Podcast
Questions and Answers
Which of the following mechanisms is NOT a typical way bacteria develop resistance to antimicrobials?
Which of the following mechanisms is NOT a typical way bacteria develop resistance to antimicrobials?
- Producing enzymes that degrade antibiotics.
- Upregulating antimicrobial efflux pumps.
- Altering the site of antimicrobial action.
- Increasing viral replication within the cell. (correct)
A certain antimicrobial drug inhibits bacterial growth but doesn't kill the bacteria. How would this drug be classified?
A certain antimicrobial drug inhibits bacterial growth but doesn't kill the bacteria. How would this drug be classified?
- Fungicidal
- Virucidal
- Bacteriostatic (correct)
- Bactericidal
Why is combination therapy, involving multiple drugs, typically used in the initial treatment of tuberculosis (TB)?
Why is combination therapy, involving multiple drugs, typically used in the initial treatment of tuberculosis (TB)?
- To reduce the duration of treatment.
- To enhance patient compliance.
- To lower the likelihood of developing resistance. (correct)
- To minimize potential side effects.
Penicillin's effectiveness against bacteria is due to its ability to:
Penicillin's effectiveness against bacteria is due to its ability to:
Why are aminoglycosides, like tobramycin (TOBI), sometimes administered via inhalation for patients with cystic fibrosis?
Why are aminoglycosides, like tobramycin (TOBI), sometimes administered via inhalation for patients with cystic fibrosis?
What does the Gram stain procedure differentiate bacteria into?
What does the Gram stain procedure differentiate bacteria into?
Which of the following best describes the mechanism of action of antivirals (excluding antiretrovirals)?
Which of the following best describes the mechanism of action of antivirals (excluding antiretrovirals)?
Vancomycin is typically used to treat infections caused by gram-positive bacteria. Why is it often used as a drug of last resort?
Vancomycin is typically used to treat infections caused by gram-positive bacteria. Why is it often used as a drug of last resort?
The outcome of antimicrobial therapy is LEAST dependent on which of the following factors?
The outcome of antimicrobial therapy is LEAST dependent on which of the following factors?
A drug is described as exhibiting time-dependent killing. What does this suggest about its effectiveness?
A drug is described as exhibiting time-dependent killing. What does this suggest about its effectiveness?
Flashcards
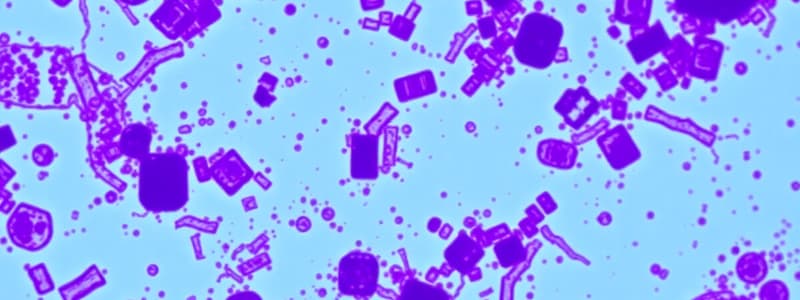
Gram stain
Gram stain
A stain used to differentiate bacteria into two major classes based on their cell wall structure: gram-positive (purple) and gram-negative (pink).
Bacteriostatic drugs
Bacteriostatic drugs
Drugs that inhibit bacterial growth without killing the bacteria.
Bactericidal drugs
Bactericidal drugs
Drugs that kill bacteria.
Emerging bacterial pathogens
Emerging bacterial pathogens
Signup and view all the flashcards
Penicillins' mechanism
Penicillins' mechanism
Signup and view all the flashcards
TB treatment
TB treatment
Signup and view all the flashcards
First-line TB drugs
First-line TB drugs
Signup and view all the flashcards
Antivirals action
Antivirals action
Signup and view all the flashcards
Vancomycin
Vancomycin
Signup and view all the flashcards
Study Notes
- The Gram stain is the simplest and most common preparation.
- Gram stain designates bacteria into two major classes: gram-positive (stain purple) and gram-negative (stain pink).
- Bacteria stain differently depending on the structural components of their cell wall which affects their susceptibility to antimicrobials.
- Drugs that inhibit bacteria growth without killing them are bacteriostatic.
- Bactericidal drugs kill bacteria.
- Virucidal drugs kill viruses, and fungicidal drugs kill fungi.
- Methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus (VRE) are emerging bacterial pathogens that resist many current antimicrobial therapies.
- Mechanisms of bacterial resistance include:
- Production of enzymes that degrade or modify antibiotics.
- Alteration of bacterial cell walls or membranes.
- Upregulation of antimicrobial efflux pumps.
- Alteration of the site of antimicrobial action.
- Penicillins inhibit cell wall synthesis and exert effects by binding to enzymes located within the cell wall.
- Penicillins prevent the cross-linking of the peptidoglycan structure necessary for cell wall development.
- Penicillins are bactericidal, exhibit time-dependent killing, and can act synergistically with aminoglycosides against some bacteria.
- Penicillins inhibit cell wall synthesis to kill bacteria but have no effect on viral disease.
- Treatment of TB consists of multiple antibiotic regimens for 6 to 12 months.
- Single-agent regimens should never be used for TB treatment because of the high likelihood of developing resistance.
- Treatment failures often result from poor patient compliance and resistance to antibiotics.
- Drugs used in TB treatment are categorized as first-line or second-line agents based on their efficacy and side-effect profiles.
- Initial therapy usually involves isoniazid, pyrazinamide, rifampin, and ethambutol.
- The outcome of antimicrobial therapy depends on host factors, susceptibility or resistance to the antimicrobial, and pharmacodynamics.
- Drugs used in the treatment of tuberculosis can be categorized as either first-line or second-line agents depending on their efficacy and side-effect profiles.
- Initial therapy generally involves a combination of isoniazid, pyrazinamide, rifampin, and ethambutol.
- Vancomycin is a glycopeptide antibiotic active against gram-positive bacteria.
- Vancomycin is not active against gram-negative bacteria.
- Vancomycin use has increased recently because of the emergence of MRSA.
- Antivirals (excluding antiretrovirals) mimic nucleosides and inhibit DNA synthesis.
- Aminoglycosides like tobramycin (TOBI) are administered via inhalation to control Pseudomonas aeruginosa infections in patients with cystic fibrosis because of low drug concentrations in bronchial secretions.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.