Podcast
Questions and Answers
What is the primary function of the alimentary canal?
What is the primary function of the alimentary canal?
- Transport of nutrient molecules into blood
- Passage of food and waste (correct)
- Secretion of digestive enzymes
- Production of bile acids
Which of the following is NOT classified as an accessory organ of the GIT?
Which of the following is NOT classified as an accessory organ of the GIT?
- Gallbladder
- Large intestine (correct)
- Pancreas
- Liver
What role do bile acids play in digestion?
What role do bile acids play in digestion?
- Solubilize lipids for digestion (correct)
- Provide optimal pH for enzymes
- Initiate protein hydrolysis
- Transport nutrients across cell membranes
Which part of the GIT is primarily responsible for the final digestion of nutrients?
Which part of the GIT is primarily responsible for the final digestion of nutrients?
What is the main function of exocrine cells in the GIT?
What is the main function of exocrine cells in the GIT?
What components help maintain teeth by compensating for demineralization?
What components help maintain teeth by compensating for demineralization?
Which system primarily controls salivary secretion?
Which system primarily controls salivary secretion?
What is the effect of atropine on salivary secretion?
What is the effect of atropine on salivary secretion?
What term describes the absence of saliva?
What term describes the absence of saliva?
Which chemical is released by acinar cells during parasympathetic stimulation?
Which chemical is released by acinar cells during parasympathetic stimulation?
Which reflex is a primary trigger for salivary secretion?
Which reflex is a primary trigger for salivary secretion?
What is the main type of receptors involved in sympathetic stimulation of salivary glands?
What is the main type of receptors involved in sympathetic stimulation of salivary glands?
What causes xerostomia?
What causes xerostomia?
What are the large peptides produced by endopeptidases that stimulate gastrin and CCK release?
What are the large peptides produced by endopeptidases that stimulate gastrin and CCK release?
What is the term used to describe the increase of HCO3- in the bloodstream during active acid secretion from the stomach?
What is the term used to describe the increase of HCO3- in the bloodstream during active acid secretion from the stomach?
What factor does NOT influence the secretion of H+ in the stomach?
What factor does NOT influence the secretion of H+ in the stomach?
Which mechanism helps protect the gastric mucosa from acidic gastric contents?
Which mechanism helps protect the gastric mucosa from acidic gastric contents?
What happens to the gastric luminal pH after a meal due to the buffering capacity of proteins?
What happens to the gastric luminal pH after a meal due to the buffering capacity of proteins?
What substance is secreted by D cells in the antrum to inhibit gastrin release?
What substance is secreted by D cells in the antrum to inhibit gastrin release?
What is the thickness of the mucus gel layer that protects the gastric epithelium?
What is the thickness of the mucus gel layer that protects the gastric epithelium?
During which condition does gastric acid secretion primarily increase?
During which condition does gastric acid secretion primarily increase?
What is the primary role of mucin in saliva?
What is the primary role of mucin in saliva?
Which enzyme is predominantly produced by the parotid glands to aid in digestion?
Which enzyme is predominantly produced by the parotid glands to aid in digestion?
How much saliva does a healthy person produce on average each day?
How much saliva does a healthy person produce on average each day?
Which of the following components of saliva plays a role in antibacterial activity?
Which of the following components of saliva plays a role in antibacterial activity?
What is the optimal pH for lingual lipase activity?
What is the optimal pH for lingual lipase activity?
What type of acid-base reaction does saliva facilitate?
What type of acid-base reaction does saliva facilitate?
What percentage of saliva is composed of water?
What percentage of saliva is composed of water?
What is the surface area of the human intestine approximately equal to?
What is the surface area of the human intestine approximately equal to?
What stimulates the release of secretin that inhibits gastrin release?
What stimulates the release of secretin that inhibits gastrin release?
Which hormone is primarily responsible for inhibiting parietal cell acid secretion?
Which hormone is primarily responsible for inhibiting parietal cell acid secretion?
What percentage of the pancreas is constituted by the endocrine component?
What percentage of the pancreas is constituted by the endocrine component?
What is the primary function of the pancreas as an exocrine gland?
What is the primary function of the pancreas as an exocrine gland?
What hormone is secreted by the alpha cells of the Islets of Langerhans?
What hormone is secreted by the alpha cells of the Islets of Langerhans?
Which function is NOT attributed to insulin?
Which function is NOT attributed to insulin?
Which digestive enzymes are primarily secreted by the acini of the pancreas?
Which digestive enzymes are primarily secreted by the acini of the pancreas?
What is the role of somatostatin in the pancreas?
What is the role of somatostatin in the pancreas?
Flashcards are hidden until you start studying
Study Notes
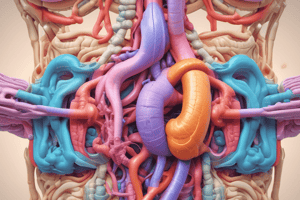
Subdivisions of the GIT System
- Alimentary Canal: The primary pathway for food and waste, which includes the mouth, pharynx, esophagus, stomach, small intestine, and large intestine.
- Accessory Organs: These are connected to the alimentary canal but do not have food or waste passing through them; they include teeth, tongue, salivary glands, liver, gallbladder, and pancreas.
Gastrointestinal Tract Function
- Initial mechanical breakdown and mixing of food with digestive fluids occurs through mechanical homogenization.
- Digestive enzymes (more than 30g protein daily) hydrolyze macromolecules into smaller molecules like oligomers and monomers.
- Electrolytes are secreted to maintain a conducive environment for enzymatic activity.
- Bile acids act as detergents, aiding in lipid digestion and absorption.
- Final digestion of nutrients occurs in the intestine via enzymes on the intestinal surface.
- Nutrient molecules are transported from the intestinal lumen into the bloodstream.
Specialized Glands and Epithelia
- The GIT has specialized glands such as salivary glands, gastric mucosa, pancreas, liver, and intestinal linings for digestion and absorption.
- Salivary glands and the pancreas have specialized cells that produce and deliver enzymes (exocrine function).
- The stomach initiates protein hydrolysis and assists in digestion through its mechanical actions.
- The pancreas and small intestine are critical for nutrient assimilation, with substantial reserve capacities for enzyme secretion.
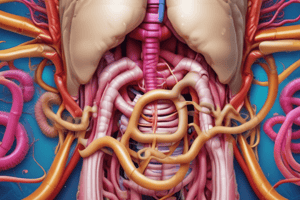
Intestinal Surface Area
- The total surface area of the human intestine is around 180 m², comparable to a tennis court (195.7 m²).
Fluid Balance in the GI Tract
- Daily ingestion is approximately 2 liters.
- Absorption in the GI tract totals around 8.8 liters, while secretion amounts to about 7 liters.
- Fecal output is around 0.2 liters daily.
Saliva Composition and Production
- Saliva originates from three major glands: parotid, sublingual, and submandibular.
- A healthy individual produces about 1 liter of saliva daily, with a pH of 6.0-7.0.
- Contains primarily water (99%), ions (e.g., HCO3-, K+, Cl-), and 1% solid proteins, primarily mucin.
- Digestive enzymes in saliva include salivary amylase and lingual lipase.
Functions of Saliva
- Lubricates food and initiates digestion of polysaccharides and lipids.
- Mild antibacterial properties through components like muramidase, lactoferrin, and immunoglobulin IgA.
- Neutralizes food acids and regurgitated stomach acid.
- Maintains teeth health by replenishing minerals lost during bacterial fermentation.
Control of Salivary Secretion
- Primarily controlled by the autonomic nervous system, rather than GIT hormones.
- Parasympathetic stimulation from the salivatory nuclei enhances secretion through taste and mechanical input.
- Sympathetic stimulation increases salivary secretion slightly via beta-adrenergic receptors.
- Xerostomia (dry mouth) can result from drug side effects or systemic diseases, leading to discomfort and infections.
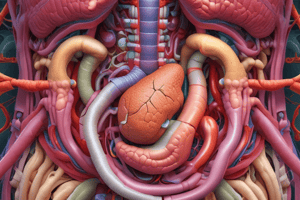
Stomach Anatomy
- The stomach is divided into three regions: cardia, fundus and body, and antrum.
- Surface mucous cells produce neutral mucins and HCO3- for protective mucous gel formation.
- Endopeptidase in the stomach works on peptide bonds, producing peptones, which stimulate gastrin release.
Gastric Acid and Protection
- HCl production involves an alkaline tide, balancing excess HCO3- entering the bloodstream.
- Regulation of HCl secretion is influenced by gastrin, histamine, and acetylcholine; absence of any factor affects acid secretion.
- Gastric mucosal barrier protects against acidic contents through mucus and alkaline secretions, maintaining a near-neutral pH for epithelial cells.
Pancreas Functions
- The pancreas serves both exocrine (digestive enzymes) and endocrine (hormone production) functions.
- The acini produce pancreatic juice, while the islets of Langerhans secrete insulin and glucagon.
- Exocrine function accounts for 99% of pancreas activity; hormones support metabolic regulation of glucose, lipids, and proteins.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.