Podcast
Questions and Answers
What is the primary mechanism of action for opioid-based antidiarrheals?
What is the primary mechanism of action for opioid-based antidiarrheals?
Which of the following is a component of a homemade rehydration solution in 'no-mans-land'?
Which of the following is a component of a homemade rehydration solution in 'no-mans-land'?
What symptom is associated with fecal impaction?
What symptom is associated with fecal impaction?
What is a common dietary cause of constipation?
What is a common dietary cause of constipation?
Signup and view all the answers
Which type of laxative works by pulling water into the stool and adding bulk?
Which type of laxative works by pulling water into the stool and adding bulk?
Signup and view all the answers
What is a potential consequence of overdosing on ginger as a medication?
What is a potential consequence of overdosing on ginger as a medication?
Signup and view all the answers
Which medication is primarily used as a transdermal patch for reducing vestibular excitation?
Which medication is primarily used as a transdermal patch for reducing vestibular excitation?
Signup and view all the answers
Which drug class includes medications that stimulate GI motility through D2 receptor antagonism?
Which drug class includes medications that stimulate GI motility through D2 receptor antagonism?
Signup and view all the answers
What is the main active ingredient in Dronabinol (Marinol)?
What is the main active ingredient in Dronabinol (Marinol)?
Signup and view all the answers
Which of the following side effects is associated with medications that belong to the Phenothiazine class?
Which of the following side effects is associated with medications that belong to the Phenothiazine class?
Signup and view all the answers
What is the primary function of the small intestine?
What is the primary function of the small intestine?
Signup and view all the answers
Which part of the large intestine is NOT correctly matched with its function?
Which part of the large intestine is NOT correctly matched with its function?
Signup and view all the answers
Which term describes a loss of appetite?
Which term describes a loss of appetite?
Signup and view all the answers
What role does the 'host flora' play in the gastrointestinal system?
What role does the 'host flora' play in the gastrointestinal system?
Signup and view all the answers
Which disorder is characterized by an inability to properly innervate the intestinal muscles?
Which disorder is characterized by an inability to properly innervate the intestinal muscles?
Signup and view all the answers
What is the length of the small intestine?
What is the length of the small intestine?
Signup and view all the answers
Which blood test specifically checks for antibodies related to gastrointestinal issues?
Which blood test specifically checks for antibodies related to gastrointestinal issues?
Signup and view all the answers
Which part of the large intestine is primarily involved in the initial absorption of water?
Which part of the large intestine is primarily involved in the initial absorption of water?
Signup and view all the answers
What is the primary immune response triggered by gluten in celiac disease?
What is the primary immune response triggered by gluten in celiac disease?
Signup and view all the answers
Which of the following is NOT a common symptom of celiac disease?
Which of the following is NOT a common symptom of celiac disease?
Signup and view all the answers
What is the preferred treatment approach for managing celiac disease?
What is the preferred treatment approach for managing celiac disease?
Signup and view all the answers
What is a severe complication that can arise from an E-coli infection?
What is a severe complication that can arise from an E-coli infection?
Signup and view all the answers
What is the typical treatment option for an E-coli infection?
What is the typical treatment option for an E-coli infection?
Signup and view all the answers
Which of the following statements about diarrhea is accurate?
Which of the following statements about diarrhea is accurate?
Signup and view all the answers
What is a potential complication of untreated diarrhea?
What is a potential complication of untreated diarrhea?
Signup and view all the answers
Which of the following is a risk factor for E-coli infection?
Which of the following is a risk factor for E-coli infection?
Signup and view all the answers
What is a primary treatment for abdominal discomfort caused by dietary ingestion?
What is a primary treatment for abdominal discomfort caused by dietary ingestion?
Signup and view all the answers
Which enzyme is specifically used to enhance the digestion of carbohydrates into simple sugars?
Which enzyme is specifically used to enhance the digestion of carbohydrates into simple sugars?
Signup and view all the answers
What is a characteristic of gastroparesis?
What is a characteristic of gastroparesis?
Signup and view all the answers
Which of the following mechanisms can trigger vomiting?
Which of the following mechanisms can trigger vomiting?
Signup and view all the answers
What is the potential side effect of medications that target nausea and vomiting?
What is the potential side effect of medications that target nausea and vomiting?
Signup and view all the answers
Which type of receptors are antagonized to treat motion-induced nausea?
Which type of receptors are antagonized to treat motion-induced nausea?
Signup and view all the answers
What should be addressed when treating the effects of profuse vomiting?
What should be addressed when treating the effects of profuse vomiting?
Signup and view all the answers
Which drug is a combination of diphenhydramine and chlorotheophylline, used for nausea?
Which drug is a combination of diphenhydramine and chlorotheophylline, used for nausea?
Signup and view all the answers
Study Notes
GI Terminology
- Host flora: Intestinal bacteria, up to 500 species.
- Colonization: The development of host flora in the intestines.
- Anorexia: Loss of appetite.
- Retching: Rhythmic movements of abdominal muscles, diaphragm, and chest wall.
- Emesis: Vomiting, expulsion of GI contents.
- Congenital: Present at birth.
- Dysphagia: Difficulty swallowing.
- Serology: Blood test, specifically antibody testing.
- Biopsy: Tissue sample for patho-analysis.
- Colonoscopy: Viewing of the lower GI tract.
- Endoscopy: Viewing of the upper GI tract.
Upper GI: Congenital Malformations
- TEF (TE fistula): Tracheoesophageal fistula, a connection between the trachea and esophagus.
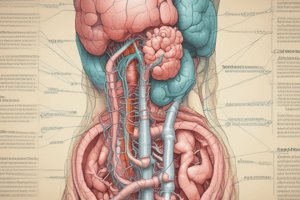
Small Intestine
- Length: 20 feet (6 meters)
- Diameter: 1 inch
- Parts: Duodenum, jejunum, ileum (longest).
- Major Function: Absorption of nutrients.
- Associated Organs: Pancreas, liver, gallbladder.
Large Intestine
- Length: 5 feet (1.5 meters)
- Diameter: 3 inches (7 cm)
- Parts: Ascending colon, transverse colon, descending colon, sigmoid colon.
- Major Functions: Reabsorption of water, vitamin B & K synthesis by host flora.
GI Innervation Review
-
Intestinal Motility: Affected by the nervous system:
- ANS: Sympathetic and parasympathetic nervous systems.
-
Enteric Nervous System: Receives input from:
- Mechanoreceptors: Detect GI stretch.
- Chemoreceptors: Detect food presence, osmolality, and pH.
Innervation Issues
- Hirschsprung Disease: A congenital condition where nerve cells are missing in the large intestine, impacting motility.
Inflammatory Disorders
- Common Signs and Symptoms: Anorexia, diarrhea, nausea.
-
Celiac Disease:
- Gluten-sensitive enteropathy: Gluten triggers an immune response to alpha-gliadin, leading to inflammation and loss of villi in the small intestine.
- Signs and Symptoms: Anorexia, bloating, diarrhea, malnutrition.
- Complications: Malnutrition, weight loss, anemia.
- Diagnosis: Serology and biopsy.
- Treatment: Gluten-free diet.
Infectious Diseases
-
C-Dif:
- Gram-positive bacteria.
- Treatment options include antibiotics.
-
E-Coli:
- Gram-negative bacteria.
- Causes: Ingestion of E-coli, often from undercooked meat, contaminated vegetables, water, and unwashed hands.
- Signs and Symptoms: Diarrhea, pain, fever.
- Complications: Hemolytic uremic syndrome, a life-threatening condition caused by Shiga-toxin damaging endothelial cells, platelets, and red blood cells.
- Treatment: Supportive care.
Diarrhea
- Symptom: Increased frequency and fluidity of loose or unformed stool.
- Causes: Inflammation or infectious organisms.
- Types: Acute (less than 4 weeks) and chronic (more than 4 weeks).
- Complications: Electrolyte imbalance, dehydration, malabsorption.
- Treatment: Rehydration, antidiarrheal medications.
Rehydration
- Hospital: Isotonic IV solutions (e.g., Normal Saline) and serum electrolyte monitoring.
- Home: Oral rehydration solutions (e.g., Gastrolyte, Pedialyte).
Antidiarrheal Medications
-
Opioid-Based:
- Mechanism of action: Mu2 receptor agonism in the GI's Enteric Nervous System, decreasing peristalsis.
- Examples: Lomotil (diphenoxylate atropine), Imodium (Loperamide HCl).
- Side Effects: Central nervous system depression, addiction.
- Atropine: Antimuscarinic agent that blocks the parasympathetic system and stimulates the sympathetic nervous system.
Constipation
- Symptom: Infrequent, incomplete, or difficult passage of stool.
- Causes: Inadequate fluid or fiber intake, alterations in peristalsis or intestinal innervation, inactivity or bedrest, surgery, drugs, pain, and altered bowel routine.
- Treatment: Laxatives (bulk forming, softeners, stimulant, osmotic, lubricant).
Bloating
- Symptom: Gas.
- Treatment: Gas X (simethicone) and Beano (alpha-d-galactosidase).
Gastroparesis
- Slowed or stopped movement of food from the stomach to the small intestine without a blockage in the stomach or intestines.
Nausea and Vomiting
- Defense System: A protective mechanism triggered by different stimuli.
- Physiology: Vomiting center in the medulla receives stimuli from the chemoreceptor trigger zone (CTZ), organs, and other regions.
- CTZ: Situated outside the blood-brain barrier, it is exposed to blood and cerebrospinal fluid contents.
-
Stimuli:
- Motion induced (motion sickness).
- Anticipatory nausea.
- Food poisoning.
- Pain.
- Medications.
Treatment of Nausea & Vomiting
-
Target specific receptors:
- Antihistamines (H1 antagonists).
- Antimuscarinic anticholinergics.
- Serotonin antagonists (5HT3 antagonists).
- Dopamine antagonists.
- Cannabinoids (CB1 and CB2 agonists).
- Treatment of the underlying cause: Treat pain, food poisoning, etc.
- Treatment of the effects of profuse vomiting: Rehydration and electrolyte correction.
Antihistamine Medications
- Mechanism of Action: Antagonize receptors of vestibular excitation.
- Examples: Dimenhydrinate (Gravol), meclizine (Dramamine), Diclectin (doxylamine + pyridoxine hydrochloride).
Ginger
- Medication: Ginger gravol (herbal therapy).
- Mechanism of Action: Increases intestinal emptying.
- Safety: Safe in moderate doses.
Antimuscarinic Anticholinergic Medications
- Mechanism of action: Reduce vestibular excitation.
- Example: Scopolamine (Hyoscine) - available in transdermal patches, IV, and oral forms.
Serotonin Antagonist Medications
- Mechanism of action: 5HT3 receptor antagonism.
- Example: Ondansetron (Zofran) - available in oral and IV forms.
Dopamine Antagonist Medications
- Mechanism of action: D2 receptor antagonism.
- Examples: Metoclopramide (Maxeran, Reglan), prochlorperazine (Stemetil) - available in oral, IV, and subcutaneous forms.
- Side Effects: Sedation.
Cannabinoid Medications
- Mechanism of action: CB1 and CB2 receptor agonism.
- Examples: Dronabinol (Marinol), Cesamet /Nabilone, cannabis.
- Agonism Effects: Affects other neurotransmitters like serotonin, GABA, and dopamine.
Summary of Treatment
- Rehydration: Essential for managing dehydration and electrolyte imbalances.
- Antidiarrheal medications: Opioid-based medications and atropine.
- Nausea and vomiting medications: Target specific receptors with antihistamines, antimuscarinic anticholinergics, serotonin antagonists, dopamine antagonists, and cannabinoids.
- Laxatives: Bulk-forming, softeners, stimulants, osmotics, and lubricants.
- Anti-bloating medications: Gas X (simethicone) and Beano (alpha-d-galactosidase).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on gastrointestinal (GI) terminology and anatomy. This quiz covers key concepts such as host flora, congenital malformations, and the structure and function of the small and large intestines. Perfect for anyone studying GI health or related fields.