Podcast
Questions and Answers
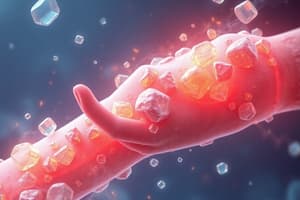
Gout is characterized by the deposition of what type of crystals in the joints and tissues?
Gout is characterized by the deposition of what type of crystals in the joints and tissues?
- Calcium oxalate
- Calcium pyrophosphate dihydrate (CPPD)
- Monosodium urate (MSU) (correct)
- Hydroxyapatite
What is the underlying cause of gout?
What is the underlying cause of gout?
- Bacterial infection
- Hyperuricemia (correct)
- Autoimmune disorder
- Osteoarthritis
Which enzyme, when deficient, contributes to hyperuricemia by reducing the conversion of urate to allantoin?
Which enzyme, when deficient, contributes to hyperuricemia by reducing the conversion of urate to allantoin?
- Amylase
- Protease
- Lipase
- Uricase (correct)
Which of the following is a common risk factor for gout?
Which of the following is a common risk factor for gout?
Which joint is most commonly affected in the initial stages of a gout flare?
Which joint is most commonly affected in the initial stages of a gout flare?
Which of the following is a typical characteristic of gout flares?
Which of the following is a typical characteristic of gout flares?
What is the term for the period between gout flares when the patient is asymptomatic?
What is the term for the period between gout flares when the patient is asymptomatic?
Which of the following can trigger a gout flare?
Which of the following can trigger a gout flare?
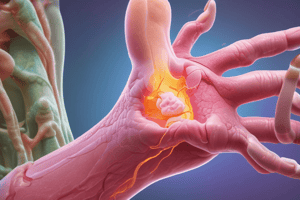
What are tophi?
What are tophi?
Which of the following is a typical characteristic of synovial fluid during a gout flare?
Which of the following is a typical characteristic of synovial fluid during a gout flare?
Why is serum urate level not always reliable during an acute gout flare?
Why is serum urate level not always reliable during an acute gout flare?
Which imaging technique can detect urate crystal deposits in tissues that are useful for the diagnosis of chronic gout?
Which imaging technique can detect urate crystal deposits in tissues that are useful for the diagnosis of chronic gout?
What is the primary goal of acute gout care?
What is the primary goal of acute gout care?
Which class of drugs is commonly used as a first-line treatment for acute gout flares?
Which class of drugs is commonly used as a first-line treatment for acute gout flares?
Which medication is particularly effective for acute gout flares when initiated early?
Which medication is particularly effective for acute gout flares when initiated early?
What is the goal of urate-lowering therapy in the management of gout?
What is the goal of urate-lowering therapy in the management of gout?
When should urate-lowering therapy be considered?
When should urate-lowering therapy be considered?
Which of the following is a first-line urate-lowering drug?
Which of the following is a first-line urate-lowering drug?
What is the mechanism of action of allopurinol?
What is the mechanism of action of allopurinol?
In patients with chronic kidney disease, what adjustment to allopurinol dosage is typically recommended?
In patients with chronic kidney disease, what adjustment to allopurinol dosage is typically recommended?
Which genetic marker is associated with an increased risk of severe cutaneous adverse reactions (SCARs) to allopurinol?
Which genetic marker is associated with an increased risk of severe cutaneous adverse reactions (SCARs) to allopurinol?
Which of the following is a second-line urate-lowering therapy?
Which of the following is a second-line urate-lowering therapy?
Why are urate-lowering drugs generally not initiated during an active gout flare?
Why are urate-lowering drugs generally not initiated during an active gout flare?
What is the recommended approach for managing patients when starting urate-lowering therapy?
What is the recommended approach for managing patients when starting urate-lowering therapy?
A patient with a history of cardiovascular disease is prescribed febuxostat. What precaution should be taken?
A patient with a history of cardiovascular disease is prescribed febuxostat. What precaution should be taken?
Which serum uric acid level defines hyperuricemia?
Which serum uric acid level defines hyperuricemia?
Which of the following dietary factors increases the risk of gout?
Which of the following dietary factors increases the risk of gout?
Which of the following features is most indicative of gout?
Which of the following features is most indicative of gout?
What is the primary nonpharmacological management for acute gout attacks?
What is the primary nonpharmacological management for acute gout attacks?
What type of crystal is used to confirm a diagnosis of gout?
What type of crystal is used to confirm a diagnosis of gout?
Which prophylactic medication is indicated during initiation of urate-lowering therapy?
Which prophylactic medication is indicated during initiation of urate-lowering therapy?
What should be ruled out before intra-articular injection of corticosteroids?
What should be ruled out before intra-articular injection of corticosteroids?
When is urate-lowering therapy is NOT indicated?
When is urate-lowering therapy is NOT indicated?
Which urate-lowering agent is contradicted in with azathioprine?
Which urate-lowering agent is contradicted in with azathioprine?
Which is the preferred first-line urate-lowering therapy (ULT) agent for all patients?
Which is the preferred first-line urate-lowering therapy (ULT) agent for all patients?
If the patient has not achieved SUA target, continues to have gout flares, and/or tophi are not resolving with XOI, uricosurics, and other interventions, what is should be considered?
If the patient has not achieved SUA target, continues to have gout flares, and/or tophi are not resolving with XOI, uricosurics, and other interventions, what is should be considered?
Which is an accurate maintenance of fluid hydration to maintain while taking Allopurinol?
Which is an accurate maintenance of fluid hydration to maintain while taking Allopurinol?
What is the initial dose of Colchicine/Colcrys for Initial Flare, followed by?
What is the initial dose of Colchicine/Colcrys for Initial Flare, followed by?
What is a diagnostic test for gout?
What is a diagnostic test for gout?
Which statement is correct?
Which statement is correct?
Flashcards
What is Gout?
What is Gout?
Gout is a metabolic condition marked by episodic inflammatory arthritis with disabling pain.
Cause of Gout
Cause of Gout
Increased body pool of urate from chronic hyperuricemia, leading to crystal formation in joints.
Gout Flare Symptoms
Gout Flare Symptoms
Joint pain rapidly becomes warm, red, tender, and substantially swollen, mimicking cellulitis.
Triggers of Gout Flares
Triggers of Gout Flares
Signup and view all the flashcards
Complications of Untreated Gout
Complications of Untreated Gout
Signup and view all the flashcards
Diagnosing Gout
Diagnosing Gout
Signup and view all the flashcards
MSU Crystals Under Polarized Light
MSU Crystals Under Polarized Light
Signup and view all the flashcards
Baseline Tests for Gout
Baseline Tests for Gout
Signup and view all the flashcards
Ultrasound Sign of Gout
Ultrasound Sign of Gout
Signup and view all the flashcards
Acute Gout Treatment
Acute Gout Treatment
Signup and view all the flashcards
Non-Pharmacologic Gout Treatment
Non-Pharmacologic Gout Treatment
Signup and view all the flashcards
Goal of Urate-Lowering Therapy
Goal of Urate-Lowering Therapy
Signup and view all the flashcards
Lifestyle Changes for Gout
Lifestyle Changes for Gout
Signup and view all the flashcards
Severe Allopurinol Reactions
Severe Allopurinol Reactions
Signup and view all the flashcards
Allopurinol Mechanism
Allopurinol Mechanism
Signup and view all the flashcards
Uricosuric Agents
Uricosuric Agents
Signup and view all the flashcards
Urate-Lowering During Flare?
Urate-Lowering During Flare?
Signup and view all the flashcards
Anti-inflammatory Prophylaxis
Anti-inflammatory Prophylaxis
Signup and view all the flashcards
Dietary Risk Factors for Gout
Dietary Risk Factors for Gout
Signup and view all the flashcards
Acute Gout Pain
Acute Gout Pain
Signup and view all the flashcards
Alcohol and Gout
Alcohol and Gout
Signup and view all the flashcards
Study Notes
- Gout is a hyperuricemic metabolic condition
- It manifests as episodic inflammatory arthritis with disabling pain
- Gout is common among middle-aged to elderly men and postmenopausal women
- Gout stems from an increased body pool of urate
- Chronic hyperuricemia leads to urate supersaturation
- Monosodium urate (MSU) crystal formation and deposition occurs within joints and connective tissue
- Untreated gout progresses to chronic gouty arthritis
- Persistent synovitis and erosive deformities occur due to MSU crystal deposition
- Humans spontaneously develop gout because they lost uricase in evolution
- Uricase converts urate into water-soluble allantoin
- Chronic hyperuricemia is a prerequisite for gout development
- Hyperuricemic individuals develop gout during their lifetime at a minority rate
- At physiologic pH, uric acid exists as urate, the ionized form, due to its weak acidic property (pKa, 5.8)
- Hyperuricemia and gout are associated with cardiovascular-metabolic comorbidities
Risk factors
- Insulin resistance syndrome
- Obesity, hypertension, type 2 diabetes
- Myocardial infarction, stroke, and urate nephrolithiasis
- Modifiable risk factors include obesity, Western diet, alcohol, sedentary lifestyle, and diuretics
Clinical Manifestations
- Early sign is acute recurrent gout flares
- Typically, one joint is initially affected, though oligo- and polyarticular flares can develop
- The metatarsophalangeal joint of the first toe (podagra) is involved in 70–90% of cases
- Followed by tarsal joints, ankles, and knees
- Finger, wrist, and elbow joints can also be involved, particularly in elderly patients or advanced disease
- Gout flares often begin at night to early morning
- Affected joints become warm, red, tender, and substantially swollen
- The clinical appearance mimics cellulitis (pseudocellulitis)
- Typical flares subside spontaneously within 1-2 weeks
- Intercritical gout is the interval with no residual symptoms until the next episode for most patients
- Triggers include purine-rich food, alcohol, diuretic use, initial introduction of urate-lowering therapy, local trauma, and medical illnesses
- Congestive heart failure and respiratory hypoxic conditions can trigger gout
Untreated Gout
- Chronic gouty arthritis can develop after years of gout flares
- Often associated with ongoing synovitis, subcutaneous tophi, deformity, and bony destruction
- Less commonly, chronic gouty arthritis is the only manifestation
- Rarely, gout can manifest only as tophi
- Women represent only 5-20% of all patients with gout
- Most women with gout are postmenopausal and elderly and tend to have osteoarthritis, hypertension, or mild renal insufficiency
- Premenopausal gout is rare
Diagnosis
- Presumptive diagnosis should be confirmed by needle aspiration of involved joints or tophaceous deposits
- Septic arthritis, other crystal-associated arthropathies, palindromic rheumatism, and psoriatic arthritis can mimic presentations
- Needle-shaped MSU crystals are present both intracellularly and extracellularly during acute flares
- Under compensated polarized light, MSU crystals show bright, negative birefringence
- Synovial fluid appears cloudy due to increased leukocytes (e.g., from 5000–75,000/μL)
- Large amounts of crystals occasionally produce thick, pasty, chalky joint fluid or drainage from distended tophus
- Joint fluid is often stained and cultured for potential septic arthritis because bacterial infection can coexist with MSU crystals
- MSU crystals can be demonstrated in the first metatarsophalangeal joint and knees not acutely involved with gout
- Arthrocentesis of these joints is useful for gout diagnosis between flares
- Serum urate levels can be normal or low at the time of an acute flare
- Inflammatory cytokines' uricosuric property (e.g., IL-6) can lower the level by ~2 mg/dL
- Serum urate values are almost always elevated at some time in a gout patient's lifetime
- Historical or postflare serum urate values are a diagnostic clue or therapeutic target to urate-lowering therapy
- Serum creatinine, liver function tests, hemoglobin, white blood cell (WBC) count, hemoglobin A1c, and serum lipids are obtained at baseline
- Lab tests are performed to assess risk factors and comorbidities and monitored for potential adverse effects
Radiographic Features
- In plain radiography, cystic changes, well-defined erosions with sclerotic margins (often with overhanging bony edges), and soft tissue masses are features
- Findings may be absent in earlier stages of gout
- Musculoskeletal ultrasound can timely aid diagnosis by revealing a double-contour sign overlying the articular cartilage
- This signifies MSU deposition
- Dual-energy computed tomography (CT) utilizes two different energy beams
- Identifies MSU based on its chemical composition to indicate MSU crystal presence
Treatment for Acute Gout
- Nonpharmacologic measures, such as ice pack application and rest, can be helpful
- The mainstay of acute gout care is anti-inflammatory drugs, colchicine, and glucocorticoids
- Choice depends on the patients' comorbidities, concurrent medications, and previous response if recurrent flares
- Early initiation of antiinflammatories helps abort or reduce the severity of flares
- Provide recurrent flare patients with a supply of medications ready to start at the first sign
- NSAIDs are used most often in individuals without complicating comorbidities
- Full anti-inflammatory doses of NSAIDs are effective for most patients
- Oral colchicine is also effective, particularly if used early in a gout flare
- Low-dose regimen (1.2 mg, then 0.6 mg in 1 h, then subsequent-day dosing) is as effective as higher-dose regimens
- Colchicine is eliminated through P-glycoprotein (MDR1) in the liver, small intestine, and kidneys via enteric and hepatic cytochrome P450 3E4 (CYP3A4)
- The dose of Colchicine is reduced among patients with renal disease or when used with P-glycoprotein or CYP3A4 inhibitors
- Use caution with clarithromycin or tacrolimus due to potential liver impairment
- Glucocorticoids given as an intramuscular injection or orally (e.g., prednisone, 30-50 mg/d tapered) can be effective
- Intraarticular glucocorticoid injection is effective and well tolerated for a single joint or a few joints involved
- Anakinra is useful with the central role of the inflammasome and IL-1β in flares when other treatments are contraindicated
Urate-Lowering Therapy
- Ultimate control requires correction of chronic hyperuricemia
- Normalize serum urate to a subsaturation point (<300-360 µmol/L [5.0-6.0 mg/dL]) to prevent recurrent gout flares and eliminate tophi are critical
- This entails a lifelong commitment to urate-lowering regimens
- Consider urate-lowering drug therapy when hyperuricemia cannot be corrected by risk factor interventions
- Risk factor interventions include control of body weight, healthy diet, limitation of alcohol, decreased fructose-rich foods, and avoidance of thiazide and loop diuretics
- The decision to initiate urate-lowering drug therapy considers the number of gout flares, severity and duration of flares, quality of life, or willingness to commit
- Initiate urate-lowering therapy in any patient who already has subcutaneous tophi or chronic gouty arthritis or known uric acid stones
- Allopurinol, a xanthine oxidase inhibitor, is the first-line urate-lowering drug
- It can be given in a single morning dose, starting at 100 mg daily or less and titrating up (to 800 mg daily)
- Target serum urate level is <5-6 mg/dL (i.e., a subsaturation point of MSU crystals)
- The starting allopurinol dose should be lowered in patients with chronic kidney disease (CKD)
- For example, start at 50 mg daily and titrate up slowly with a estimated glomerular filtration rate of 30-45 mL/min
- Starting at a low dose and titrating up reduces the risk of severe cutaneous adverse reactions (SCARs), Stevens-Johnson syndrome and toxic epidermal necrolysis
- It also reduces the risk of gout flares associated with rapid serum urate reduction due to introduction of urate-lowering therapy
- Mild cutaneous reactions can develop in ~2% of users and allopurinol is generally well tolerated
- SCARs to allopurinol are rare but can be life-threatening, and thus, appropriate precaution is advised
- Risk factors include CKD, higher allopurinol initial dosing (>100 mg daily in CKD patients), and HLA-B*5801 carriage
HLA-B*5801 risks
- Older age and female sex are also associated with a higher risk of SCARs
- HLA-B*5801 carriage rate is substantially higher among Southeast Asians (except Japanese), Pacific Islanders, and blacks than whites or Hispanics
- Leading to racial disparity in the risk of SCARs
- Screening for HLA-B*5801 should be performed before starting allopurinol in those Asians and blacks
- An alternative urate-lowering agent should be administered if patients carry HLA-B*5801 allele
- Febuxostat is a newer xanthine oxidase inhibitor metabolized by glucuronide formation and oxidation in the liver
- Febuxostat is considered to not require dose adjustment in moderate to severe CKD and has also been used in patients who carry the HLA-B*5801 allele
- Uricosuric agents such as probenecid are considered second-line urate-lowering therapies
- Uricosuric agents can be used in patients with good renal function either alone or in combination with xanthine oxidase inhibitors such as allopurinol
- Probenecid can be started at 250 mg twice daily and increased gradually as needed up to 3 g/d to achieve and maintain a target serum urate level
- Probenecid is generally not effective in patients with serum creatinine levels >177 µmol/L (2 mg/dL)
- Benzbromarone (not available in the United States) is another uricosuric drug effective in patients with CKD
- Thiazide and loop diuretics increase serum urate levels and trigger gout attacks
- Losartan, amlodipine, fenofibrate, and sodium-glucose cotransporter-2 inhibitors are common comorbidity drugs that also help lower serum urate levels
- Pegloticase is a pegylated uricase available for patients who do not tolerate or fail full doses of other treatments
- Urate-lowering drugs are not initiated during active ongoing gout flares
- Urate-lowering drugs can worsen the flare by acutely lowering serum urate levels
- Urate-lowering therapy can be started during the resolution phase of or after a gout flare
- Urate-lowering medications can be given with anti-inflammatory prophylaxis (e.g., colchicine 0.6 mg one to two times daily or naproxen 250 mg twice daily)
- This reduces the risk of flares that often occur with the initiation of urate-lowering therapy
- Paradoxical flares are inflammatory reactions to MSU crystals shed from dissolution of organized MSU deposits (synovial tophi) induced by rapid serum urate reduction
- Faster urate reduction has been associated with a higher risk of flares in clinical trials of urate-lowering drugs
- Continuing concomitant anti-inflammatory prophylaxis is usually recommended until the patient is normouricemic and without gouty attacks for 3-6 months or tophi disappear
Description
- Gout is a form of inflammatory arthritis characterized by recurrent attacks of acute joint pain and swelling
- The attacks happen due to the deposition of monosodium urate crystals in joints and surrounding tissues
- Definition of hyperuricemia: serum uric acid levels above 6.8 mg/dL, the saturation point of urate in body fluids
- Gout typically affects peripheral joints
- The first metatarsophalangeal joint is the most commonly involved site in initial attacks
- Untreated gout can lead to chronic arthropathy, tophi formation, and increased risk of cardiovascular and renal complications
Etiology
- Gout results from the accumulation and crystallization of uric acid in joints and tissues
- This crystallization is due to either overproduction or underexcretion of uric acid, or a combination of both
- Elevated uric acid levels can occur due to increased purine intake, enhanced purine synthesis, or decreased renal excretion
- The acute gout attack is triggered by the release of urate crystals from deposits or newly formed crystals
- This leads to an intense inflammatory response mediated by neutrophils and pro-inflammatory cytokines
- Genetic factors influence the risk of developing gout
Incidence
- Estimated global prevalence of gout: 1-4% of the adult population
- Higher rates occur in developed countries
- In the United States, gout affects approximately 4% of adults
- Men are 3-4 times more likely to develop the condition than women
Risk factors for gout
- Men are at higher risk, with peak onset between 30-50 years; women's risk increases post-menopause
- High intake of purine-rich foods (e.g., red meat, seafood), alcohol (especially beer), and fructose-sweetened beverages increases risk
- Obesity and Metabolic Syndrome is associated with increased uric acid production and decreased excretion
- Alcohol use or abuse may trigger an episode of gout
Prevention
- Maintain a healthy weight through balanced diet and regular physical activity
- Limit intake of purine-rich foods, alcohol (especially beer), and sugar-sweetened beverages
- Stay well-hydrated to promote uric acid excretion
- Manage comorbidities such as hypertension, diabetes, and hyperlipidemia
Assessment Findings
- Sudden onset of severe pain, often in the first metatarsophalangeal joint (podagra)
- The affected joint appears red, swollen, and warm to touch
- Limited Range of Motion is present
- Tophi formation
- Low-grade fever, fatigue, and malaise may accompany acute attacks
Assessment tools and Grading
- Used for diagnosis and classification of gout
- Gout Classification Criteria (ACR/EULAR)
- Assesses disease activity and response to treatment
- Gout Activity Score (GAS)
- Measures the extent of tophaceous deposits in chronic gout
- Tophus Burden Assessment
Differential Diagnosis
- Acute monoarthritis, hyperuricemia
- Gout - Synovial fluid crystal analysis
- Fever, single hot swollen joint
- Septic Arthritis - Joint aspiration, culture
- Similar presentation, older patients
- Pseudogout - Synovial fluid CPPD crystals
- Symmetric polyarthritis, morning stiffness
- Rheumatoid Arthritis - RF, anti-CCP antibodies
Diagnostic Studies and Possible Findings
- Presence of negatively birefringent, needle-shaped urate crystals under polarized light microscopy is diagnostic
- Synovial Fluid Analysis
- Elevated levels (>6.8 mg/dL), though may be normal during acute attacks
- Serum Uric Acid
- Elevated ESR and CRP during acute attacks
- Inflammatory Markers
- May show soft tissue swelling acutely; punched-out erosions with overhanging edges in chronic gout
- X-rays
- Can detect urate crystal deposits in tissues, useful for diagnosing chronic gout
- Dual-Energy CT
- Normal uric acid levels are common during an acute attack
- Always look at the clinical presentation in conjunction with diagnostic studies
Treatment Prioritization
- Manage acute gout attacks to relieve pain and inflammation
- Implement urate-lowering therapy to prevent recurrent attacks and complications
- Address modifiable risk factors and comorbidities
- Provide patient education on lifestyle modifications and medication adherence
Nonpharmacological Management
- Rest and elevate the affected joint during acute attacks
- Apply ice to reduce pain and inflammation
- Implement dietary modifications to reduce purine intake
- Encourage weight loss in overweight/obese patients
Pharmacological Management
- 1st Line for Acute Attacks:
- Naproxen 500 mg twice daily or Indomethacin 50 mg three times daily for 3-5 days NSAIDs
- 1.2 mg initially, followed by 0.6 mg one hour later, then 0.6 mg daily for 7-10 days
- Colchicine
- Prednisone 30-40 mg daily, tapered over 7-10 days (for those unable to take NSAIDs or colchicine)
- Corticosteroids
- Urate-Lowering Therapy (for frequent attacks or chronic gout):
- Start at 100 mg daily, titrate up to achieve serum uric acid <6 mg/dL
- Allopurinol
- Alternative for those intolerant to allopurinol, start at 40 mg daily
- Febuxostat
- Prophylaxis during initiation of urate-lowering therapy:
- Low-dose colchicine (0.6 mg daily) or low-dose NSAIDs for 3-6 months
- Serum uric acid levels, renal function, and liver function tests regularly Monitor
Acute attacks
- Medication management should ideally be initiated within 24 hours of flare onset
- Monotherapy is appropriate using colchicine, oral steroids, NSAIDS, OR COX-2 inhibitors
- If mild to moderate pain
- Combination therapy is appropriate
- If severe polyarticular gout flare
- Reduce dose as soon as symptoms High-dose NSAIDs for 2-5 days with precautions
- Best if initiated within 36 hours of flare onset
- Colchicine
- May be effective if patient cannot tolerate NSAIDs
- Oral or injectable corticosteroids
- May be contributing to hyperuricemia; consider modifying or eliminating as possible
- Review medications patient is taking
- Can provide rapid relief; should be considered if flare involves one or two large joints
- Intra-articular injection of corticosteroids
NSAIDs
- MOA: inhibit cyclooxygenase (COX-1 and COX-2) activity and prostaglandin synthesis
- FDA indication: management of pain and inflammation in acute gouty arthritis
- May cause serious Gl events including bleeding, ulceration, perforation, with or without warning
- Avoid in patients with sulfonamide hypersensitivity
- Use with caution in patients with known or suspected cardiovascular risk factors
- May lead to or worsen hypertension
- May lead to fluid retention or worsen heart failure
- Avoid concomitant use with salicylates
- Use with caution in patients with asthma
- Avoid use in patients with renal disease
- Titrate for effect, 50 mg PO TID until pain resolved
- Indomethacin/Indocin Usual: 50 mg PO BID for shortest duration possible Max: 150 mg/day PO Availability: Caps: 25 mg, 50 mg
- May diminish effect of ACE inhibitors
- Avoid late in pregnancy due to premature closure of ductus arteriosus
- Available by prescription or OTC
- Initial: 500 mg PO BID; titrate for effect
- Naproxen/Naprosyn Availability: Tabs: 250 mg, 375 mg, 500 mg
- Avoid late in pregnancy due to premature closure of ductus arteriosus
- Dose strengths and formulations not necessarily bioequivalent
- Consider when changing formulation
Urate Lowering Agents
- Allopurinol and febuxostat inhibit xanthine oxidase; probenecid inhibits uric acid reabsorption; uricase decreases serum uric acid; colchicine reduces pain and inflammation associated with gout attack
- MOA FDA indication: management of symptoms associated with gout
- All should be accompanied by adequate daily fluid intake
- Allopurinol preferred first-line urate-lowering therapy (ULT) agent for all patients
- A xanthine oxidase inhibitor (XOI) is recommended over probenecid for patients with CKD stage >3
- Concomitant anti-inflammatory prophylaxis therapy for 3-6 months is recommended when initiating ULT
- If a patient is taking a maximum dose of a single XOI and does not achieve SUA target, continues to have gout flares, or tophi are not resolving, consider switching to a different XOI agent prior to adding a uricosuric agent
- If a patient has not achieved SUA target, continues to have gout flares, and/or tophi are not resolving with XOI, uricosurics, and other interventions, consider switching to pegloticase
- Initial: 100-200 mg/day PO
- Allopurinol/Zyloprim Usual: 200-300 mg/day PO Max: 800 mg/day PO Availability: Tabs: 100 mg, 300 mg
- Mild Disease
- Initial: 400-600 mg/day PO
- Usual: 200-300 mg/day PO
- Max: 800 mg/day PO Moderate/Severe Disease
- Maintain adequate fluid hydration
- Baseline BUN/creatinine before initiation
- Monitor CBC, renal and hepatic function at 1 wk, 6 wk, and every 3 months while on allopurinol
- Bone marrow suppression, as well as renal and hepatic impairment, can occur
- Consider starting at a low dose, then titrate to target
- Administered doses >300 mg
- Consider alkaline urine state
- Educate patients about the potential for allopurinol hypersensitivity reaction
- Consider HLA-B*5801 testing before starting allopurinol therapy for populations that have high risk for hypersensitivity reaction
Acute Attack Prevention
- Colchicine/Colcrys
- Initial Flare
- If on dialysis, max dose is 0.6 mg
- May take without regard to meals
- 1.2 mg PO initially, then 0.6 mg 1 hr later; wait 12 hr, then 0.6 mg BID
- Availability: Tabs: 0.6 mg
- Probenecid/Benemid Prevention - 0.6 mg PO BID Initial (post attack) If moderate or severe renal or hepatic dysfunction, treatment course can be repeated no more than once every 2 wk GI side effects common Caution in older adults or debilitated patients Caution with anticoagulants Do not initiate therapy during acute gout attack
- 250-500 mg PO BID (with food) for 7 days; advance to 500 mg PO BID; may increase every 4 wk thereafter Availability: Tabs: 500 mg Max: 2 g PO
Urate-Lowering Agents - FebuxoStat/Uloric
- Initial: 40 mg PO daily
- Max: may increase to 80 mg daily if serum uric acid remains >6 mg/dL after 2 wk therapy
- Initial: 100 mg/day PO; consider 50 mg/day for patients with stage 4 chronic kidney disease
- Increase Dose & Max 6mg: Availability: Tabs: 40 mg, 80 mg Anaphylaxis and infusion reactions can occur
- If attack-free for >6 months, may decrease daily dose (monitor serum urate levels)
- Patients should be adequately hydrated
- Contraindicated in patients receiving azathioprine (Imuran) and mercaptopurine
- High risk for adverse CV events; use with extreme caution
- Consider switching to an alternative ULT agent for patients with a history of CVD or a new CV event
- Indicated for refractory gout
- Prevent Acute Attack If attack-free for >6 - months, may decrease daily dose (monitor -serum urate levels)
- Patients should be, adequately hydrated
- Max dose for initial 6mg; Indications for Consultation
- Preventive therapy includes urate-lowering agents
- Allopurinol Febuxostat Probenecid for patients that have difficulty achieving the goals.
Preventive Agents
- Consider urate lowering therapy in patients
- Prior Stones: Urate renal stones
- CKD Factors: diagnosed with a first gout flare and with stage 3 or greater chronic kidney disease; SUA >9 mg/dL, or urolithiasis; 2 or greater CKD; With tophi
- Agents dosed for long term
Considerations for Preventive Agents:
- Alternate first-line agent: uricosurics increase excretion of uric acid Treat patient to target serum urate level of <6 mg/dL Initiate anti-inflammatory prophylaxis therapy, up to 3-6 months, to avoid mobilization flare when initiating urate-lowering therapy
- Urate-lowering therapy is generally not recommended for patients with asymptomatic hyperuricemia and no prior gout flares or subcutaneous tophi
Consulation or Referral
- Difficult achieveing treatment goals,
- Neurology if issues
- Cardiology Management
Initial Diagnostic Patient Guidance
- Explain nature of the illness and relation to uric acid levels
- Discuss management/ and the prevention
- diet and lifestyle changes
Follow Up
- Make frequent visits to monitor, and assess current attacks
- Expected is a 3-10 day resolution of acute gout
- Treatment can prevent attacks and dissolute over time
- Make sure to reinforce lifestyle, and meds
Complications:
- Joint destruction with topography, renal failure
- CVD issues from increased attacks Overall: There can a reduced life quaitly
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.