring of advanced CKD on renal imaging?
What is the primary indicator of chronic scarring of advanced CKD on renal imaging?
What is the primary cause of death in patients with CKD?
What is the primary cause of death in patients with CKD?
What is the primary treatment for anemia of chronic disease in pre-ESKD CKD?
What is the primary treatment for anemia of chronic disease in pre-ESKD CKD?
What is the primary mechanism of metabolic acidosis in CKD?
What is the primary mechanism of metabolic acidosis in CKD?
What is the primary complication of CKD that contributes to vessel stiffness?
What is the primary complication of CKD that contributes to vessel stiffness?
What is the primary indication for hospitalization and nephrology consultation in patients with uremia?
What is the primary indication for hospitalization and nephrology consultation in patients with uremia?
What is the primary treatment for hyperkalemia in CKD?
What is the primary treatment for hyperkalemia in CKD?
What is the primary complication of CKD that contributes to fractures?
What is the primary complication of CKD that contributes to fractures?
What is the primary goal of treatment for CKD?
What is the primary goal of treatment for CKD?
What is the primary goal of managing traditional CVD risk factors in patients with CKD?
What is the primary goal of managing traditional CVD risk factors in patients with CKD?
In patients with advanced CKD, why may glycemic targets need to be relaxed?
In patients with advanced CKD, why may glycemic targets need to be relaxed?
What is the reasonable daily sodium intake goal in patients with advanced CKD?
What is the reasonable daily sodium intake goal in patients with advanced CKD?
At what level of GFR should potassium restriction be considered?
At what level of GFR should potassium restriction be considered?
What is the recommended daily fluid restriction in patients with CKD and volume overload?
What is the recommended daily fluid restriction in patients with CKD and volume overload?
What is the recommended daily phosphorus intake in patients with CKD?
What is the recommended daily phosphorus intake in patients with CKD?
When should a patient with CKD be referred to a nephrologist?
When should a patient with CKD be referred to a nephrologist?
What is the primary reason for hospital admission in patients with CKD?
What is the primary reason for hospital admission in patients with CKD?
What is the recommendation for metformin use in patients with CKD receiving iodinated contrast media?
What is the recommendation for metformin use in patients with CKD receiving iodinated contrast media?
What is the primary predictor of mortality in patients with CKD?
What is the primary predictor of mortality in patients with CKD?
What percentage of patients with SLE develop lupus nephritis?
What percentage of patients with SLE develop lupus nephritis?
What is the recommended treatment for all patients with lupus nephritis?
What is the recommended treatment for all patients with lupus nephritis?
What is the prognosis for patients with SLE who undergo dialysis?
What is the prognosis for patients with SLE who undergo dialysis?
What is the term for the pattern of injury seen in lupus nephritis?
What is the term for the pattern of injury seen in lupus nephritis?
What is the recommended therapy for patients with class III or IV lesions?
What is the recommended therapy for patients with class III or IV lesions?
What is the prognosis for patients with class VI lesions?
What is the prognosis for patients with class VI lesions?
What is the term for the pattern of injury seen in Goodpasture Syndrome?
What is the term for the pattern of injury seen in Goodpasture Syndrome?
What is the significance of serum complement levels in Goodpasture Syndrome?
What is the significance of serum complement levels in Goodpasture Syndrome?
What percentage of patients with Goodpasture syndrome have circulating anti-GBM antibodies?
What percentage of patients with Goodpasture syndrome have circulating anti-GBM antibodies?
What is the primary goal of treatment in patients with Goodpasture syndrome?
What is the primary goal of treatment in patients with Goodpasture syndrome?
Which of the following is a poor prognostic factor in patients with Goodpasture syndrome?
Which of the following is a poor prognostic factor in patients with Goodpasture syndrome?
What is the pathogenesis of ANCA-associated vasculitis?
What is the pathogenesis of ANCA-associated vasculitis?
What is a common symptom of ANCA-associated vasculitis?
What is a common symptom of ANCA-associated vasculitis?
What is a characteristic of granulomatosis with polyangiitis?
What is a characteristic of granulomatosis with polyangiitis?
What is a concerning sign in patients with ANCA-associated vasculitis?
What is a concerning sign in patients with ANCA-associated vasculitis?
What is the term for a kidney disease characterized by inflammation and damage to the glomeruli?
What is the term for a kidney disease characterized by inflammation and damage to the glomeruli?
Which of the following is a characteristic of nephritic syndrome?
Which of the following is a characteristic of nephritic syndrome?
Which of the following is a primary cause of Focal Segmental Glomerulosclerosis (FSGS)?
Which of the following is a primary cause of Focal Segmental Glomerulosclerosis (FSGS)?
What is the characteristic pattern of injury seen on biopsy in IgA nephropathy?
What is the characteristic pattern of injury seen on biopsy in IgA nephropathy?
What is the primary goal of treatment for post-infectious glomerulonephritis?
What is the primary goal of treatment for post-infectious glomerulonephritis?
Which of the following is a characteristic of Diabetic Nephropathy?
Which of the following is a characteristic of Diabetic Nephropathy?
What is the primary treatment for HIV-associated nephropathy?
What is the primary treatment for HIV-associated nephropathy?
Which of the following is a characteristic of Minimal Change Disease?
Which of the following is a characteristic of Minimal Change Disease?
What is the primary complication of Membranous Nephropathy?
What is the primary complication of Membranous Nephropathy?
Which of the following is a characteristic of Renal Amyloidosis?
Which of the following is a characteristic of Renal Amyloidosis?
What is the primary goal of treatment for IgA nephropathy?
What is the primary goal of treatment for IgA nephropathy?
What is the primary mechanism of acute tubular necrosis?
What is the primary mechanism of acute tubular necrosis?
What is the characteristic urinary finding in acute tubular necrosis?
What is the characteristic urinary finding in acute tubular necrosis?
What is the primary goal of treatment in acute tubular necrosis?
What is the primary goal of treatment in acute tubular necrosis?
What is the characteristic metabolic abnormality in acute tubular necrosis?
What is the characteristic metabolic abnormality in acute tubular necrosis?
What is the name of the phase characterized by a sharp increase in creatinine levels?
What is the name of the phase characterized by a sharp increase in creatinine levels?
What is the primary indication for dialysis in acute tubular necrosis?
What is the primary indication for dialysis in acute tubular necrosis?
What is the term for the excessive urine output that occurs during the recovery phase of acute tubular necrosis?
What is the term for the excessive urine output that occurs during the recovery phase of acute tubular necrosis?
What is the primary difference between the initial and maintenance phases of acute tubular necrosis?
What is the primary difference between the initial and maintenance phases of acute tubular necrosis?
What is the primary mechanism of injury in interstitial nephritis due to drug hypersensitivity reaction?
What is the primary mechanism of injury in interstitial nephritis due to drug hypersensitivity reaction?
In analgesic nephropathy, which of the following is a common finding on CT scan?
In analgesic nephropathy, which of the following is a common finding on CT scan?
What is the primary mechanism of injury in heavy metal toxicity?
What is the primary mechanism of injury in heavy metal toxicity?
What is the primary goal of treatment for interstitial nephritis?
What is the primary goal of treatment for interstitial nephritis?
What is the primary complication of chronic kidney disease that may occur in patients taking insulin for diabetes?
What is the primary complication of chronic kidney disease that may occur in patients taking insulin for diabetes?
What is the primary indicator of chronic scarring of advanced CKD on renal imaging?
What is the primary indicator of chronic scarring of advanced CKD on renal imaging?
What is the primary cause of death in patients with CKD?
What is the primary cause of death in patients with CKD?
What is the primary goal of treatment for PTRA?
What is the primary goal of treatment for PTRA?
What is the primary complication of sickle cell disease on the kidneys?
What is the primary complication of sickle cell disease on the kidneys?
What is the primary reason for hospitalization in patients with AKI?
What is the primary reason for hospitalization in patients with AKI?
What is the likely cause of hypercalciuria and nephrolithiasis in patients with occupational exposures?
What is the likely cause of hypercalciuria and nephrolithiasis in patients with occupational exposures?
What is the characteristic of urine culture in patients with renal tuberculosis?
What is the characteristic of urine culture in patients with renal tuberculosis?
What is the pathophysiological mechanism of lithium toxicity in the kidneys?
What is the pathophysiological mechanism of lithium toxicity in the kidneys?
What is the laboratory finding in patients with lead poisoning?
What is the laboratory finding in patients with lead poisoning?
What is the treatment goal for patients with chronic interstitial nephritis due to lead exposure and lithium use?
What is the treatment goal for patients with chronic interstitial nephritis due to lead exposure and lithium use?
What is the characteristic imaging finding in patients with lithium-related nephrotoxicity?
What is the characteristic imaging finding in patients with lithium-related nephrotoxicity?
What is the diagnostic criterion for lead poisoning?
What is the diagnostic criterion for lead poisoning?
What is the complication of untreated renal tuberculosis?
What is the complication of untreated renal tuberculosis?
What is the primary mechanism of lead toxicity in the proximal tubules?
What is the primary mechanism of lead toxicity in the proximal tubules?
What is the primary goal of supportive care in patients with chronic interstitial nephritis?
What is the primary goal of supportive care in patients with chronic interstitial nephritis?
What is the primary mechanism of kidney injury in cast nephropathy?
What is the primary mechanism of kidney injury in cast nephropathy?
What is the characteristic appearance of medullary sponge kidney on imaging?
What is the characteristic appearance of medullary sponge kidney on imaging?
What is the primary complication of medullary sponge kidney?
What is the primary complication of medullary sponge kidney?
What is the primary predictor of kidney function decline in patients with autosomal dominant polycystic kidney disease?
What is the primary predictor of kidney function decline in patients with autosomal dominant polycystic kidney disease?
Which of the following medications may be prescribed to help lower blood pressure and reduce proteinuria in patients with kidney disease?
Which of the following medications may be prescribed to help lower blood pressure and reduce proteinuria in patients with kidney disease?
What is the typical presentation of a simple renal cyst?
What is the typical presentation of a simple renal cyst?
What is the percentage of patients with autosomal dominant polycystic kidney disease who will have kidney failure by age 70?
What is the percentage of patients with autosomal dominant polycystic kidney disease who will have kidney failure by age 70?
What is the characteristic of a simple renal cyst on ultrasound?
What is the characteristic of a simple renal cyst on ultrasound?
What is the primary concern in a patient with a complex renal cyst?
What is the primary concern in a patient with a complex renal cyst?
What is the probable diagnosis for a patient presenting with abdominal or flank pain, hematuria, and a history of UTI and nephrolithiasis?
What is the probable diagnosis for a patient presenting with abdominal or flank pain, hematuria, and a history of UTI and nephrolithiasis?
What is the primary goal of treatment for medullary sponge kidney?
What is the primary goal of treatment for medullary sponge kidney?
What is the likely cause of impaired ability to concentrate or dilute urine in older patients?
What is the likely cause of impaired ability to concentrate or dilute urine in older patients?
What is the prognosis for patients with medullary sponge kidney?
What is the prognosis for patients with medullary sponge kidney?
What is the benefit of using ACE inhibitors or ARBs in patients with autosomal dominant polycystic kidney disease?
What is the benefit of using ACE inhibitors or ARBs in patients with autosomal dominant polycystic kidney disease?
What is the primary difference between cast nephropathy and medullary sponge kidney?
What is the primary difference between cast nephropathy and medullary sponge kidney?
What is the percentage of patients with autosomal dominant polycystic kidney disease who have associated cysts in the liver?
What is the percentage of patients with autosomal dominant polycystic kidney disease who have associated cysts in the liver?
What is the primary complication of cast nephropathy?
What is the primary complication of cast nephropathy?
What is the consequence of impaired renal clearance of medications in older patients?
What is the consequence of impaired renal clearance of medications in older patients?
What is the diagnostic criterion for autosomal dominant polycystic kidney disease in patients under 30 years old?
What is the diagnostic criterion for autosomal dominant polycystic kidney disease in patients under 30 years old?
What is the goal of treatment for patients with autosomal dominant polycystic kidney disease?
What is the goal of treatment for patients with autosomal dominant polycystic kidney disease?
What is the primary cause of direct renal toxicity in Rhabdomyolysis?
What is the primary cause of direct renal toxicity in Rhabdomyolysis?
What is the goal of treatment in Rhabdomyolysis?
What is the goal of treatment in Rhabdomyolysis?
What is the most common cause of Renal Artery Stenosis?
What is the most common cause of Renal Artery Stenosis?
What is the mechanism by which Renal Artery Stenosis leads to Chronic Kidney Disease?
What is the mechanism by which Renal Artery Stenosis leads to Chronic Kidney Disease?
What is the primary complication of Rhabdomyolysis?
What is the primary complication of Rhabdomyolysis?
What is the term for the syndrome of acute necrosis of skeletal muscle resulting in markedly elevated plasma creatine kinase levels and myoglobinuria?
What is the term for the syndrome of acute necrosis of skeletal muscle resulting in markedly elevated plasma creatine kinase levels and myoglobinuria?
What is the primary goal of medical management in Renal Artery Stenosis?
What is the primary goal of medical management in Renal Artery Stenosis?
What is the term for the narrowing of the renal arteries, leading to reduced blood flow to the kidneys?
What is the term for the narrowing of the renal arteries, leading to reduced blood flow to the kidneys?
What is the primary cause of Chronic Kidney Disease in Renal Artery Stenosis?
What is the primary cause of Chronic Kidney Disease in Renal Artery Stenosis?
What is the term for the sudden reduction in kidney function, which can occur with ACE inhibitors or ARBs?
What is the term for the sudden reduction in kidney function, which can occur with ACE inhibitors or ARBs?
What is the preferred method of reversing hypokalemia in patients who are unable to tolerate oral supplementation?
What is the preferred method of reversing hypokalemia in patients who are unable to tolerate oral supplementation?
What is the primary mechanism by which insulin and glucose treats hyperkalemia?
What is the primary mechanism by which insulin and glucose treats hyperkalemia?
What is the recommended dose of calcium gluconate for the treatment of hyperkalemia?
What is the recommended dose of calcium gluconate for the treatment of hyperkalemia?
What is the most likely cause of hypomagnesemia in a patient with lithium therapy?
What is the most likely cause of hypomagnesemia in a patient with lithium therapy?
What is the primary treatment for asymptomatic hypermagnesemia in patients with normal kidney function?
What is the primary treatment for asymptomatic hypermagnesemia in patients with normal kidney function?
What is the characteristic clinical presentation of severe hypophosphatemia?
What is the characteristic clinical presentation of severe hypophosphatemia?
What is the primary cause of hyperphosphatemia in patients with tumor lysis syndrome?
What is the primary cause of hyperphosphatemia in patients with tumor lysis syndrome?
Why do we correct calcium levels for albumin?
Why do we correct calcium levels for albumin?
What is the primary cause of hypocalcemia in patients with chronic kidney disease?
What is the primary cause of hypocalcemia in patients with chronic kidney disease?
What is the primary complication of rapid calcium infusion?
What is the primary complication of rapid calcium infusion?
What is the primary reason for avoiding D5W in cases of increased intracranial pressure?
What is the primary reason for avoiding D5W in cases of increased intracranial pressure?
What percentage of Total Body Fluids is distributed to the intracellular space?
What percentage of Total Body Fluids is distributed to the intracellular space?
What is the primary difference between Lactated Ringers and 0.9% NaCl?
What is the primary difference between Lactated Ringers and 0.9% NaCl?
What is the primary goal of fluid resuscitation in cases of hemorrhagic or septic shock?
What is the primary goal of fluid resuscitation in cases of hemorrhagic or septic shock?
What is the characteristic of colloid IV fluids that differentiates them from crystalloids?
What is the characteristic of colloid IV fluids that differentiates them from crystalloids?
What is the significance of 25% albumin in colloid IV fluids?
What is the significance of 25% albumin in colloid IV fluids?
What is the associated complication of dextran and Hetastarch in colloid IV fluids?
What is the associated complication of dextran and Hetastarch in colloid IV fluids?
What is the characteristic of 0.9% NaCl or Lactated Ringers in crystalloid IV fluids?
What is the characteristic of 0.9% NaCl or Lactated Ringers in crystalloid IV fluids?
What is the primary electrolyte determinant of plasma osmolality?
What is the primary electrolyte determinant of plasma osmolality?
What is the term for the effect of hypotonic fluids on blood cells?
What is the term for the effect of hypotonic fluids on blood cells?
What is the primary mechanism that maintains normal plasma concentrations of potassium?
What is the primary mechanism that maintains normal plasma concentrations of potassium?
What is the preferred treatment for euvolemic hyponatremia?
What is the preferred treatment for euvolemic hyponatremia?
What is the term for the sudden onset of organ hypoperfusion due to intravascular volume depletion?
What is the term for the sudden onset of organ hypoperfusion due to intravascular volume depletion?
What is the primary cause of hypernatremia?
What is the primary cause of hypernatremia?
What is the term for the rapid correction of hyponatremia, which can lead to cerebral edema?
What is the term for the rapid correction of hyponatremia, which can lead to cerebral edema?
What is the primary goal of treatment for hypovolemic hyponatremia?
What is the primary goal of treatment for hypovolemic hyponatremia?
What is the term for the regulation of nerve and muscle function, as well as acid-base and water balance?
What is the term for the regulation of nerve and muscle function, as well as acid-base and water balance?
What is the primary complication of correcting hypernatremia too rapidly?
What is the primary complication of correcting hypernatremia too rapidly?
Flashcards are hidden until you start studying
Study Notes
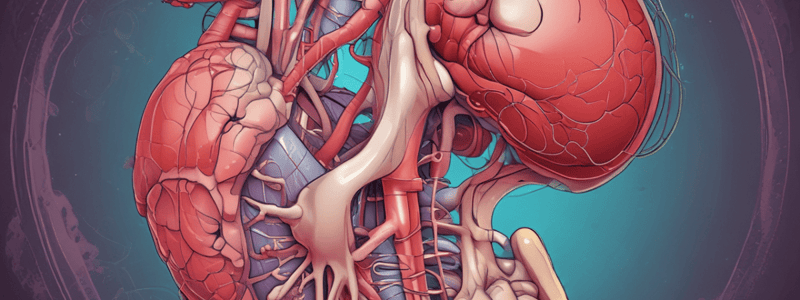
Kidney Anatomy
- Kidneys are retroperitoneal, cushioned by fat, and have adrenals resting on top of them
- The right kidney is slightly lower than the left due to the liver's position
Kidney Function
- Kidneys receive 20-25% of cardiac output, approximately 1 liter per minute
- Of this, 125ml/min filters into the Glomerular Filtration Rate (GFR)
- Only 1.5 liters/day of the 173 liters/day of filtrate is excreted as urine, with 99% being reabsorbed
- Distal tubule and collecting ducts handle fine-tuning of water and acid-base for homeostasis
Renal Patients
- Patients may be inpatient or outpatient, with symptoms ranging from none to highly symptomatic
- Symptoms include dysuria, urgency, frequency, incontinence, nocturia, polyuria, oliguria, anuria, flank pain, hematuria, uremia, and azotemia
- Findings include weight gain, hypertension, edema, mental status changes, ascites, muffled heart tones, and crackles
Kidney Disease Classification
- Acute kidney injury: sudden onset
- Chronic kidney disease: long-lasting, caused by another condition (e.g., diabetes, hypertension)
- Renal insufficiency: some lessening of kidney function (GFR impacted)
- Renal failure: kidneys not working, requiring dialysis
- End-stage renal disease
Laboratory Studies
- Glomerular filtration rate (GFR): the volume of blood filtered through the kidney per minute
- Normal GFR: 150-250 L/24hr or 90-120 ml/min
- GFR starts a slow annual decline after 30-35 years old
- Decreased in patients with renal disease, with monitoring recommended in patients with chronic kidney disease (CKD)
- Estimated via calculations using the CKD-EPI Equation
Additional Laboratory Studies
- Cystatin C: a protein produced by all nucleated cells, completely reabsorbed by the kidney at the proximal renal tubule
- Elevated cystatin C levels indicate poor kidney function
- Serum creatinine: a byproduct of the breakdown of creatine phosphate in muscle, removed in the kidneys via glomerular filtration
- 24-hour urine: carefully collected urine over an exact 24-hour cycle, quantifying total protein excretion
- Spot urine: a marker of urinary excretion of albumin, with normal levels being < 30mg/24hr urine sample
Kidney Disease
- Much kidney disease is asymptomatic and often discovered incidentally through tests for other conditions
- Symptoms of kidney disease may include hypertension, edema, nausea, or hematuria, which can lead to a diagnosis of kidney disease
- Initial approach to kidney disease involves assessing the cause and severity of any abnormal renal function
Acute vs Chronic Kidney Disease
- Kidney disease can be acute (Acute Kidney Injury, AKI) or chronic (Chronic Kidney Disease, CKD)
- Acute Kidney Injury (AKI) is characterized by a rapid worsening of kidney function over hours to days, resulting in retention of waste products in the blood
- Chronic Kidney Disease (CKD) is characterized by a gradual loss of kidney function over months to years
- Determining AKI from CKD is important for diagnosis and treatment
Evaluation of Urine
- Urine collection involves clean catch or catheterization, and examination within one hour
- Dipstick urinalysis involves testing for urinary pH, specific gravity, protein, hemoglobin, glucose, ketones, bilirubin, nitrites, and leukocyte esterase
- Microscopy of centrifuged urinary sediment involves examining formed elements, such as crystals, cells, casts, and infectious organisms
Proteinuria
- Defined as excessive protein excretion in the urine, generally greater than 150 mg/24 hours in adults
- Proteinuria can be due to glomerular disease, functional proteinuria, overload proteinuria, or tubular proteinuria
- Glomerular proteinuria results from effacement of epithelial cell foot processes, leading to increased glomerular permeability and increased filtration of albumin
Hematuria
- Blood in the urine is considered clinically significant if >3 RBCs per HPF on at least 2 occasions
- Hematuria can be due to renal or extrarenal causes, including glomerulonephritis, hereditary disorders, cysts, calculi, interstitial nephritis, and genitourinary neoplasms
Causes of AKI
- Categorized by anatomy: prerenal, renal, and postrenal causes
- Prerenal causes include impaired perfusion, cardiac failure, sepsis, blood loss, dehydration, and vascular occlusion
- Renal causes include glomerulonephritis, small-vessel vasculitis, acute tubular necrosis, drugs, toxins, and interstitial nephritis
- Postrenal causes include urinary calculi, retroperitoneal fibrosis, benign prostatic enlargement, prostate cancer, cervical cancer, urethral stricture, and meatal stenosis/phimosis
Prerenal AKI
- Most common etiology of AKI, occurring in 40-80% of cases
- Defined as a physiologic response to renal hypoperfusion
- Reversible with restoration of renal blood flow, but can develop into intrinsic kidney injury if persists
Postrenal AKI
- Least common cause of AKI, occurring in 5-10% of cases
- Defined as obstruction to urinary outflow from both kidneys or a single functioning kidney
- Can occur due to obstruction at the level of the urethra, bladder, ureters, or renal pelvises
Intrinsic Renal Causes of AKI
- Corresponds to damage to the kidney tissue itself
- Includes glomerular disorders, renal disorders, and nephritic vs nephrotic syndrome
When to Refer and Admit
- Refer to a nephrologist if AKI persists for 1-2 weeks or has a concerning degree of severity
- Admit to the hospital if AKI is severe, requires acute intervention, or has abnormalities that cannot be handled expeditiously in an outpatient setting
COVID-19 and AKI
- 30% of patients hospitalized with COVID-19 and 50% of critically ill patients are affected by AKI
- Associated with poorer prognosis
- Most common cause of AKI in COVID-19 patients is acute tubular necrosis (ATN)
Essentials of Diagnosis
- Decline in GFR over months to years, with persistent proteinuria or abnormal renal morphology, and hypertension in most cases.
- Bilateral small or echogenic kidneys on ultrasound in advanced disease.
- Symptoms and signs of uremia when nearing end-stage disease.
Chronic Kidney Disease (CKD)
- Affects at least 10% of Americans.
- CKD may be asymptomatic until it nears end-stage, with over 70% of late-stage cases due to diabetes mellitus or hypertension/cardiovascular disease.
- Glomerulonephritis, cystic diseases, chronic tubulointerstitial diseases, and other renal diseases account for the remainder.
- Progressive decline in kidney function occurs even if the cause of damage can be found and treated.
- Destruction of nephrons leads to compensatory hypertrophy and supranormal GFR of the remaining nephrons.
- Serum creatinine may remain relatively normal even in the face of significant loss of renal mass.
- CKD is an independent risk factor for CVD, with proteinuric CKD conferring the highest risk.
Signs and Symptoms
- Stages 1-4 CKD are typically asymptomatic (>15% GFR).
- Symptoms develop slowly and do not manifest until disease is far advanced (GFR < 5-10 mL/minute/1.73 m2).
- Uremic syndrome results from the accumulation of metabolic waste products.
- Symptoms of uremia may include fatigue, anorexia, nausea, and a metallic taste in the mouth.
- Neurologic symptoms may include memory impairment, insomnia, restless legs, and twitching.
- Generalized pruritus (without rash) may occur, as may decreased libido and menstrual irregularities.
- Medications that are cleared by the kidneys will accumulate as kidney function worsens and may result in toxicity.
Laboratory Findings
- eGFR must be measured over time to monitor progression.
- Anemia, hyperphosphatemia, hypocalcemia, hyperkalemia, and metabolic acidosis are common complications of advanced CKD.
- Urinary sediment may show broad waxy casts as a result of dilated, hypertrophic nephrons.
- Any proteinuria must be monitored over time.
- Higher urinary protein excretion is associated with more rapid progression of CKD and increased risk of cardiovascular mortality.
Imaging Findings
- Abnormalities on renal imaging (e.g., polycystic kidneys or a single kidney) are diagnostic of CKD, even when eGFR is normal.
- Small, echogenic kidneys bilaterally (less than 9-10 cm) by ultrasonography indicate chronic scarring of advanced CKD.
- Large kidneys can be seen with adult polycystic kidney disease, diabetic nephropathy, HIV-associated nephropathy, plasma cell myeloma, amyloidosis, and obstructive uropathy.
Complications
- Patients with CKD experience greater morbidity/mortality compared with the general population.
- ~80% of patients with CKD die before reaching ESKD, primarily of CVD.
- Hypertension is the most common complication of CKD, tending to be progressive and salt-sensitive.
- A low-salt diet (2 g/day) is essential to control BP and avoid volume overload.
- Diuretics are nearly always needed to help control HTN.
- Thiazides work well in earlier CKD, while loop diuretics may be more effective when GFR < 30 mL/minute/1.73 m2.
- Initial drug therapy for proteinuric patients should include ACE inhibitors or ARBs.
- Complications result in increased cardiac workload due to hypertension, volume overload, and anemia.
- May also have accelerated rates of atherosclerosis and vascular calcification, contributing to LVH and heart failure with preserved EF.
CKD: Treatment
- Aggressive control of diabetes is crucial in early CKD, but glycemic targets may need to be relaxed in advanced CKD due to increased risk of hypoglycemia.
- Blood pressure control is vital to slow the progression of all forms of CKD.
- In proteinuric patients, agents that block the renin-angiotensin-aldosterone system are important.
- SGLT2 inhibitors can slow CKD progression, even in patients without diabetes.
- Management of traditional CVD risk factors is vital, and risks for AKI should be minimized or avoided.
CKD: Complications
- Patients with CKD should be evaluated by a renal nutritionist.
- Protein restriction is necessary, with a recommended intake of 0.6-0.8 g/kg/day to slow CKD progression.
- Salt and water restriction are important, with a goal of 2 g/day of sodium and daily fluid restriction to 2 L if volume overload is present.
- Potassium restriction is necessary once the GFR has fallen below 10-20 mL/minute/1.73 m2, and patients should limit their intake to less than 50-60 mEq/day.
- Phosphorus restriction is necessary, with a goal of lowering elevated serum phosphorus levels toward normal in all stages of CKD; dietary phosphate restriction to 800-1000 mg/day is the first step.
CKD: Complications (Drugs and Mortality)
- Many drugs excreted by the kidney require dosage adjustments based on GFR.
- The risk of lactic acidosis with metformin is due to both dose and eGFR, and it should be discontinued when eGFR < 50%.
- Diabetes, advanced age, low serum albumin, lower SES, and inadequate dialysis are all significant predictors of mortality.
CKD: Referral and Admission
- Patients with stage 3-5 CKD should be referred to a nephrologist for management in conjunction with the PCP.
- Patients with other forms of CKD, such as proteinuria greater than 1 g/day or polycystic kidney disease, should be referred to a nephrologist at earlier stages.
- Admission should be considered for decompensation related to CKD, such as worsening of acid-base status, electrolyte abnormalities, and volume overload, that cannot be appropriately treated in the outpatient setting.
IV Contrast in Patients on Metformin
- The US FDA recommends withholding metformin temporarily in patients receiving iodinated contrast media if their GFR is between 30 and 60 mL/min/1.73 m2 and restarting after creatinine has been checked 48 hours after contrast.
- The American College of Radiology (ACR) recommends that, for patients with eGFR ≥30 mL/min/1.73 m2, there is no need to discontinue metformin prior to the procedure.
- For patients with eGFR ≤30 mL/min/1.73 m2, metformin should be withheld at the time of the contrast infusion and for 48 hours after the procedure, and renal function should be reassessed.
Acute Kidney Injury and Chronic Kidney Disease
- Acute Kidney Injury (AKI): sudden deterioration of renal function over days to weeks, leading to uremic symptoms and biochemical abnormalities, and can be life-threatening
- Chronic Kidney Disease (CKD): long-standing and progressive impairment of kidney function over weeks to months, eventually leading to end-stage renal disease
Nephritic and Nephrotic Syndromes
- Nephritic syndrome: characterized by red blood cells, red blood cell casts, proteinuria, hypertension, and edema
- Nephrotic syndrome: characterized by proteinuria > 3.5 g, fatty casts, and no white/red cells
Primary Glomerular Diseases
-
Minimal Change Disease (MCD):
- Most common cause of proteinuric kidney disease in children (~80%)
- Often resolves with corticosteroid treatment
- Can occur following viral upper respiratory infections, neoplasms, drugs, or hypersensitivity reactions
-
Focal Segmental Glomerulosclerosis (FSGS):
- Can be primary or secondary to another underlying disease
- Genetic testing is becoming more common, especially in children
- Diagnosis requires kidney biopsy
-
Membranous Nephropathy:
- Most common cause of primary adult nephrotic syndrome
- "Spike and dome" pattern on kidney biopsy
- Secondary causes include hepatitis B virus and cancer
-
Diabetic Nephropathy:
- Most common cause of ESKD in the US
- Develops about 10 years after onset of DM
- Family history of kidney disease increases risk
-
HIV-Associated Nephropathy:
- Presents with nephrotic syndrome and declining GFR in patients with active HIV infection
- Associated with low CD4 counts and AIDS
-
Renal Amyloidosis:
- Rare cause of nephrotic syndrome caused by tissue deposition of overproduced, abnormally folded protein
- Diagnosis requires kidney biopsy
-
Glomerulonephritis:
- Uncommon cause of AKI (~5% of cases)
- Glomerular inflammation often incites a proliferative response
-
IgA Nephropathy:
- Most common primary glomerular disease worldwide
- Can be primary or secondary to cirrhosis, celiac disease, or infections
- Classic presentation is an episode of gross hematuria associated with a mucosal viral infection
-
Post-Infectious Glomerulonephritis:
- Symptoms occur during or after an infection
- Characterized by glomerular injury during active or recent infection
-
Lupus Nephritis:
- Occurs in 35-90% of patients with SLE
- Presents within the nephritic spectrum
- All patients with SLE should have routine UAs to monitor for hematuria or proteinuria
-
Goodpasture Syndrome:
- May be preceded by an upper respiratory tract infection
- Kidney findings are consistent with an RPGN
- Serum complement levels are normal### Goodpasture Syndrome
-
Circulating anti-GBM antibodies are present in over 90% of patients
-
Kidney biopsy typically shows crescent formation with light microscopy
-
Patients with pulmonary hemorrhage and strong clinical suspicion of Goodpasture syndrome should be treated emergently, often prior to confirming the diagnosis
-
Treatment involves a combination of therapeutic plasma exchange and administration of corticosteroids and cyclophosphamide
-
Patients with oliguric AKI or requiring dialysis upon presentation have a poor prognosis
ANCA-Associated Vasculitis (AAV)
- Causes nephritic syndrome
- Caused by granulomatosis with polyangiitis, microscopic polyangiitis, and eosinophilic granulomatosis with polyangiitis (formerly Churg-Strauss disease)
- Can present as a kidney-limited disease without systemic vasculitis
- Pathogenesis involves cytokine-primed neutrophils presenting cytoplasmic antigens on their surfaces
- Renal involvement classically presents as RPGN, but more indolent presentations can be seen
- Most cases are idiopathic, but some are linked to infection, environmental exposure, or drug exposure
- Symptoms may include fever, malaise, weight loss, and upper or lower respiratory tract symptoms
- Vasculitic involvement of dermal capillaries and nerve arterioles can result in purpura and mononeuritis multiplex
- 90% of patients with granulomatosis with polyangiitis have upper or lower respiratory tract symptoms
- Hemoptysis is a concerning sign of possible alveolar hemorrhage and usually warrants hospitalization and aggressive immunosuppression
Glomerular Diseases
- A glomerulus is a network of capillaries responsible for retaining plasma proteins in blood when filtrate is excreted in urine
- Pathology affecting the glomerulus can lead to proteinuria and hematuria
- Glomerular diseases can be nephrotic or nephritic
- Most glomerular disorders are treated with corticosteroids and/or immune-suppressing agents
- Some of these are acute kidney injuries that can lead to chronic kidney disease and even end-stage renal disease
Here are the study notes:
Acute Tubular Necrosis (ATN)
- Most common cause of AKI (80% of cases)
- Etiologies: ischemia, drugs, toxins, sepsis, and contrast dye
- Pathophysiology:
- Hypoperfusion leads to cellular death and muddy brown casts in tubules
- Lack of oxygen hurts cells, stops vasodilators, and constricts tubules
- Dead cells clog tubules, reducing GFR and increasing BUN/Creatinine
- Clinical Presentation:
- Decreased GFR and increased BUN/Creatinine levels
- Oliguria or anuria
- Edema and fatigue
- Hematuria (dead cells/casts)
- Diagnostic Evaluation:
- Serum creatinine > 0.3 mg/dl within 48 hrs or 1.5 times baseline within 7 days
- Metabolic acidosis
- Hyperkalemia, hyperphosphatemia
- Renal tubular casts ("muddy brown")
- Renal epithelial cells
- BUN:Creatinine ratio < 20:1 (intrarenal)
- Increased fractional excretion of sodium (FENa)
Rhabdomyolysis
- Defined as a syndrome of acute necrosis of skeletal muscle
- Etiologies: trauma, prolonged immobility, drug toxicity, hypothermia
- Pathophysiology:
- Release of myoglobin leads to direct renal toxicity
- Causes AKI in 10-15% of cases
- Clinical Presentation:
- Myalgias or weakness
- Dark urine
- May be asymptomatic
- Diagnostic Evaluation:
- CK levels > 20,000 IU/L
- Elevated LFTs
- Electrolyte abnormalities (e.g., hyperkalemia)
- Urine dipstick positive for "blood" without RBCs on microscopy
Renal Artery Stenosis (RAS)
- Characterized by narrowing of renal arteries, reducing blood flow to kidneys
- Causes: atherosclerosis (most common), fibromuscular dysplasia
- Mechanisms:
- Renal artery narrowing leads to reduced kidney perfusion
- RAAS activation causes renovascular hypertension
- Impact on kidney health:
- Hypertension
- Ischemic nephropathy
- AKI (especially with ACE inhibitors or ARBs)
- Chronic kidney disease (CKD)
Interstitial Nephritis
- Pathophysiology and Etiology:
- Drug hypersensitivity reaction (70% of cases)
- Infections (15%)
- Autoimmune diseases (6%)
- Clinical Presentation:
- Fever, rash, arthralgias, peripheral blood eosinophilia
- Diagnostic Evaluation:
- Urinalysis: WBCs, RBCs, white cell casts
- Peripheral blood smear: eosinophilia
- Ultrasound: may visualize kidneys
- Kidney biopsy: clinical history and lab data often suggest the diagnosis
- Treatment and Prognosis:
- Supportive care and removal of the causative agent
- Good prognosis for acute interstitial nephritis with weeks to months of recovery
I hope this helps! Let me know if you'd like me to add anything.### Renal Failure
- Renal failure is a rare but potential complication of recurrent issues like UTIs, kidney stones, and severe infections.
Simple Cysts in the Kidney
- Most simple cysts are discovered incidentally on ultrasound (US) and are typically asymptomatic.
- Simple cysts can become infected or cause hematuria.
- Simple cysts must be differentiated from malignancy, abscess, or polycystic kidney disease.
- A simple cyst is considered benign if it:
- Is echo-free on US
- Has sharply demarcated (smooth) walls
- Has an enhanced back wall on US
- Benign cysts are not usually treated unless the patient becomes symptomatic (e.g., drainage if blocking urine flow).
- Rarely, simple cysts can transform into renal cell carcinoma.
- Complex cysts (with thick walls, calcifications/solid components, or mixed echogenicity) should be investigated further for carcinoma.
- Renal cell carcinoma is typically vascular.
- Cysts with questionable characteristics require periodic reevaluation and possible urologic consultation.
Adverse Events of IV Fluids
- Arrhythmia, edema, and electrolyte abnormalities can occur if IV fluids are given incorrectly.
Distribution of Total Body Fluids
- Total body fluids (TBF) account for 60% of body weight in men and 50% in women.
- Intracellular fluids account for 60% of TBF, while extracellular fluids account for 40% of TBF.
- Extracellular fluids are further divided into interstitial space (75%) and plasma (25%).
Types of IV Fluids
- Crystalloids: distribute evenly into extracellular space, composed of water, dextrose, Na+, Cl-, and other electrolytes.
- Examples: Lactated Ringers (LR), 0.9% NaCl.
- Characteristics: 25% remains in intravascular space, 75% distributes into interstitial space.
- Free Water (D5W): metabolized to water and carbon dioxide, distributes evenly into TBF; not suitable for resuscitation.
- Colloids: more expensive than crystalloids, remains in plasma, and can cause coagulopathy and kidney impairment.
- Examples: packed RBCs, pooled human plasma, semisynthetic glucose polymers, and semisynthetic hydroxyethyl starch.
- Characteristics: 500 mL of colloid equals 500 mL of intravascular volume expansion.
Contraindications and Precautions
- D5W should be avoided in cases of increased intracranial pressure because it can cross into cerebral cells and cause further ICP elevation.
- D5W can cause hyperglycemia due to its small amount of dextrose.
Goals of Fluid Resuscitation
- Restore intravascular volume and prevent organ hypoperfusion.
- Administer fluids rapidly, with 500-1000 mL boluses, and reassess after each bolus.
Preferred IV Fluid for Resuscitation
- Crystalloids, particularly Lactated Ringers, are preferred for fluid resuscitation.
Signs and Symptoms of Intravascular Dehydration
- Tachycardia, hypotension, orthostasis, increased BUN/Cr ratio >10:1, dry mucous membranes, decreased skin turgor, reduced urine output, and dizziness.
Osmolality and Osmolarity
- Osmolality: osmoles of solute per kg of solvent (mOsm/kg).
- Osmolarity: osmoles of solute per L of solution (Osm/L).
Functions of Electrolytes
- Regulate nerve and muscle function, maintain acid-base and water balance.
Hyponatremia
- Defined as sodium levels below 135 mmol/L.
- Causes: increased ADH, excessive water retention, and low solute intake.
- Types:
- Hypervolemic: excess Na+ and fluid, but fluid excess > Na+ excess.
- Euvolemic: normal Na+ but excess fluid volume, no edema.
- Hypovolemic: low Na+ and fluid, Na+ lower than fluid.
Symptoms of Hyponatremia
- Mild: nausea, headache, lethargy, malaise.
- Severe: seizures, brain herniation, coma, and death.
Causes of Hyponatremia
- Hyperglycemia, replacement of lost solute with water, volume depletion, SIADH, glucocorticoid deficiency, medications, and renal failure.
Treatment of Hyponatremia
- Fluid restriction, vasopressin agonists, and stop offending medications.
- Avoid rapid correction of hyponatremia to prevent osmotic demyelination.
Osmotic Demyelination
- Occurs with rapid correction of hyponatremia, leading to lethargy, affective changes, and permanent neurological damage.
Correcting Hypernatremia
- Aim for a safe range of 120-125 Na+, avoid rapid increases/decreases of >8-12 Na+ per 24 hours.
- Correct over 48-96 hours to prevent cerebral edema and brain damage.
Potassium Homeostasis
- Maintained by the Na+/K+ pump, which regulates potassium levels in the body.
Causes of Potassium Depletion
- Increased K+ into cells, diuretics, hypomagnesemia, and vomiting and diarrhea.
Monitoring Potassium and Magnesium
- Magnesium levels should be monitored in relationship to potassium levels.
Conditions Requiring IV Potassium Supplementation
- EKG changes, symptoms, or inability to tolerate oral potassium.
Causes of Hyperkalemia
- Increased K+ intake, shift of K+ from IC to EC, and reduced urinary excretion.
Signs and Symptoms of Hyperkalemia
- Muscle weakness, paralysis, abnormal cardiac conduction, and VFIB.
Treatment of Hyperkalemia
- Sodium polystyrene sulfonate, IV calcium, insulin and glucose, sodium bicarbonate, and beta-adrenergic agonists.
Calcium in Hyperkalemia Treatment
- Used to antagonize the effect of K+ on cardiac conduction cells, but does not decrease plasma K+ levels.
Magnesium Distribution
- Primarily distributed in bone.
Causes of Hypomagnesemia
- Renal insufficiency, excessive vitamin or antacid use, lithium therapy, and hypercatabolic states.
Symptoms of Hypomagnesemia
- Arrhythmias, muscle weakness, lethargy, confusion, and loss of deep tendon reflexes.
Hyperphosphatemia
- Causes: tumor lysis syndrome, kidney dysfunction, and internal redistribution.
- Symptoms: delirium, lethargy, paresthesia, neuromuscular hyperexcitability, and seizures.
Hypophosphatemia
- Causes: decreased GI absorption, reduced tubular reabsorption, and internal redistribution.
- Symptoms: tissue hypoxia, confusion, delirium, seizures, and respiratory failure.
Calcium Correction
- Corrected for albumin levels, as low albumin levels can cause falsely low calcium levels.
Causes of Hypocalcemia
- CKD, hypoparathyroidism, vitamin D deficiency, hyperphosphatemia, and hypomagnesemia.
Symptoms of Hypocalcemia
- Neuromuscular, neurologic, acute, and chronic symptoms.
Calcium Infusion Precautions
- Infusion should be done slowly to avoid hypotension, bradycardia, and asystole.
Drugs that Cause Hypercalcemia
- Lithium and thiazide diuretics.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.