Podcast
Questions and Answers
A patient presents with dysphagia following a stroke. Which cranial nerve is MOST likely affected, impacting their ability to form a food bolus?
A patient presents with dysphagia following a stroke. Which cranial nerve is MOST likely affected, impacting their ability to form a food bolus?
- CN XI - Accessory
- CN IX - Glossopharyngeal
- CN V - Trigeminal (correct)
- CN VII - Facial
A patient is diagnosed with achalasia. Which of the following BEST describes the underlying pathophysiology contributing to their dysphagia?
A patient is diagnosed with achalasia. Which of the following BEST describes the underlying pathophysiology contributing to their dysphagia?
- Development of scar tissue constricting the esophageal lumen.
- Formation of a pouch in the esophageal lining trapping food.
- External compression of the esophagus by a tumor mass.
- Loss of muscle contraction in the lower esophagus. (correct)
Which of the following is the primary difference between a sliding and rolling hiatal hernia?
Which of the following is the primary difference between a sliding and rolling hiatal hernia?
- Sliding hernias involve the sphincter sliding upwards, while rolling hernias involve the upper part of the stomach herniating through the diaphragm alongside a normally positioned sphincter. (correct)
- Rolling hernias are more common than sliding hernias.
- Only rolling hernias present with heartburn.
- Sliding hernias require surgical intervention, while rolling hernias are managed medically.
A pregnant woman reports experiencing frequent heartburn. An upper endoscopy reveals a hiatal hernia. Which type of hiatal hernia is MOST likely contributing to her symptoms?
A pregnant woman reports experiencing frequent heartburn. An upper endoscopy reveals a hiatal hernia. Which type of hiatal hernia is MOST likely contributing to her symptoms?
What is the primary cause of gastritis?
What is the primary cause of gastritis?
A patient with a peptic ulcer is being evaluated for the underlying cause. Which infectious agent is MOST commonly associated with the development of peptic ulcers?
A patient with a peptic ulcer is being evaluated for the underlying cause. Which infectious agent is MOST commonly associated with the development of peptic ulcers?
A 50-year-old male presents with pyrosis and is diagnosed with a hiatal hernia. Which of the following is the MOST likely underlying mechanism contributing to his pyrosis?
A 50-year-old male presents with pyrosis and is diagnosed with a hiatal hernia. Which of the following is the MOST likely underlying mechanism contributing to his pyrosis?
Which of the following is a potential long-term complication associated with chronic, recurring heartburn related to a hiatal hernia?
Which of the following is a potential long-term complication associated with chronic, recurring heartburn related to a hiatal hernia?
What is the primary mechanism by which Helicobacter pylori survives in the acidic environment of the stomach?
What is the primary mechanism by which Helicobacter pylori survives in the acidic environment of the stomach?
A patient presents with symptoms suggestive of a gastric disorder. Which diagnostic test would provide specific and non-invasive confirmation of H. pylori infection?
A patient presents with symptoms suggestive of a gastric disorder. Which diagnostic test would provide specific and non-invasive confirmation of H. pylori infection?
A patient is diagnosed with an H. pylori infection and prescribed triple therapy. What does this therapeutic approach typically involve?
A patient is diagnosed with an H. pylori infection and prescribed triple therapy. What does this therapeutic approach typically involve?
What is the likely cause of pyloric stenosis in adults?
What is the likely cause of pyloric stenosis in adults?
In immunocompromised patients with H. pylori infection who are difficult to treat, what additional medication is often added to the standard triple therapy, forming a quadruple therapy?
In immunocompromised patients with H. pylori infection who are difficult to treat, what additional medication is often added to the standard triple therapy, forming a quadruple therapy?
What is the most common route of transmission for H. pylori?
What is the most common route of transmission for H. pylori?
Dumping syndrome is a condition that can occur post-gastric bypass. What is the primary purpose of a gastric bypass surgery?
Dumping syndrome is a condition that can occur post-gastric bypass. What is the primary purpose of a gastric bypass surgery?
What is the mechanism of action of Pantoprazole?
What is the mechanism of action of Pantoprazole?
A patient post-gastric bypass is experiencing dumping syndrome. Which dietary modification is MOST appropriate to minimize their symptoms?
A patient post-gastric bypass is experiencing dumping syndrome. Which dietary modification is MOST appropriate to minimize their symptoms?
A patient with dumping syndrome is at risk for vitamin deficiencies due to:
A patient with dumping syndrome is at risk for vitamin deficiencies due to:
A female patient reports abdominal pain primarily relieved after a bowel movement, along with alternating constipation and diarrhea. This presentation MOST strongly suggests:
A female patient reports abdominal pain primarily relieved after a bowel movement, along with alternating constipation and diarrhea. This presentation MOST strongly suggests:
A patient diagnosed with IBS is experiencing increased symptoms during periods of high stress. Which of the following BEST explains this relationship?
A patient diagnosed with IBS is experiencing increased symptoms during periods of high stress. Which of the following BEST explains this relationship?
A patient with IBS is considering dietary changes to manage their symptoms. Which dietary addition is MOST likely to improve their condition based on its effect on serotonin levels?
A patient with IBS is considering dietary changes to manage their symptoms. Which dietary addition is MOST likely to improve their condition based on its effect on serotonin levels?
A patient presents with severe abdominal pain, distension, and vomiting. Imaging reveals a complete twisting of the intestine, compromising blood supply. Which condition is MOST likely causing these symptoms?
A patient presents with severe abdominal pain, distension, and vomiting. Imaging reveals a complete twisting of the intestine, compromising blood supply. Which condition is MOST likely causing these symptoms?
A male patient reports groin pain and a noticeable bulge in the inguinal region, especially when lifting heavy objects. This presentation is MOST consistent with:
A male patient reports groin pain and a noticeable bulge in the inguinal region, especially when lifting heavy objects. This presentation is MOST consistent with:
A patient reports discomfort and bloating in the abdomen, particularly after meals. Imaging reveals a sharp bend in the colon near the spleen, trapping intestinal contents. This is MOST indicative of:
A patient reports discomfort and bloating in the abdomen, particularly after meals. Imaging reveals a sharp bend in the colon near the spleen, trapping intestinal contents. This is MOST indicative of:
Flashcards
Dysphagia
Dysphagia
Difficulty swallowing, can arise from developmental defects or neurological damage.
Cranial Nerves V & X Role in Swallowing
Cranial Nerves V & X Role in Swallowing
Damage to these nerves may impair chewing or the unconscious movements needed for swallowing.
Diverticulum
Diverticulum
A pouch that forms in the GI tract, trapping food.
Hiatal Hernia
Hiatal Hernia
Signup and view all the flashcards
Sliding Hiatal Hernia
Sliding Hiatal Hernia
Signup and view all the flashcards
Rolling Hiatal Hernia
Rolling Hiatal Hernia
Signup and view all the flashcards
Gastritis
Gastritis
Signup and view all the flashcards
Peptic Ulcer
Peptic Ulcer
Signup and view all the flashcards
Gastric Bypass
Gastric Bypass
Signup and view all the flashcards
Accelerated Gastric Emptying
Accelerated Gastric Emptying
Signup and view all the flashcards
Dumping Syndrome
Dumping Syndrome
Signup and view all the flashcards
Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS)
Signup and view all the flashcards
IBS Predisposing Factors
IBS Predisposing Factors
Signup and view all the flashcards
Splenic Flexure Syndrome
Splenic Flexure Syndrome
Signup and view all the flashcards
Volvulus
Volvulus
Signup and view all the flashcards
Inguinal Hernia
Inguinal Hernia
Signup and view all the flashcards
Pyloric Stenosis
Pyloric Stenosis
Signup and view all the flashcards
H. pylori's Urease Role
H. pylori's Urease Role
Signup and view all the flashcards
H. pylori Associated Risks
H. pylori Associated Risks
Signup and view all the flashcards
H. pylori Diagnosis
H. pylori Diagnosis
Signup and view all the flashcards
H. pylori Triple Therapy
H. pylori Triple Therapy
Signup and view all the flashcards
H. pylori Quadruple Therapy
H. pylori Quadruple Therapy
Signup and view all the flashcards
Study Notes
- Exam covers 25% of the final grade
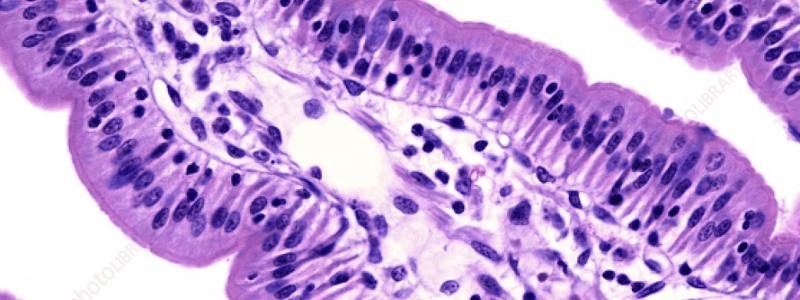
Dysphagia
- Dysphagia is difficulty swallowing
- It is caused by a developmental defect, where there is connection between the esophagus and trachea via fistula
- Dysphagia can happen anywhere along the swallowing tract
Contributions to Dysphagia
- Neurological damage to cranial nerves contributes to swallowing difficulty
- Damage to the Trigeminal nerve (CN V, chewing nerve) causes issues with chewing and bolus formation, leading to swallowing difficulties
- Damage to the Vagus nerve (CN X, swallowing nerve) affects unconscious throat movements required for smooth food passage
- Tumors can pressurize the GI tract, leading to obstruction
- Achalasia: Loss of muscle contraction in the lower esophagus leads to food getting stuck
- Diverticulum: A pouch within the inner layers of the GI tract that traps food
- Fibrosis: Scar tissue can contract and constrict the airway
Hiatal Hernia
- This is a hernia in the upper GI tract
- Sliding hernia (95%): The sphincter slides upwards, misaligning with the diaphragm, causing part of the stomach to poke through
- Treatment for sliding hernia involves surgery to suture it in place
- Rolling hernia (5%): There is loss of rigidity and increased mobility, causing the upper part of the stomach to be ABOVE the sphincter's opening
- Treatment for rolling hernia involves surgical removal of any small, necrotic pieces
- Risk factors for hiatal hernia include pregnancy
- Manifestations include pyrosis (heartburn) and the possibility of cancerous changes from recurring heartburn or herniation, due to the inability to release air
Gastric Disorders
- Gastritis: Inflammation of the stomach lining, caused by alcohol or medications, appears red and inflamed during endoscopy
- Peptic Ulcer: Can occur in the stomach or duodenum, caused by H. pylori or overuse of NSAID drugs affecting the stomach lining
- Pyloric Stenosis: Narrow opening between the stomach and duodenum due to thickened pyloric sphincter. Can cause projectile vomiting especially in babies or adults with unresolved peptic ulcers
Pathogenesis of H. Pylori
- Transmitted via stomach-to-oral route
- Urease bacterium produces urease enzyme to remain dormant in the environment
- It converts urea into NH3, creating an alkaline environment in the stomach by neutralizing stomach acid
Additional Info on Gastric Disorders
- Gastric disorders are associated with cancer of the stomach lining or lymphoma, or prolonged prescription drug use
- Diagnosed using fast, specific, and noninvasive tests, such as urea breath test or stool sample
- Medication for gastric disorders: Triple therapy with 2 antibiotics and a proton pump inhibitor. Commonly using Clarithromycin, amoxicillin and pantoprazole
- Immunocompromised patients receive quadruple therapy with bismuth
Dumping Syndrome
- This syndrome can occur after a gastric bypass, to reduce the absorption of nutrients
- Accelerated gastric emptying causes food to leave the stomach too quickly
- Extreme diarrhea
- Rapid absorption pulls water and electrolytes out of cells, causing dehydration
- Vitamin deficiencies due to bypassing the jejunum
- Management involves avoiding sugar on an empty stomach, or eating more frequent, smaller meals
Inflammatory Bowel Disease (IBS)
- IBS is a non-inflammatory condition affecting 15% of humans
- Manifestations: Abnormal contractions of the large intestinal wall, changes in bowel habits, pain or discomfort in the left quadrant of the abdomen
- Male = Diarrhea
- Female = Constipation
- Pain relief after a bowel movement rules out rectal cancer
- Stress interference with the brain-gut axis is a predisposing factor
- Gut microbiome imbalances caused by broad-spectrum antibiotic use or food allergies
- 5-HT (serotonin) imbalance: 5-HT is a promoter for bowel movement
Intestinal Obstructions
- Inguinal hernia: A twist, more common in males due to heavy lifting
- Volvulus: Any twist leading to ischemia or necrosis due to lack of perforation. Can cause sepsis
Inflammatory Bowel Disease (IBD)
- Autoimmune
- White blood cells from the gut triggered by bacterium, B cell focused
- No prevalence between male or females
Crohn's Disease
- Colposcopy reveals inflammation patches throughout the GI tract
- Fissures (deep cracks/lesions) lead to stool malabsorption.
- Complications: Fissures may cause a fistula combining the small & large intestine
Ulcerative Colitis
- Inflamed continuous lesions (innermost lining only) cause bloody stool & anemia
- Complications include toxic megacolon requiring surgical removal, which can lead to sepsis
- Rectovaginal fistula (rectum & vagina) = fecal matter coming through the vagina
- Enterovesicle fistula (between bladder & intestine resulting in fecal matter & potential blockage
Celiac Disease
- Autoimmune with sensitivity to wheat, rye, barley (gluten = protein)
- Gluten is broken down in the small intestine into gliadin, then binds to tissue transglutaminase
- Creates antibodies for celiac
Acute Appendicitis
- (inflamed appendix) reservoir of bacteria becomes inflamed if circulation is prohibited through obstruction
- Infections
- Neoplasm
- Manifestations: pain in RLQ & belly button, firm upon palpation (eventual distention
Cholelithiasis
- More common in fair-skinned females and Indigenous populations
- Birth control (estrogen & progesterone) slows downs the gallbladder, causing stone formation
- Calcium birubinate & cholesterol micro crystals & mucin can cause delayed gallbladder emptying (cholesterol buildup)
- Larger calculi has a larger impact
- Cholecystitis is infection of the biliary system
Manifestations
- Cholelithiasis
Treatment Strategies
- Describe the goal of using an NG tube with intermittent suctioning
- Describe: lithotripsy
- Describe: cholecystectomy
Cholestasis
- Gallstones in the gallbladder/cystic duct can cause obstructions
- Stones in the common bile duct prevent bile from reaching the duodenum, backing up into the liver
- Clay coloured stool because of blockage prevents proper excretion
Acute Pancreatitis
- Digestive enzymes get trapped, then can't absorb nutrients properly
- Creates pancreatic inflammation then necrosis
- Pancreas becomes irritated
- Gallstones is the is the #1 trigger for Acute Pancreatitis
- Alcohol use is #2
- Cause inflammatory response (plasma leaves vessels leading to hypovolemic shock/neurogenic shock) YOU CANNOT VASOCONSTRICT NOW
- DIC, ARDS
Chronic Pancreatitis
- Inflamed pancreas can lead to fibrosis
- Etiology includes alcohol abuse, smoking, gallstones
- Manifestations: Abdominal pain with nausea/vomiting
- Complications: Steatorrhea (fatty stool) can result in secondary diabetes mellitus due to fibrosis
Cirrhosis
- Infections from hepatitis
- Infections: Hepatitis B, C, D causes bleeding
- AIH (autoimmune hepatitis) autoimmune
- PBC (primary biliary cholangitis) autoimmune destruction of intrahepatic bile ducts
- PSC (primary sclerosis cholangitis) no antibodies involved
- NAFLD (non alcoholic fatty liver disease) resistance to blood flow through a scarred liver
- Genetic, hereditary hemochromatosis
- Wilsons disease (copper overload in the liver)
- A1AT (alpha 1 antitrypsin deficiency) liver dysfunction
- Cirrhosis causes resistance to blood flow through the liver, leading to portal hypertension causes hemorrhoids
- Bulging esophageal varices (bulging into the lumen of the esophagus) can lead to GI bleed through vomiting
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the underlying causes and mechanisms of gastrointestinal disorders, answering key questions about dysphagia, achalasia, hiatal hernias, gastritis, and peptic ulcers. Understand the role of cranial nerves, infectious agents, and long-term complications in GI health.