Podcast
Questions and Answers
What is a significant challenge associated with sulcus removal surgery compared to surgery for vocal nodules?
What is a significant challenge associated with sulcus removal surgery compared to surgery for vocal nodules?
- It can be performed under local anesthesia.
- It requires less surgical disturbance of the vocal fold mucosa.
- It requires considerable surgical disturbance of the vocal fold mucosa. (correct)
- It involves additional steps for postoperative care.
Which step is essential in the surgical process of glottic sulcus removal described by Bouchayer and colleagues?
Which step is essential in the surgical process of glottic sulcus removal described by Bouchayer and colleagues?
- Circumcision of the sulcus lips. (correct)
- Direct removal of the vocal ligament.
- Application of postoperative antibiotics.
- Placement of a tracheostomy tube.
How does the thickness of the mucosa affect the surgical outcomes for glottic sulcus removal?
How does the thickness of the mucosa affect the surgical outcomes for glottic sulcus removal?
- Thinner mucosa guarantees a better surgical outcome.
- Thicker mucosa may yield a normal voice post-surgery. (correct)
- Thicker mucosa prevents any surgical intervention.
- Thin mucosa always results in a normal voice.
What is a possible postoperative outcome for patients with very thin mucosa after surgery?
What is a possible postoperative outcome for patients with very thin mucosa after surgery?
What does the surgical process for sulcus removal involve in terms of mucosal manipulation?
What does the surgical process for sulcus removal involve in terms of mucosal manipulation?
What is a primary cause of the chief problem associated with a glottic sulcus?
What is a primary cause of the chief problem associated with a glottic sulcus?
Which symptom is most commonly reported by patients with a glottic sulcus?
Which symptom is most commonly reported by patients with a glottic sulcus?
What diagnostic tool is often required for a definitive diagnosis of a glottic sulcus?
What diagnostic tool is often required for a definitive diagnosis of a glottic sulcus?
What does the presence of a mucosal bridge indicate in relation to glottic sulcus?
What does the presence of a mucosal bridge indicate in relation to glottic sulcus?
What kind of management is typically NOT expected to resolve a glottic sulcus?
What kind of management is typically NOT expected to resolve a glottic sulcus?
What vocal phenomenon might be noted in patients with glottic sulcus during assessment?
What vocal phenomenon might be noted in patients with glottic sulcus during assessment?
What does the term 'sulcus' refer to in relation to the anatomy of the vocal cords?
What does the term 'sulcus' refer to in relation to the anatomy of the vocal cords?
Which group of individuals is glottic sulcus primarily associated with?
Which group of individuals is glottic sulcus primarily associated with?
Flashcards are hidden until you start studying
Study Notes
Glottic Sulcus
- Epidemiology: Glottic sulcus primarily occurs in vocal overdoers; some believe it can be congenital, but this is not confirmed.
- Pathophysiology and Pathology:
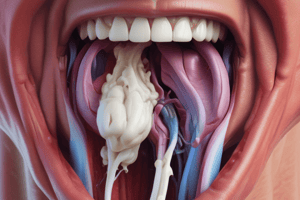
- Glottic sulcus is an epithelium-lined pocket parallel to the vocal fold edge.
- May result from a spontaneously emptied epidermal cyst, leaving a collapsed pocket.
- A mucosal bridge occurs when two parallel sulci originate from a single cyst.
- Diagnosis:
- History: Patients often report voice overuse and chronic hoarseness.
- Vocal Capability Battery: Displays noticeable hoarseness, upper voice limitations, particularly diplophonia, with an abrupt transition between hoarse phonation and aphonia.
- Laryngeal Examination: May initially reveal fewer findings than expected for the voice impairment.
- Stroboscopy: Shows a segment of reduced vibration, with the entire length of the mucosa oscillating at lower frequencies and the midportion stopping at higher frequencies, leading to short-segment vibration of anterior and posterior segments.
- Management:
- Medical: Supportive, but ineffective in resolving the structural abnormality.
- Behavioral: Short preoperative voice therapy is indicated for vocal overdoers, with the initial goal of selecting and preparing for surgery.
- Surgical:
- Removal is technically demanding, requiring significant vocal fold mucosa disturbance.
- Steps include cordal injection, circumcision of sulcus lips, and dissection of the mucosal pocket without injuring the vocal ligament.
- Outcomes depend on mucosal thickness, with thicker, almost polypoid mucosa potentially yielding a normal voice.
- Residual mucosal stiffness may persist even after optimal surgery in patients with thin and adherent mucosa.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.