Podcast
Questions and Answers
Which imaging technique is specifically used to assess vesicoureteric reflux (VUR)?
Which imaging technique is specifically used to assess vesicoureteric reflux (VUR)?
- Voiding cystourethrography (correct)
- DMSA scan
- MRI
- CT scan
A renal abscess is a complication of a urinary tract infection (UTI).
A renal abscess is a complication of a urinary tract infection (UTI).
True (A)
What type of scan is used to assess the glomerular filtration rate (GFR) of kidneys separately?
What type of scan is used to assess the glomerular filtration rate (GFR) of kidneys separately?
DTPA scan
The _____ scan is used to determine the degree of scarring in kidneys affected by VUR.
The _____ scan is used to determine the degree of scarring in kidneys affected by VUR.
Match the following terms with their corresponding descriptions:
Match the following terms with their corresponding descriptions:
Which of the following cell types is NOT found in the cortical collecting duct?
Which of the following cell types is NOT found in the cortical collecting duct?
True hypoaldosteronism is characterized by low levels of both renin and aldosterone.
True hypoaldosteronism is characterized by low levels of both renin and aldosterone.
What is the primary role of aldosterone in the P-cells of the cortical collecting duct?
What is the primary role of aldosterone in the P-cells of the cortical collecting duct?
Aldosterone receptor blockers include __________ and __________.
Aldosterone receptor blockers include __________ and __________.
Match the following conditions with their characteristics:
Match the following conditions with their characteristics:
Which transport mechanism is NOT involved in the reabsorption of magnesium ($Mg^{2+}$)?
Which transport mechanism is NOT involved in the reabsorption of magnesium ($Mg^{2+}$)?
Phosphorus is reabsorbed in multiple organs throughout the body.
Phosphorus is reabsorbed in multiple organs throughout the body.
What is the role of the Na⁺ - H⁺ antiport in the proximal convoluted tubule?
What is the role of the Na⁺ - H⁺ antiport in the proximal convoluted tubule?
The _______ is responsible for the maximum absorption of magnesium ($Mg^{2+}$).
The _______ is responsible for the maximum absorption of magnesium ($Mg^{2+}$).
Match the following transport mechanisms with their descriptions:
Match the following transport mechanisms with their descriptions:
Which type of defect is most commonly associated with inherited Type-1 RTA?
Which type of defect is most commonly associated with inherited Type-1 RTA?
Type-1 RTA is most commonly acquired due to Sjogren's syndrome.
Type-1 RTA is most commonly acquired due to Sjogren's syndrome.
What is the urine pH requirement for confirming an inability to acidify urine in Type-1 RTA?
What is the urine pH requirement for confirming an inability to acidify urine in Type-1 RTA?
In Type-1 RTA, calcium reabsorption from bone leads to __________, stone formation, and renal rickets.
In Type-1 RTA, calcium reabsorption from bone leads to __________, stone formation, and renal rickets.
Match the conditions with their corresponding features of Type-1 RTA:
Match the conditions with their corresponding features of Type-1 RTA:
Which of the following is an inherited cause of Proximal RTA?
Which of the following is an inherited cause of Proximal RTA?
Euglycemic glycosuria is a feature of Global Dysfunction of PCT.
Euglycemic glycosuria is a feature of Global Dysfunction of PCT.
What is the common clinical feature that leads to renal rickets in patients with Fanconi syndrome?
What is the common clinical feature that leads to renal rickets in patients with Fanconi syndrome?
Patients with Proximal RTA typically experience _____________ due to salt and water depletion.
Patients with Proximal RTA typically experience _____________ due to salt and water depletion.
Match the following causes of Proximal RTA with their categories:
Match the following causes of Proximal RTA with their categories:
What percentage of children have at least one compound papilla?
What percentage of children have at least one compound papilla?
Simple conical papillae allow for reflex.
Simple conical papillae allow for reflex.
Name one characteristic of composite papillae.
Name one characteristic of composite papillae.
The percentage of children with simple conical papillae in the mid pole is __________.
The percentage of children with simple conical papillae in the mid pole is __________.
Match the types of papillae with their characteristics:
Match the types of papillae with their characteristics:
What is Bartter syndrome primarily characterized by?
What is Bartter syndrome primarily characterized by?
Patients with Bartter syndrome experience hyperkalemia as a symptom.
Patients with Bartter syndrome experience hyperkalemia as a symptom.
What treatment is commonly used for Bartter syndrome?
What treatment is commonly used for Bartter syndrome?
The luminal side of the Thick Ascending Loop of Henle is responsible for transporting Na⁺, K⁺, and _____ ions.
The luminal side of the Thick Ascending Loop of Henle is responsible for transporting Na⁺, K⁺, and _____ ions.
Match the types of Bartter syndrome with their corresponding features:
Match the types of Bartter syndrome with their corresponding features:
What is the main role of juxtamedullary nephrons?
What is the main role of juxtamedullary nephrons?
Cortical nephrons constitute about 15% of all nephrons in the kidneys.
Cortical nephrons constitute about 15% of all nephrons in the kidneys.
What is the main site of acute tubular necrosis?
What is the main site of acute tubular necrosis?
The outer medullary collecting duct is part of the __________.
The outer medullary collecting duct is part of the __________.
Match the types of renal issues with their characteristics:
Match the types of renal issues with their characteristics:
From which embryonic structure are the collecting ducts derived?
From which embryonic structure are the collecting ducts derived?
What percentage of nephrons are juxtamedullary nephrons?
What percentage of nephrons are juxtamedullary nephrons?
Pre-renal causes of renal failure arise from issues within the kidney itself.
Pre-renal causes of renal failure arise from issues within the kidney itself.
What is the origin of the proximal tubule (PT) in the nephron?
What is the origin of the proximal tubule (PT) in the nephron?
The spongy urethra is derived from the mesonephric duct.
The spongy urethra is derived from the mesonephric duct.
What two structures make up the renal corpuscle?
What two structures make up the renal corpuscle?
The ________ urethra is formed from the pelvic part of the definitive urogenital sinus.
The ________ urethra is formed from the pelvic part of the definitive urogenital sinus.
Match the parts of the nephron to their corresponding segments:
Match the parts of the nephron to their corresponding segments:
What is the primary defect in Type-1 RTA?
What is the primary defect in Type-1 RTA?
Phosphorus loss in urine is significant in Type-1 RTA.
Phosphorus loss in urine is significant in Type-1 RTA.
What hormonal condition is typically severe in Type-1 RTA?
What hormonal condition is typically severe in Type-1 RTA?
In Type-1 RTA, the required HCO3 for treatment is between ___ and ___ mEq/kg/day.
In Type-1 RTA, the required HCO3 for treatment is between ___ and ___ mEq/kg/day.
Match the following features with RTA Type-1 and Type-2:
Match the following features with RTA Type-1 and Type-2:
Flashcards are hidden until you start studying
Study Notes
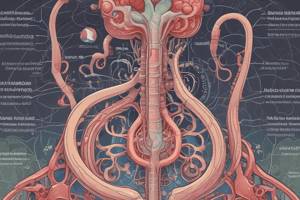
Gross Anatomy of Kidney
- Papillary necrosis can be medullary or papillary.
- Medullary type papillary necrosis shows a ball on tree appearance.
- Papillary type papillary necrosis shows a lobster claw appearance.
- Renal abscess is a complication of UTI and has a poor prognosis.
Childhood UTI Investigation Protocol
- Complicated UTI requires treatment for two weeks.
- Ultrasound should be performed to look for abnormalities.
- CAKUT anomalies should be assessed, such as double pelvis or duplicated ureter.
- Voiding cystourethrography (VCU/MCU) is used to evaluate vesicoureteric reflux (VUR) and posterior urethral valve (in males).
- If VUR is present, a DMSA scan is used to determine the degree of scarring.
- DTPA scan is used to determine the glomerular filtration rate of each kidney separately.
Cortical Collecting Duct
- The cortical collecting duct is lined with four types of cells: P-cell, α-Intercalated cells, β-1 cells, and an unnamed cell.
- P-cells play a role in potassium and hydrogen ion reabsorption, along with sodium and water reabsorption through ENaC channels.
- Aldosterone acts on the basolateral membrane of P-cells.
Pathology - Hypoaldosteronism
- Hypoaldosteronism is also known as Renal tubular acidosis type IV (RTA-IV).
- It is characterized by hyperkalemia without renal failure.
- True hypoaldosteronism can be hyporeninemic or hyperreninemic.
Hyporeninemic Hypoaldosteronism
- Caused by reduced renin and aldosterone levels.
- Common causes include NSAIDs, β-blockers, aliskiren, diabetes mellitus, and prorenin to renin deficiency.
Hyperreninemic Hypoaldosteronism
- Caused by increased renin but decreased aldosterone levels.
- Common causes include adrenal insufficiency (Addison's disease) and drugs like ACE inhibitors, ARBs, aldosterone synthase inhibitors, heparin, and ketoconazole.
Acquired Pseudo hypoaldosteronism (PHA)
- Caused by chronic tubular interstitial fibrosis, vesico-urethral reflux, obstructive nephropathy, and drugs producing fibrosis like calcineurin inhibitors.
Inherited Pseudo hypoaldosteronism (PHA)
- Includes PHA-type-1, PHA-type-2, and PHA-type-a.
Aldosterone Receptor Blockers
- Spironolactone, eplerenone, and ENaC channel blockers like amiloride, triamterene, trimethoprim, pentamidine.
- Excessive aldosterone leads to metabolic alkalosis and hypokalemia.
- Conn's syndrome is a condition caused by excessive aldosterone production.
Proximal Convoluted Tubule
- The proximal convoluted tubule (PCT) is responsible for the maximum reabsorption of all ions except magnesium.
Transporters
- Symport transporter systems in the PCT include sodium-dependent amino acid transporter, sodium-dependent glucose transporter (SGLT-2), and sodium-dependent phosphate transporter type II.
- Damage to the PCT leads to phosphorus loss and Rickets.
- Antiport system in the PCT includes sodium-hydrogen antiport.
- Passive paracellular transport occurs between cells.
Pathology of Type-1 / Distal RTA
- Type-1 RTA is a type of distal renal tubular acidosis.
- It is characterized by a defect in the activity of the α-1 cell.
Physiology of α-1 Cell
- The luminal membrane of α-1 cells allows the movement of hydrogen and potassium ions.
- The basolateral membrane contains carbonic anhydrase (-11), H-K ATPase, and H ATPase.
Physiology of β-1 Cell
- The luminal membrane of β-1 cells facilitates the movement of bicarbonate ions.
- The basolateral membrane contains pendrin channel and anion exchanger.
Pathology of Type-1 / Distal RTA
- Inherited: Autosomal dominant defects in anion exchanger or autosomal recessive defects in H+ ATPase or H+/K+ ATPase.
- Acquired: Sjogren's syndrome (most common), drugs like amphotericin Band toluene, and diseases like primary biliary cirrhosis and systemic lupus erythematosus.
Clinical Manifestations of Type-1 / Distal RTA
- Most common in children.
- Normal renal function tests.
- Inability to acidify urine (urine pH > 5.5 for 3 consecutive days).
- Significant normal anion gap metabolic acidosis (NAGMA) (HCO3- 10-12 mEq/L).
- Increased calcium reabsorption from bone leading to hypercalciuria and stone formation (CaP04), medullary nephrocalcinosis, and renal rickets.
- Hypocitraturia and stones.
- Salt and water wasting leading to secondary hyperaldosteronism and hypokalemia.
Nephrology
- The collecting part of the nephron is the active space for urine concentration and includes the connecting tubule, cortical collecting duct, outer medullary collecting duct, and inner medullary collecting duct.
- Cortical nephrons are short-looped and responsible for a lesser role in urine concentration.
- Juxtamedullary nephrons are long-looped and play a major role in urine concentration.
Approach to Renal Failure
- Non-CKD: Occurs within hours to days and typically involves tubulointerstitial causes like acute tubular necrosis or tubular injury.
- CKD: Chronic kidney disease involves a decrease in the number of functional nephrons over days to weeks.
- Pre-renal causes: Decreased blood flow to the kidneys.
- Post-renal causes: Obstruction in the urinary tract.
Global Dysfunction of PCT (Fanconi Syndrome / Type-a RTA / Proximal RTA)
- The PCT can be affected by both inherited and acquired causes.
Inherited Causes
- Cystinosis: Most common in children.
- Galactosemia.
- Wilson's disease: Most common in adolescents.
Acquired Causes
- Drugs: Most common in adults.
- Multiple myeloma: Most common in the elderly.
Clinical Features of Fanconi Syndrome
Cardinal Manifestations
- Phosphorus loss leads to renal rickets.
- Normal renal function tests with minimal proteinuria.
- Euglycemic glycosuria.
- Wasting/Growth retardation due to amino acid loss in urine.
- Normal anion gap metabolic acidosis (NAGMA) due to HCO3- loss in urine.
- Salt and water depletion leading to secondary RAAS activation and hypokalemia.
Other Features
- Hypouricemia.
- Hypocarnitinemia.
- Polyuria.
- Dehydration.
- Minimal proteinuria.
Loop of Henle (TALH)
- The thick ascending loop of Henle (TALH) is responsible for the reabsorption of sodium, potassium, and chloride.
- The Na⁺-K⁺-2Cl⁻ transporter is located on the luminal membrane of the TALH.
Pathology - Bartter Syndrome
- Bartter syndrome is a genetic disorder characterized by a defect in the Na⁺-K⁺-2Cl⁻ channel.
Symptoms of Bartter Syndrome
- Severe salt wasting leading to polyuria and failure to thrive.
- Secondary RAAS activation with prostaglandin-mediated loss of potassium and hydrogen ions, leading to hypokalemia, metabolic alkalosis, hypercalciuria, renal stones, hypomagnesemia, and normal to low blood pressure.
Types of Bartter Syndrome
- Type I (mc): Children, maternal, polyhydramnios.
- Type II: Children.
- Type III/classical: Adults.
- Type IV: Present with sensorineural hearing loss (SNHL).
- Type V: Autosomal dominant (AD), Defect in calcium-sensing receptor, hypocalcemia.
Treatment of Bartter Syndrome
- Indomethacin.
Nephrology - 716
- The document describes different types of papillae and grades of a medical condition, likely related to the kidneys.
Papillae Types
- Composite papillae: Flat/concave surface, round/oval opening, open gaping orifices, allowing reflux.
- Simple conical papillae: Slit-like orifices (closed), cone-shaped and do not allow reflux.
Asymmetric Involvement of Kidneys
- Vesicoureteral reflux (VUR).
- Renal artery disease.
Tubular Anatomy
- The nephron has various parts with distinct embryological origins.
Embryological Origin
- Bladder: Cloaca (primitive rectum), except trigone: mesonephric duct (mesodermal).
- Prostate: Primitive urogenital sinus (UG sinus).
- Urethra: Prostatic urethra up to opening of ejaculatory duct: vesico-ureteric canal. Membranous urethra and remaining prostatic urethra: Pelvic part of definitive UG sinus. Spongy urethra: Cephalic part of UG sinus.
- Rectum: Primitive rectum (Cloaca).
- Anal canal: Up to pectinate line: cloaca, below pectinate line: Anal pit.
Excretory Part
- Origin: Nephrogenic cord, derived from the urogenital ridge.
Renal Corpuscle
- Glomerulus + Bowman's capsule.
Tubules
- Proximal convoluted tubule (Pars convoluta) S₁ + S₂
- Proximal straight tubule (Pars recta) S₃
- Thin descending limb of loop of Henle
- Thin ascending limb of loop of Henle
- Thick ascending limb of loop of Henle (Distal straight tubule)
- Distal convoluted tubule
- Macula densa
Difference Between RTA-1 and RTA-2
| Feature | RTA Type-1 / Distal | RTA Type-2 / Proximal |
|---|---|---|
| Defect Site | a-1 Cell | Global PCT dysfunction |
| Defect | H+/K+ATPase, Anion exchanger | |
| Phosphorus loss in urine | No | Significant |
| Ca+ loss in urine | Significant | Due to Ca+ loss |
| Rickets | Severe | Due to phosphorus loss |
| NAGMA | Severe | Mild |
| Secondary hyperaldosteronism | Severe | Mild |
| Hypokalemia | Severe | Mild |
| Aminoaciduria | No | Significant |
| Hypocitraturia | Present | Absent |
| Required HCO3 for treatment | 2-4 mEq/kg/day | 10-15 mEq/kg/day |
Unnamed Cells
- The unnamed cells are influenced by ADH and contain aquaporin channels.
- These cells are involved in the counter current exchanger and free water reabsorption.
Urine Anion Gap
- The urine anion gap can be used to differentiate between RTA and VIPoma.
- Formula: Na+ + K+ + UC (unmeasured cation) = Cl- + UA (unmeasured anion).
- Urine anion gap = Na+ + K+ - Cl- = UA - UC.
- Positive urine anion gap indicates RTA, while negative urine anion gap suggests VIPoma.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.