Podcast
Questions and Answers
What characterizes the muscularis propria of the large intestine?
What characterizes the muscularis propria of the large intestine?
- Contains three separate longitudinal bands in the rectum (correct)
- Has inner circular and outer longitudinal muscle layers (correct)
- Consists of only longitudinal muscle layers
- Only contains outer circular muscles
Which type of cells is NOT found in the mucosa of the large intestine?
Which type of cells is NOT found in the mucosa of the large intestine?
- Ciliated epithelium cells (correct)
- Mucous secreting goblet cells
- Absorptive cells
- Goblet cells
Where does an abrupt transition in epithelial type occur in the large intestine?
Where does an abrupt transition in epithelial type occur in the large intestine?
- At the anus
- At the anorectal junction (correct)
- At the rectum
- At the caecum
What is a prominent feature of the mucosa in the large intestine?
What is a prominent feature of the mucosa in the large intestine?
What is true about the rectal mucosa compared to the rest of the large bowel?
What is true about the rectal mucosa compared to the rest of the large bowel?
Which structure opens into small pits at the distal ends of the columns of Morgagni?
Which structure opens into small pits at the distal ends of the columns of Morgagni?
What type of epithelial change occurs at the anal sphincter?
What type of epithelial change occurs at the anal sphincter?
What distinguishes the mucosal glands of the large intestine?
What distinguishes the mucosal glands of the large intestine?
What unique feature distinguishes the duodenum from other parts of the small intestine?
What unique feature distinguishes the duodenum from other parts of the small intestine?
Which cell type in the small intestine is primarily responsible for lubrication?
Which cell type in the small intestine is primarily responsible for lubrication?
What is the role of enterocytes found in the intestinal villi?
What is the role of enterocytes found in the intestinal villi?
What type of tissue is found in abundance within the mucosa of the appendix?
What type of tissue is found in abundance within the mucosa of the appendix?
Which characteristic is true about the crypts of Lieberkuhn?
Which characteristic is true about the crypts of Lieberkuhn?
How does the height of villi change along the small intestine?
How does the height of villi change along the small intestine?
What is the main function of the muscularis propria at the ileocecal junction?
What is the main function of the muscularis propria at the ileocecal junction?
Which of the following descriptions best fits Paneth cells?
Which of the following descriptions best fits Paneth cells?
Which cellular component is most abundant in the enterocytes of the small intestine?
Which cellular component is most abundant in the enterocytes of the small intestine?
What type of epithelial tissue lines the intestinal villi?
What type of epithelial tissue lines the intestinal villi?
What type of cells are primarily found lining the glands in the pylorus of the stomach?
What type of cells are primarily found lining the glands in the pylorus of the stomach?
Which of the following features is characteristic of the pyloric sphincter?
Which of the following features is characteristic of the pyloric sphincter?
What is the primary function of G cells in the pyloric region?
What is the primary function of G cells in the pyloric region?
How is the mucosa of the small intestine structured?
How is the mucosa of the small intestine structured?
What cellular structure enhances the absorption surface area of enterocytes?
What cellular structure enhances the absorption surface area of enterocytes?
Brunner's glands are located in which part of the digestive system?
Brunner's glands are located in which part of the digestive system?
What distinguishes the villous absorptive mucosa of the duodenum from that of the stomach?
What distinguishes the villous absorptive mucosa of the duodenum from that of the stomach?
Which structure is involved with the segmentation and mixing of contents in the small intestine?
Which structure is involved with the segmentation and mixing of contents in the small intestine?
Which is NOT a function of the pylorus of the stomach?
Which is NOT a function of the pylorus of the stomach?
What purpose do the many circular folds, or plicae circulares, serve in the jejunum?
What purpose do the many circular folds, or plicae circulares, serve in the jejunum?
What type of epithelium lines the lumen of the oesophagus?
What type of epithelium lines the lumen of the oesophagus?
Which component is NOT present in the muscularis propria of the oesophagus?
Which component is NOT present in the muscularis propria of the oesophagus?
What is the primary function of the gastric glands in the stomach?
What is the primary function of the gastric glands in the stomach?
Which part of the stomach is primarily involved in the secretion of mucus?
Which part of the stomach is primarily involved in the secretion of mucus?
How does the microanatomy of the oesophagus aid in its function?
How does the microanatomy of the oesophagus aid in its function?
What characterizes the lower portion of the muscularis externa in the oesophagus?
What characterizes the lower portion of the muscularis externa in the oesophagus?
Which junction is characterized by a transition from stratified squamous to simple columnar epithelium?
Which junction is characterized by a transition from stratified squamous to simple columnar epithelium?
What type of muscles are found in the middle portion of the muscularis externa of the oesophagus?
What type of muscles are found in the middle portion of the muscularis externa of the oesophagus?
What is the primary role of parietal cells in the gastric glands?
What is the primary role of parietal cells in the gastric glands?
What type of epithelium is found in the gastric mucosa?
What type of epithelium is found in the gastric mucosa?
What does the muscularis propria of the stomach include?
What does the muscularis propria of the stomach include?
Which cell type in the gastric glands secretes pepsin?
Which cell type in the gastric glands secretes pepsin?
Which region of the stomach is primarily responsible for the storage of food?
Which region of the stomach is primarily responsible for the storage of food?
How are the gastric pits characterized?
How are the gastric pits characterized?
Flashcards are hidden until you start studying
Study Notes
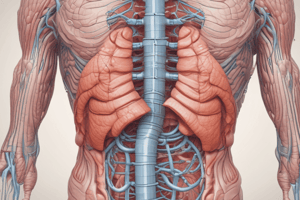
Introduction
- The gastrointestinal tract (GIT) breaks down and absorbs food.
- The GIT is specialized to serve different functions from mouth to anus.
- Four abrupt transitions in the mucosa occur along the GIT:
- Oesophago-gastric junction: distal oesophagus meets proximal stomach
- Gastroduodenal junction: pyloric stomach joins duodenum of the small intestine
- Ileocecal junction: ileum of small intestine joins cecum of large intestine
- Rectoanal junction: between the rectum and anal canal
Oesophagus
- Muscular tube that carries food from the pharynx to the stomach.
- When relaxed, oesophageal mucosa is deeply folded, allowing distension.
- Lumen is lined by stratified squamous epithelium, with a narrow lamina propria containing lymphoid tissue.
- Submucosa is loose with elastin fibres and contains seromucous glands.
- Muscularis propria consists of outer longitudinal and inner circular muscle layers.
- Oesophagus is subdivided into three sections:
- Upper portion: Entirely skeletal muscle, crucial for voluntary swallowing.
- Middle portion: Combination of skeletal and smooth muscle.
- Lower portion: Entirely smooth muscle.
Oesophago-gastric Junction
- At the junction, the mucosa transitions from stratified squamous to simple columnar epithelium.
- Muscularis mucosae continues but is not easily discernible in the stomach.
- Submucosa and muscularis propria remain uninterrupted.
- No defined anatomical sphincter, rather a physiological sphincter mechanism.
Stomach
- Portion of the GIT partially digesting food to form chyme.
- Anatomically divided into four parts: cardia, fundus, body, and pylorus.
- Histologically divided into three parts:
- Cardia: Small area of mucous-secreting glands surrounding the oesophagus entrance.
- Body/Fundus: Major histological region (histologically identical).
- Pylorus: Most distal part of the stomach.
Body of Stomach
- Mucosa forms regular folds (rugae) with gastric glands extending from the muscularis mucosae to the stomach lumen.
- Inner circular layer of the muscularis propria has an additional inner oblique layer.
- Submucosa is loose and contains larger blood vessels.
- Serosal layer is thin.
Gastric Gland
- Secretes gastric juice containing hydrochloric acid and pepsin.
- Divided into three parts: isthmus, neck, and base.
Gastric Gland Cell Types
- Parietal cells: secrete gastric acid and intrinsic factor (essential for vitamin B12 uptake).
- Neck mucous cells: secrete acidic mucin.
- Stem cells: give rise to all other gastric gland cells.
- Chief (Peptic) cells: secrete pepsin, characterized by basophilic granular cytoplasm.
- Neuroendocrine cells: secrete serotonin.
Pylorus of Stomach
- Glands are branched and coiled, with gastric pits occupying half the mucosal thickness.
- Glands are lined by mucous-secreting cells and a few parietal cells.
- Prominent muscularis mucosae separates glands from the submucosa.
- G cells secrete gastrin, a hormone that promotes pepsin and acid secretion, enhancing gastric motility.
Gastroduodenal Junction
- Marks a transition from the glandular mucosa of the stomach to the villous mucosa of the duodenum.
- Brunners glands (secreting alkaline mucous) are found in the submucosa of the duodenum, sometimes extending into the mucosa.
- Pyloric sphincter has a thickening of the circular layer of the muscularis propria.
- Circular and longitudinal layers of muscularis propria are continuous between pylorus and duodenum.
Small Intestine
- Mucosa and submucosa form circular folds (plicae circulares), particularly numerous in the jejunum.
- Mucosal surface is covered in villi with microvilli on the luminal surface of enterocytes.
- Muscularis mucosae lies under crypts and separates the mucosa from the submucosa.
- Vascular submucosa forms the core of plicae circulares.
- Peritoneal aspect of the muscular propria is covered by loose collagenous serosa.
Duodenum
- Exhibits typical small intestine features with elongated villi and crypts of Lieberkuhn.
- Villus height decreases towards the end of the small intestine.
- Characterized by extensive coiled, branched, tubular Brunners glands in the submucosa.
- Brunners glands sometimes extend into the lamina propria and empty into the crypts.
Duodenal Epithelium
- Contains goblet cells with mucigen granules, Golgi apparatus, and rough endoplasmic reticulum (rER).
- Enterocytes have less prominent rER but high numbers of free ribosomes and mitochondria.
Intestinal Villi
- Lined by simple columnar epithelium continuous with that of the crypts.
- Lamina propria extends into the villus core and contains a rich vascular and lymphatic network for nutrient absorption.
- Muscularis mucosae lies beneath the crypts.
Intestinal Villi Epithelium
- Contains diverse cell types:
- Enterocytes: columnar cells with microvilli, serving an absorptive role.
- Goblet cells: secrete mucin for lubrication.
- Paneth cells: defensive role.
- Stem cells.
- Intraepithelial lymphocytes: mostly T-cells.
- Neuroendocrine cells: regulate gastric motility and secretion.
Ileocecal Junction
- Abrupt transition from the small intestinal villiform pattern to the large intestinal glandular form.
- Thickened extension of the muscularis propria provides strong support for the mucosa.
- Lymphoid tissue, including Peyers patches, is present in the mucosa.
Appendix
- Structurally similar to the large intestine.
- Suspensory mesoappendix is continuous with the outer serosal layer.
- Contains lymphoid tissue in the mucosa and submucosa, sometimes forming follicles that bulge into the lumen.
- Mucosal glands are less densely packed than in the large intestine.
Colon
- Muscularis propria consists of inner circular and outer longitudinal muscle, except in the rectum where the longitudinal muscle forms three bands (taeniae coli).
- Mucosa is similar throughout the colon, folded when not distended, but without distinct plicae circulares.
- Prominent muscularis mucosae is present.
- Mucosa contains two cell types:
- Absorptive cells
- Mucous-secreting goblet cells
- Cells are closely packed in straight crypts extending into the muscularis mucosae.
Anorectal Junction
- Rectal mucosa is similar to the rest of the large bowel, but with more goblet cells.
- At the junction, the epithelium transitions to stratified squamous epithelium in the anal canal.
- Branched tubular circumanal glands open into pits at the distal ends of the columns of Morgagni (longitudinal folds of the mucosa).
- At the anal sphincter, the epithelium gradually changes to skin with sebaceous and apocrine glands.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.