Podcast
Questions and Answers
Which of the following best describes the underlying cause of gout?
Which of the following best describes the underlying cause of gout?
- Bacterial infection within the synovial fluid.
- Autoimmune destruction of joint cartilage.
- Deposition of monosodium urate (MSU) crystals in tissues. (correct)
- Reduced blood flow to the affected joint.
Hyperuricemia, a key factor in gout, can arise from what?
Hyperuricemia, a key factor in gout, can arise from what?
- Excess uric acid production, decreased renal excretion, or both.
- Increased metabolism of fatty acids. (correct)
- Overproduction of collagen in joint tissues.
- Increased absorption of calcium in the kidneys.
A patient presents with a painful, swollen first metatarsophalangeal joint. Which condition is most closely associated with these symptoms?
A patient presents with a painful, swollen first metatarsophalangeal joint. Which condition is most closely associated with these symptoms?
- Olecranon bursitis. (correct)
- Carpal tunnel syndrome.
- Achilles tendinitis.
- Podagra.
Tophi, a clinical manifestation of chronic gout, are characterized by what?
Tophi, a clinical manifestation of chronic gout, are characterized by what?
If a definitive diagnosis of gout is desired, what is the best method to use?
If a definitive diagnosis of gout is desired, what is the best method to use?
Which dietary recommendation is LEAST appropriate for a patient trying to manage their gout?
Which dietary recommendation is LEAST appropriate for a patient trying to manage their gout?
Why is Indomethacin avoided in elderly patients?
Why is Indomethacin avoided in elderly patients?
When is it appropriate to start serum urate-lowering therapy (ULT) for a patient with gout?
When is it appropriate to start serum urate-lowering therapy (ULT) for a patient with gout?
A patient with hypertension and gout is prescribed a diuretic. Which diuretic should be AVOIDED?
A patient with hypertension and gout is prescribed a diuretic. Which diuretic should be AVOIDED?
Referral to a rheumatologist is MOST appropriate in which of the following situations?
Referral to a rheumatologist is MOST appropriate in which of the following situations?
Flashcards
What is Gout?
What is Gout?
A systemic metabolic disease resulting from tissue deposition of monosodium urate (MSU) due to prolonged hyperuricemia.
What is Hyperuricemia?
What is Hyperuricemia?
Elevated uric acid levels in the blood, which can lead to the formation of urate crystals in joints and tissues.
Acute Gouty Flare
Acute Gouty Flare
A painful condition with rapid onset, often at night, characterized by warmth, redness, swelling, and decreased range of motion in the affected joint.
What are Tophi?
What are Tophi?
Signup and view all the flashcards
Needle Aspiration
Needle Aspiration
Signup and view all the flashcards
Uricostatic Drugs
Uricostatic Drugs
Signup and view all the flashcards
Lifestyle changes for Gout
Lifestyle changes for Gout
Signup and view all the flashcards
Loop and Thiazide Diuretics
Loop and Thiazide Diuretics
Signup and view all the flashcards
First-line acute gout drugs
First-line acute gout drugs
Signup and view all the flashcards
Serum Urate Lowering Therapy (ULT)
Serum Urate Lowering Therapy (ULT)
Signup and view all the flashcards
Study Notes
- Gout is a systemic metabolic disease.
- It arises from tissue deposition of monosodium urate (MSU) due to prolonged hyperuricemia
- Hyperuricemia results from excess uric acid production, decreased renal excretion, or both
- Gout has four stages: asymptomatic hyperuricemia, acute gouty flares, intercritical gout, and chronic tophaceous gout
Epidemiology
- Gout is the most common inflammatory arthritis in adults.
- About 3.9% of adults in America have gouty arthritis.
- Gout prevalence increases with age, and its incidence is rising in developed countries.
- The male to female ratio of gout is about 4:1.
- Predominant age of gout is 30-50 in men, and over 60 in women.
Risk Factors
- 73% of gout patients have mild to severe renal insufficiency.
- Certain Medications including Diuretics, Low-dose aspirin, Tacrolimus, and Cyclosporine are risk factors
- Comorbidities that are risk factors include obesity, renal disease, hypertension (HTN), and metabolic syndrome.
- High levels of meat and seafood consumption, overeating, and alcohol consumption in men increase the risk.
- Lower body temperature, trauma, surgery, dehydration, and starvation are risk factors.
Clinical Presentation: Acute Gout
- Acute gout involves rapid onset and buildup of pain, reaching maximum within 4-12 hours.
- The first flare often begins at night and can wake the person from sleep
- Hallmark symptoms include intense pain, warmth, redness, tenderness, swelling, and decreased range of motion (ROM)
- Initial episodes are usually monoarticular, commonly affecting the first metatarsophalangeal joint (podagra) in 50% of patients.
- Other joints involves include the insteps, heels, knees, wrists, fingers, and elbows
- Systemic signs such as fatigue, fever, and chills may be present.
- Untreated acute gout can last from several hours to several weeks.
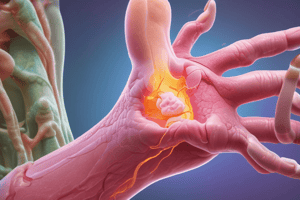
Clinical Presentation: Chronic Tophaceous Gout
- Chronic tophaceous gout typically develops after 5-10 years of acute intermittent gout.
- Characterized by collections of solid urate with chronic inflammatory and destructive changes in connective tissue
- Tophus means "chalk stone” in Latin.
- Tophi appear as firm swellings, usually not painful or tender, and may appear yellow or white
- Common locations for tophi include digits of the hands and feet, olecranon bursa, and helix/antihelix of the ear.
Diagnostic Evaluation
- Definitive diagnosis involves needle aspiration for MSU crystal identification.
- Labs include uric acid levels, complete blood count (CBC), and inflammatory markers.
- Musculoskeletal ultrasound may show a hyperechoic band over anechoic cartilage.
- Dual-energy computed tomography can visualize MSU crystal deposits, but sensitivity is lower in patients with recent-onset disease.
Pharmacologic Management of Acute Gout
- First-line therapy includes NSAIDs (equally effective), administered orally at maximal dosage until 1-2 days post symptom relief; for example, indomethacin 50 mg three times per day.
- Colchicine inhibits microtubule polymerization, preventing neutrophil migration; most effective in the first 12-24 hours of an attack.
- Avoid colchicine in renal and hepatic insufficiency
- Administer 1.2 mg initially, then 0.6 mg one hour later, then 0.6 to 1.2 mg per day
- Corticosteroids are preferred when NSAIDs and colchicine are contraindicated, with a taper to avoid rebound flares.
- Oral, intramuscular, or intra-articular routes of corticosteroids are options, with variable dosing (e.g., Prednisone 40 mg for four days, then 20 mg for four days, then 10 mg for four days).
Chronic Gout Prevention
- Urate-lowering therapy (ULT) should be initiated to prevent recurrences in patients with a history of gout, at least two flares per year (or one per year in person with chronic kidney disease stage 2 or greater), tophi, and a history of nephrolithiasis.
- ULT should be started 6-8 weeks post-flare resolution, at low doses, and increased slowly every 4-6 weeks to reach a serum urate level less than 6mg/dl.
- Monitor serum urate every 2-5 weeks while titrating the dose, then every 6 months.
- ULT should be continued for three to six months after resolution of a gout flare if there are no ongoing symptoms.
- Therapy should continue indefinitely if there are ongoing signs or symptoms, or having one or more tophi on examination.
Treatment of Chronic Gout
- Xanthine oxidase inhibitors are uricostatic drugs that decrease uric acid synthesis.
- Allopurinol (Zyloprim) 100 mg per day initially, except in patients with renal dysfunction; the common effective dosage is 300 mg per day, but higher dosages may be needed.
- Febuxostat (Uloric) 40 mg once per day, may increase up to 80 mg per day if serum uric acid level > 6 mg per dL (357 µmol per L) after two weeks.
Geriatric Considerations
- Avoid loop and thiazide diuretics in patients with HTN and gout, as they can increase uric acid levels.
- Calcium channel blockers and the ARB Losartan are associated with a decreased risk of incident gout.
- Losartan is the only angiotensin receptor blocker with this property.
- Indomethacin is avoided in older adults due to a greater risk of adverse effects compared with other NSAIDs.
- Glucocorticoids are generally tolerated in short-term use for acute attacks in whom NSAIDs or colchicine may pose an increased risk
More Geriatric Considerations
- Contraindications to the use of NSAIDs in older adults are heart failure, renal impairment, or gastrointestinal disease like ulcers.
- Contraindications to colchicine include gastrointestinal intolerance, dosing restrictions in patients with renal and hepatic dysfunction, and potential drug interactions, as well as the high cost of therapy.
Referral
- Rheumatologist consultation is indicated to establish the diagnosis by joint aspiration and MSU crystal identification.
- Indications include drug toxicity or intolerance, if patient develops acute flares with the maximum tolerated treatment, if the diagnosis is in doubt, and if patient is unable to use or tolerate the medication
Follow-up
- Acute gout requires a 1 week follow-up
- Chronic gout requires a 2 month follow-up
Patient Education
- Identification of characteristic crystals
- Education regarding medications: acute gout/to prevent further attacks/chronic gout
- Lifestyle changes: controlling weight, limiting alcohol, limiting meals with meats and fish rich in purines, increasing low-fat dairy consumption, and consuming cherries to control gout
- Patients with chronic gout will require lifetime treatment to lower the uric acid body pool
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Gout is a metabolic disease caused by monosodium urate deposition due to hyperuricemia. Hyperuricemia results from excess uric acid production or decreased renal excretion. Gout has four stages: asymptomatic hyperuricemia, acute gouty flares, intercritical gout, and chronic tophaceous gout.