Podcast
Questions and Answers
What is a common symptom of gastric ulcers?
What is a common symptom of gastric ulcers?
- Nausea and vomiting
- Constipation
- Gnawing or burning pain at the upper abdomen (correct)
- Severe headache
How do proton-pump inhibitors (PPIs) function in the treatment of gastric issues?
How do proton-pump inhibitors (PPIs) function in the treatment of gastric issues?
- They directly neutralize stomach acid
- They promote the growth of healthy gut bacteria
- They block the enzyme responsible for secreting hydrochloric acid (correct)
- They increase the secretion of gastric acid
What can Helicobacter pylori infection lead to if left untreated?
What can Helicobacter pylori infection lead to if left untreated?
- Cancers of the stomach and esophagus (correct)
- Improved digestion
- Reduced stomach acid production
- Enhanced immune response
What is a potential cause of gastroesophageal reflux disease (GERD)?
What is a potential cause of gastroesophageal reflux disease (GERD)?
What role does hydrochloric acid (HCl) play in the stomach?
What role does hydrochloric acid (HCl) play in the stomach?
Which class of drugs is used to reduce gastric acidity?
Which class of drugs is used to reduce gastric acidity?
What can excessive stomach acid lead to?
What can excessive stomach acid lead to?
What is a common treatment for gastrointestinal infections caused by H. pylori?
What is a common treatment for gastrointestinal infections caused by H. pylori?
What is the primary mechanism of action for proton-pump inhibitors?
What is the primary mechanism of action for proton-pump inhibitors?
Which of the following is NOT a common side effect of proton-pump inhibitors?
Which of the following is NOT a common side effect of proton-pump inhibitors?
What is the main role of H2 receptor blockers in gastrointestinal treatment?
What is the main role of H2 receptor blockers in gastrointestinal treatment?
In the treatment of Helicobacter pylori, what constitutes the first line therapy?
In the treatment of Helicobacter pylori, what constitutes the first line therapy?
What is a potential side effect of using osmotic laxatives?
What is a potential side effect of using osmotic laxatives?
Which laxative type is recommended for slow passage of stool but not for rapid bowel evacuation?
Which laxative type is recommended for slow passage of stool but not for rapid bowel evacuation?
At what time should proton-pump inhibitors be taken for maximum effectiveness?
At what time should proton-pump inhibitors be taken for maximum effectiveness?
What is a key nursing consideration when administering antacids?
What is a key nursing consideration when administering antacids?
Which fiber type is mainly used as a bulk-forming laxative?
Which fiber type is mainly used as a bulk-forming laxative?
What condition is characterized by infrequent bowel movements and hard stool?
What condition is characterized by infrequent bowel movements and hard stool?
What is the primary mechanism by which stimulant laxatives promote bowel movement?
What is the primary mechanism by which stimulant laxatives promote bowel movement?
How long does it typically take for oral stimulant laxatives to take effect?
How long does it typically take for oral stimulant laxatives to take effect?
What is one potential risk associated with the prolonged use of stimulant laxatives?
What is one potential risk associated with the prolonged use of stimulant laxatives?
Which statement accurately describes the feedback mechanism in the endocrine system?
Which statement accurately describes the feedback mechanism in the endocrine system?
What is the role of releasing factors secreted by the hypothalamus?
What is the role of releasing factors secreted by the hypothalamus?
What is the purpose of hormone replacement therapy?
What is the purpose of hormone replacement therapy?
Which of the following is an example of a selective estrogen receptor modulator used in hormone treatment?
Which of the following is an example of a selective estrogen receptor modulator used in hormone treatment?
Which of the following is NOT a characteristic of stimulant laxatives?
Which of the following is NOT a characteristic of stimulant laxatives?
What is the primary hormone produced by the thyroid gland that helps regulate metabolism?
What is the primary hormone produced by the thyroid gland that helps regulate metabolism?
What condition is characterized by insufficient secretion of thyroid-stimulating hormone (TSH)?
What condition is characterized by insufficient secretion of thyroid-stimulating hormone (TSH)?
Which of the following treatments is capable of causing hyperthyroidism if there is over-supplementation?
Which of the following treatments is capable of causing hyperthyroidism if there is over-supplementation?
What mechanism of action do sulfonylureas use to help manage type 2 diabetes?
What mechanism of action do sulfonylureas use to help manage type 2 diabetes?
Which of the following is a common side effect of biguanides like Metformin?
Which of the following is a common side effect of biguanides like Metformin?
What is a key nursing consideration when administering insulin?
What is a key nursing consideration when administering insulin?
Which type of insulin acts the fastest, typically beginning to work within 15 minutes?
Which type of insulin acts the fastest, typically beginning to work within 15 minutes?
What type of diabetes results from the body not producing enough insulin or the body having insulin resistance?
What type of diabetes results from the body not producing enough insulin or the body having insulin resistance?
Which of the following is an adverse effect associated with carbimazole?
Which of the following is an adverse effect associated with carbimazole?
What type of medications would be suitable for type 2 diabetes that focuses on decreasing intestinal glucose absorption?
What type of medications would be suitable for type 2 diabetes that focuses on decreasing intestinal glucose absorption?
Which symptom is NOT associated with hyperthyroidism?
Which symptom is NOT associated with hyperthyroidism?
The primary role of glucagon in the body is to:
The primary role of glucagon in the body is to:
Levothyroxine, a synthetic thyroid hormone, should ideally be taken:
Levothyroxine, a synthetic thyroid hormone, should ideally be taken:
What is a potential severe complication of diabetes mellitus if poorly managed?
What is a potential severe complication of diabetes mellitus if poorly managed?
Flashcards
Peptic Ulcer
Peptic Ulcer
A sore in the lining of the stomach or the upper part of the small intestine.
GERD
GERD
Acid from the stomach flows back into the esophagus.
Proton Pump Inhibitors (PPIs)
Proton Pump Inhibitors (PPIs)
Drugs that stop the stomach from producing acid.
H. pylori
H. pylori
Signup and view all the flashcards
Gastric Acid
Gastric Acid
Signup and view all the flashcards
Stomach Acid Function
Stomach Acid Function
Signup and view all the flashcards
H2 Receptor Blockers
H2 Receptor Blockers
Signup and view all the flashcards
Antacids
Antacids
Signup and view all the flashcards
Helicobacter pylori antibiotics
Helicobacter pylori antibiotics
Signup and view all the flashcards
Triple Therapy
Triple Therapy
Signup and view all the flashcards
Bulk-forming Laxative
Bulk-forming Laxative
Signup and view all the flashcards
Osmotic Laxative
Osmotic Laxative
Signup and view all the flashcards
Stool Softener
Stool Softener
Signup and view all the flashcards
Constipation
Constipation
Signup and view all the flashcards
PPI Side Effects
PPI Side Effects
Signup and view all the flashcards
Docusate Action
Docusate Action
Signup and view all the flashcards
Stimulant Laxatives Action
Stimulant Laxatives Action
Signup and view all the flashcards
Stimulant Laxative Side Effects
Stimulant Laxative Side Effects
Signup and view all the flashcards
Feedback Mechanism
Feedback Mechanism
Signup and view all the flashcards
Endocrine System
Endocrine System
Signup and view all the flashcards
Hormone Action
Hormone Action
Signup and view all the flashcards
Hypothalamus and Pituitary Connection
Hypothalamus and Pituitary Connection
Signup and view all the flashcards
Hormone Replacement Therapy
Hormone Replacement Therapy
Signup and view all the flashcards
Thyroid Gland Function
Thyroid Gland Function
Signup and view all the flashcards
Thyroid Hormone Synthesis
Thyroid Hormone Synthesis
Signup and view all the flashcards
Hypothalamus-Pituitary-Thyroid Axis
Hypothalamus-Pituitary-Thyroid Axis
Signup and view all the flashcards
Negative Feedback Regulation
Negative Feedback Regulation
Signup and view all the flashcards
Hypothyroidism Symptoms
Hypothyroidism Symptoms
Signup and view all the flashcards
Hypothyroidism Causes
Hypothyroidism Causes
Signup and view all the flashcards
Hypothyroidism Treatment
Hypothyroidism Treatment
Signup and view all the flashcards
Levothyroxine Dosage
Levothyroxine Dosage
Signup and view all the flashcards
Levothyroxine Interactions
Levothyroxine Interactions
Signup and view all the flashcards
Hyperthyroidism Symptoms
Hyperthyroidism Symptoms
Signup and view all the flashcards
Hyperthyroidism Causes
Hyperthyroidism Causes
Signup and view all the flashcards
Hyperthyroidism Treatment
Hyperthyroidism Treatment
Signup and view all the flashcards
Carbimazole Nursing Considerations
Carbimazole Nursing Considerations
Signup and view all the flashcards
Type 1 Diabetes
Type 1 Diabetes
Signup and view all the flashcards
Type 2 Diabetes
Type 2 Diabetes
Signup and view all the flashcards
Study Notes
Drugs Affecting the Digestive and Endocrine Systems
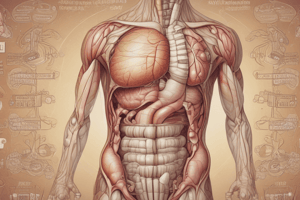
- Digestive System Overview: The digestive system breaks down food, absorbs nutrients, and eliminates waste. Organs involved include the mouth, pharynx, esophagus, stomach, liver, gallbladder, small intestine, large intestine, and rectum/anus. Different enzymes and hormones aid in these processes.
Learning Objectives
- Students should understand gastric ulcers and GERD (Gastroesophageal Reflux Disease).
- Students should describe the mechanism of action of drugs for gastric ulcers and GERD.
- Students should describe the mechanism of action of different types of laxatives.
Natural Defenses Against Stomach Acid
- Stomach lining has a bicarbonate barrier to neutralize acid.
- Mucus layer protects stomach lining from gastric juice (pH ~2).
- Gastric mucosa cells and capillaries are also involved in the protection process.
Peptic Ulcer Formation
- Normal: Damaging factors (gastric acidity, peptic enzymes), protective factors (mucus, bicarbonate secretion, etc.) balance.
- Injury: Stressors such as H. pylori infection, NSAIDs, alcohol, gastric hyperacidity or reflux upset the balance, increasing damage.
- Ulcer: Tissue damage occurs when injurious factors exceed or impair protective factors, leading to ulcers.
Functions of Stomach Acid
- Creating an acidic environment to inactivate pathogens.
- Protect against infections.
- Aid in protein digestion through activation of pepsin.
Gastric Acid Formation
- Parietal cells are responsible for stomach acid production.
- Histamine and other factors play a role in stimulating the proton pump, which transports acid into the stomach.
Gastric Ulcers
- Characterized by gnawing or burning pain in the upper abdomen.
- Progression can lead to bleeding and perforation if the erosion gets deeper.
- Helicobacter pylori (H. pylori), a bacteria, is a common cause of stomach ulcers.
Gastroesophageal Reflux Disease (GERD)
- A condition where stomach acid moves upwards into the esophagus.
- Causes intense heartburn and may lead to esophageal ulcers.
- Stomach sphincter plays a role in preventing reflux.
Drug Therapy
- Proton pump inhibitors (PPIs): Potent acid inhibitors that reduce stomach acid by irreversibly binding to the acid producing enzyme (H+, K+, ATPase).
- H2 receptor blockers: Reduce acid production by blocking H2 receptors.
- Antacids: Rapidly neutralize stomach acid using compounds of aluminum, magnesium, or calcium.
- Antibiotics: Used to eliminate H. pylori to treat infection-related ulcers and other problems.
Specific Drug Discussion (PPIs)
- Mechanism of Action: Block H+, K+, ATPase enzyme, reducing stomach acid secretion.
- Use: Treating peptic ulcer disease, GERD, H. pylori infection.
- Drugs: Omeprazole, Lansoprazole, etc.
Specific Drug Discussion (H2 Receptor Blockers)
- Mechanism of Action: Block H2 receptors to lower acid production.
- Use: Ulcers, GERD
- Drugs: Famotidine, Ranitidine
Specific Drug Discussion (Antacids)
- Mechanism of Action: Neutralize stomach acid.
- Use: Reduce symptoms of peptic ulcers ,GERD
- Drugs: Aluminum Hydroxide and Magnesium Hydroxide combinations (e.g. Triact
Specific Drug Discussion (Antibiotics)
- Mechanism of Action: Eliminate H. pylori infection, which causes ulcers.
- Use: Use in combination with other drugs to treat ulcers..
- Drugs: Amoxicillin, Clarithromycin, and Metronidazole, Tetracycline.
H.pylori Eradication Therapies
- Triple therapy: PPI, Clarithromycin, Amoxicillin (14 days).
- Quadruple therapy: PPI, Bismuth, Tetracycline, Metronidazole (14 days).
- Sequential therapy: combination regimens (variable time periods for each).
Constipation
- Characterized by infrequent bowel movements, difficult stool passage, and persists for several weeks or longer.
- When stool moves too slowly through the digestive tract.
Laxatives
- Bulk-forming: Absorb water, increasing fecal mass and stimulating bowel activity.
- Osmotic: Increase osmotic pressure in the colon, drawing water into the stool and softening it.
- Stool softeners/Surfactants: Reduce surface tension of stool to allow penetration of water inside stool for better pass.
- Stimulants: Irritate the bowel, stimulating bowel muscle contractions
Nursing Considerations for Drugs
- PPIs: Take 15-30 minutes before food, do not chew.
- H2 Receptor Blockers: Take with food.
- Antacids: Can be chewed, taken with or after food.
- All drugs: Administer separate from other medications to avoid interactions.
Lifestyle Changes for GERD
- Quit smoking
- Eat small meals often;
- Chew food slowly
- Avoid heartburn triggers (caffeine, alcohol, etc)
- Maintain good posture - sitting up straight; no lying down after meals.
- Sleep with elevation of your head and shoulders.
Endocrine System Overview
- The endocrine system is a network of glands that regulate the body's functions using hormones.
- The endocrine glands produce and secrete hormones that control various bodily processes.
Learning Objectives for Endocrine System
- Students should understand feedback mechanisms in endocrine systems.
- Students should describe the mechanism of action of drugs for diabetes mellitus.
Hormones: Role in Homeostasis
- Chemical messengers for communication in the body.
- Feedback mechanisms: Positive feedback amplifies responses, while negative feedback opposes them.
Hormones Associated with Hypothalamus and Pituitary
- Releasing and inhibiting hormones regulate the release of other hormones.
- Hypothalamus and pituitary gland regulate various bodily functions.
Hormone Replacement Therapy
- Hormones are administered to compensate for insufficient endogenous hormones.
- Use in cancer treatment therapies to shrink size of hormone-sensitive tumors.
- Example: Tamoxifen for breast cancer treatment.
Thyroid Gland
- Regulates the basal metabolic rate.
- Produces hormones (T3, T4) which control many bodily functions, including metabolism.
- The Hypothalamus and Pituitary gland regulate thyroid function through negative feedback.
Hypothyroidism
- Insufficient thyroid hormone production.
- Symptoms include: weakness, muscle cramps, weight gain, slow metabolism, cold intolerance.
- Treated with Levothyroxine (synthetic thyroid hormone).
Hyperthyroidism
- Excess thyroid hormone production.
- Symptoms include: goiter, nervousness, tremors, weight loss, heat intolerance.
- Treated with anti-thyroid drugs, surgery, or radioactive iodine.
Diabetes Mellitus
- A metabolic disorder characterized by high blood glucose levels.
- Types: Type 1 (insulin deficiency) and Type 2 (insulin resistance).
Diabetes Mellitus Signs and Symptoms
- High fasting blood sugar (2 readings)
- Polyuria (frequent urination)
- Polyphagia (increased hunger)
- Polydipsia (increased thirst)
- Glycosuria (glucose in urine)
- Weight loss
- Fatigue
Diabetic Drugs (Oral and Parenteral Hypoglycemics)
- Sulfonylureas: Increase insulin secretion from beta cells.
- Biguanides: Reduce glucose production, increase its uptake.
- Alpha-glucosidase inhibitors: Slow carbohydrate digestion.
- Dipeptidyl peptidase-4 (DPP-4) inhibitors: Increase incretin activity, potentially lowering blood glucose.
Insulin
- Naturally produced hormone for blood sugar control.
- Types: Rapid-acting, short-acting, intermediate-acting, long-acting and combinations.
- Delivery method: injections.
Nursing Considerations for Drug Therapies
- Insulin: Monitor blood glucose levels, give before meals, keep carbs available, rotate injection sites.
- Sulfonylureas: Monitor blood glucose levels, give 15 minutes before meals.
- Biguanides: Administer with meals; monitor glucose levels carefully; avoid in kidney patients.
- Alpha-glucosidase inhibitors: Administer at the start of a meal, monitor glucose levels.
General Notes
- Always check with a medical professional for specific instructions regarding drug use.
- Lifestyle modifications (diet, exercise) are crucial for managing diabetes, in addition to prescription drugs.
- Be sure to follow healthcare providers' instructions carefully.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.