Podcast
Questions and Answers
Which of the following scenarios would LEAST likely contribute to the development of dysphagia?
Which of the following scenarios would LEAST likely contribute to the development of dysphagia?
- A patient with a developmental defect resulting in a fistula connecting the esophagus and trachea.
- A patient who has a fully functional trigeminal nerve (CN V). (correct)
- A patient with achalasia, characterized by the loss of muscle contraction in the lower esophagus.
- A patient experiencing scar tissue contraction of the esophagus, leading to constriction.
A patient presents with dysphagia following a stroke that damaged specific cranial nerves. If the patient has difficulty with the unconscious movements that propel food down the esophagus, which cranial nerve is MOST likely affected?
A patient presents with dysphagia following a stroke that damaged specific cranial nerves. If the patient has difficulty with the unconscious movements that propel food down the esophagus, which cranial nerve is MOST likely affected?
- Facial (CN VII)
- Trigeminal (CN V)
- Hypoglossal (CN XII)
- Vagus (CN X) (correct)
In the context of hiatal hernias, which statement BEST differentiates a sliding hernia from a rolling hernia?
In the context of hiatal hernias, which statement BEST differentiates a sliding hernia from a rolling hernia?
- Sliding hernias occur when the sphincter slides upwards, and rolling hernias occur when the upper part of the stomach protrudes above the sphincter while the sphincter remains in its normal position. (correct)
- Sliding hernias are characterized by the upper part of the stomach protruding above the sphincter, while rolling hernias involve the sphincter sliding upwards.
- Sliding hernias involve the sphincter remaining in the correct anatomical position, while rolling hernias involve the sphincter sliding upwards.
- Sliding hernias primarily result from a loss of rigidity in the stomach, whereas rolling hernias are caused by the sphincter sliding upwards.
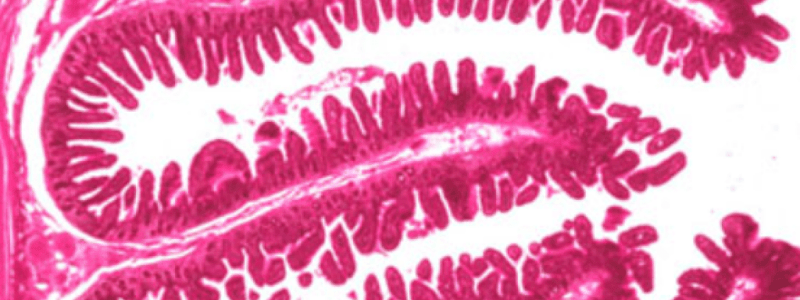
Following an endoscopy, a patient is diagnosed with gastritis. What is the MOST likely macroscopic appearance the clinician observed during the procedure?
Following an endoscopy, a patient is diagnosed with gastritis. What is the MOST likely macroscopic appearance the clinician observed during the procedure?
Which of the following pathophysiological processes would MOST directly lead to the formation of a diverticulum in the GI tract?
Which of the following pathophysiological processes would MOST directly lead to the formation of a diverticulum in the GI tract?
Which of the following factors poses the GREATEST risk for the development of cancerous changes in the context of a hiatal hernia?
Which of the following factors poses the GREATEST risk for the development of cancerous changes in the context of a hiatal hernia?
A patient is diagnosed with a peptic ulcer. What is the MOST likely etiological agent responsible for this condition?
A patient is diagnosed with a peptic ulcer. What is the MOST likely etiological agent responsible for this condition?
Which of the following is the MOST likely treatment to prevent the upward movement of the sphincter in a sliding hiatal hernia?
Which of the following is the MOST likely treatment to prevent the upward movement of the sphincter in a sliding hiatal hernia?
In the context of tissue death and sepsis, what critical process initiates the spread of bacteria beyond the gut?
In the context of tissue death and sepsis, what critical process initiates the spread of bacteria beyond the gut?
What is the primary immunological mechanism that underlies the pathology of Inflammatory Bowel Disease (IBD)?
What is the primary immunological mechanism that underlies the pathology of Inflammatory Bowel Disease (IBD)?
What diagnostic finding is most indicative of Crohn's Disease during a colposcopy?
What diagnostic finding is most indicative of Crohn's Disease during a colposcopy?
Which complication of Crohn's Disease involves the formation of a direct connection between the small and large intestine?
Which complication of Crohn's Disease involves the formation of a direct connection between the small and large intestine?
Which hormonal mechanism primarily contributes to the increased risk of cholelithiasis in women using estrogen-based birth control?
Which hormonal mechanism primarily contributes to the increased risk of cholelithiasis in women using estrogen-based birth control?
What is the primary characteristic of the lesions observed in Ulcerative Colitis that distinguishes it from other inflammatory bowel diseases?
What is the primary characteristic of the lesions observed in Ulcerative Colitis that distinguishes it from other inflammatory bowel diseases?
A patient presents with biliary sludge. Which combination of factors is most likely contributing to this condition?
A patient presents with biliary sludge. Which combination of factors is most likely contributing to this condition?
A patient is diagnosed with cholestasis secondary to cholelithiasis. Which of the following findings would be most indicative of this condition?
A patient is diagnosed with cholestasis secondary to cholelithiasis. Which of the following findings would be most indicative of this condition?
Which of the following complications of Ulcerative Colitis is characterized by severe dilation of the colon and carries a high risk of perforation and sepsis?
Which of the following complications of Ulcerative Colitis is characterized by severe dilation of the colon and carries a high risk of perforation and sepsis?
In Celiac Disease, the ingestion of gluten leads to the production of antibodies. Which protein fragment and enzyme are directly involved in triggering this autoimmune response?
In Celiac Disease, the ingestion of gluten leads to the production of antibodies. Which protein fragment and enzyme are directly involved in triggering this autoimmune response?
Following a cholecystectomy, what long-term adaptation is most crucial for patients to manage potential digestive complications?
Following a cholecystectomy, what long-term adaptation is most crucial for patients to manage potential digestive complications?
What is the most common primary mechanism leading to acute appendicitis, and how does it typically manifest?
What is the most common primary mechanism leading to acute appendicitis, and how does it typically manifest?
In the context of cholelithiasis management, what is the primary rationale for using an NG tube with intermittent suctioning?
In the context of cholelithiasis management, what is the primary rationale for using an NG tube with intermittent suctioning?
What is the underlying mechanism that allows H. pylori to survive in the harsh acidic environment of the stomach?
What is the underlying mechanism that allows H. pylori to survive in the harsh acidic environment of the stomach?
A patient with a known penicillin allergy tests positive for H. pylori. Which antibiotic regimen would be MOST appropriate as part of their triple therapy?
A patient with a known penicillin allergy tests positive for H. pylori. Which antibiotic regimen would be MOST appropriate as part of their triple therapy?
Why might a healthcare provider prescribe bismuth subsalicylate as part of a quadruple therapy for H. pylori in an immunocompromised patient?
Why might a healthcare provider prescribe bismuth subsalicylate as part of a quadruple therapy for H. pylori in an immunocompromised patient?
What is a key characteristic of pyloric stenosis that can result in projectile vomiting, especially in infants?
What is a key characteristic of pyloric stenosis that can result in projectile vomiting, especially in infants?
A patient presents with symptoms suggestive of H. pylori infection. Assuming all tests are equally accurate, which diagnostic test would be the MOST appropriate initial choice and why?
A patient presents with symptoms suggestive of H. pylori infection. Assuming all tests are equally accurate, which diagnostic test would be the MOST appropriate initial choice and why?
Which of the following is the MOST likely route of transmission for H. pylori?
Which of the following is the MOST likely route of transmission for H. pylori?
What is a potential long-term complication associated with H. pylori infection if left untreated?
What is a potential long-term complication associated with H. pylori infection if left untreated?
What is the primary purpose of gastric bypass surgery that can sometimes lead to dumping syndrome?
What is the primary purpose of gastric bypass surgery that can sometimes lead to dumping syndrome?
In acute pancreatitis, what is the primary mechanism through which the inflammatory response can lead to hypovolemic shock?
In acute pancreatitis, what is the primary mechanism through which the inflammatory response can lead to hypovolemic shock?
Why does excessive fat or oil intake particularly exacerbate pancreatic irritation?
Why does excessive fat or oil intake particularly exacerbate pancreatic irritation?
What is the most likely reason behind pancreatitis occurring post-ERCP (Endoscopic Retrograde Cholangiopancreatography)?
What is the most likely reason behind pancreatitis occurring post-ERCP (Endoscopic Retrograde Cholangiopancreatography)?
A patient presents with acute pancreatitis. Which assessment finding would be most indicative of potential peritonitis?
A patient presents with acute pancreatitis. Which assessment finding would be most indicative of potential peritonitis?
Besides gallstones and alcohol use, what other conditions or factors are known to potentially trigger acute pancreatitis?
Besides gallstones and alcohol use, what other conditions or factors are known to potentially trigger acute pancreatitis?
A patient presents with chronic abdominal pain, steatorrhea, and weight loss. A stool test reveals low fecal elastase levels. Which of the following is the MOST likely underlying pathology contributing to these findings?
A patient presents with chronic abdominal pain, steatorrhea, and weight loss. A stool test reveals low fecal elastase levels. Which of the following is the MOST likely underlying pathology contributing to these findings?
Which of the following pathophysiological processes is MOST directly responsible for the development of secondary diabetes mellitus in patients with chronic pancreatitis?
Which of the following pathophysiological processes is MOST directly responsible for the development of secondary diabetes mellitus in patients with chronic pancreatitis?
A patient with a history of chronic alcohol abuse and smoking is diagnosed with chronic pancreatitis. Which diagnostic finding would provide the STRONGEST evidence supporting this diagnosis?
A patient with a history of chronic alcohol abuse and smoking is diagnosed with chronic pancreatitis. Which diagnostic finding would provide the STRONGEST evidence supporting this diagnosis?
Which of the following conditions shares the MOST direct pathogenic link with the development of Primary Sclerosing Cholangitis (PSC)?
Which of the following conditions shares the MOST direct pathogenic link with the development of Primary Sclerosing Cholangitis (PSC)?
In the progression of Non-Alcoholic Fatty Liver Disease (NAFLD) to cirrhosis, which of the following pathophysiological mechanisms plays the MOST critical role in driving hepatocellular damage?
In the progression of Non-Alcoholic Fatty Liver Disease (NAFLD) to cirrhosis, which of the following pathophysiological mechanisms plays the MOST critical role in driving hepatocellular damage?
A patient is diagnosed with Primary Biliary Cholangitis (PBC). Which of the following best describes the PRIMARY pathological process involved in this condition?
A patient is diagnosed with Primary Biliary Cholangitis (PBC). Which of the following best describes the PRIMARY pathological process involved in this condition?
Which of the following genetic conditions leads to liver damage due to the accumulation of copper?
Which of the following genetic conditions leads to liver damage due to the accumulation of copper?
Which of the following mechanisms contributes MOST directly to the development of hepatocellular carcinoma (HCC) in the context of cirrhosis?
Which of the following mechanisms contributes MOST directly to the development of hepatocellular carcinoma (HCC) in the context of cirrhosis?
Flashcards
Dysphagia
Dysphagia
Difficulty swallowing.
Fistula (in Dysphagia context)
Fistula (in Dysphagia context)
Developmental defect creating an abnormal connection (e.g., between the esophagus and trachea).
Trigeminal Nerve (CN V) & Dysphagia
Trigeminal Nerve (CN V) & Dysphagia
Impaired chewing due to damage of CN V (Trigeminal nerve), affecting bolus formation.
Achalasia
Achalasia
Signup and view all the flashcards
Diverticulum
Diverticulum
Signup and view all the flashcards
Sliding Hiatal Hernia
Sliding Hiatal Hernia
Signup and view all the flashcards
Rolling Hiatal Hernia
Rolling Hiatal Hernia
Signup and view all the flashcards
Gastritis
Gastritis
Signup and view all the flashcards
Acute Pancreatitis
Acute Pancreatitis
Signup and view all the flashcards
Most Common Cause of Acute Pancreatitis
Most Common Cause of Acute Pancreatitis
Signup and view all the flashcards
Other Causes of Acute Pancreatitis
Other Causes of Acute Pancreatitis
Signup and view all the flashcards
ERCP & Pancreatitis
ERCP & Pancreatitis
Signup and view all the flashcards
Complications of Acute Pancreatitis
Complications of Acute Pancreatitis
Signup and view all the flashcards
Cholelithiasis Risk Factors
Cholelithiasis Risk Factors
Signup and view all the flashcards
Biliary Sludge
Biliary Sludge
Signup and view all the flashcards
Cholecystitis
Cholecystitis
Signup and view all the flashcards
Biliary Colic
Biliary Colic
Signup and view all the flashcards
Cholestasis
Cholestasis
Signup and view all the flashcards
Sepsis
Sepsis
Signup and view all the flashcards
Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD)
Signup and view all the flashcards
Crohn's Disease
Crohn's Disease
Signup and view all the flashcards
Ulcerative Colitis
Ulcerative Colitis
Signup and view all the flashcards
Toxic Megacolon
Toxic Megacolon
Signup and view all the flashcards
Celiac Disease
Celiac Disease
Signup and view all the flashcards
Acute Appendicitis
Acute Appendicitis
Signup and view all the flashcards
Fecaliths
Fecaliths
Signup and view all the flashcards
Pyloric Stenosis
Pyloric Stenosis
Signup and view all the flashcards
H. Pylori
H. Pylori
Signup and view all the flashcards
Urease
Urease
Signup and view all the flashcards
Urea Breath Test
Urea Breath Test
Signup and view all the flashcards
H. Pylori Triple Therapy
H. Pylori Triple Therapy
Signup and view all the flashcards
Pantoprazole
Pantoprazole
Signup and view all the flashcards
Bismuth Quadruple Therapy
Bismuth Quadruple Therapy
Signup and view all the flashcards
Dumping Syndrome
Dumping Syndrome
Signup and view all the flashcards
Chronic Pancreatitis
Chronic Pancreatitis
Signup and view all the flashcards
Low Fecal Elastase
Low Fecal Elastase
Signup and view all the flashcards
Etiology of Chronic Pancreatitis
Etiology of Chronic Pancreatitis
Signup and view all the flashcards
Manifestations of Chronic Pancreatitis
Manifestations of Chronic Pancreatitis
Signup and view all the flashcards
Cirrhosis
Cirrhosis
Signup and view all the flashcards
Primary Biliary Cholangitis (PBC)
Primary Biliary Cholangitis (PBC)
Signup and view all the flashcards
Primary Sclerosing Cholangitis (PSC)
Primary Sclerosing Cholangitis (PSC)
Signup and view all the flashcards
NAFLD Impact
NAFLD Impact
Signup and view all the flashcards
Study Notes
- Exam worth 25%
Dysphagia
- Defined as difficulty swallowing
- Can result from a developmental defect, such as a connection between the esophagus and trachea via a fistula
- Can be caused by neurological damage to cranial nerves
- Damage to cranial nerve V (trigeminal nerve) can cause difficulty chewing and forming a bolus
- Damage to cranial nerve X (vagus nerve) can cause issues with unconscious movements that allow food to go down smoothly
- Tumors from the outside can pressurize the GI tract, leading to obstruction
- Achalasia, or loss of muscle contraction in the lower esophagus, can cause food to get stuck
- Diverticulum, a pouch that forms within the inner layers of the GI tract, can trap food
- Fibrosis, where scar tissue contracts and constricts the airway causing Dysphagia
Hiatal Hernia
- Condition where part of the stomach protrudes into the upper GI tract
Sliding Hernia (95%)
- The sphincter slides upwards, and the stomach protrudes above the diaphragm
- Treated surgically by suturing it in place
Rolling Hernia (5%)
- The upper part of the stomach is above the small opening of the sphincter
- A small piece of the stomach may become necrotic and require surgical removal
- Pregnancy is a risk factor
- Manifestations include pyrosis (heartburn) and potential cancerous changes
Gastric Disorders
Gastritis
- Inflammation of the stomach lining caused by alcohol or medications
- Endoscopy reveals a red and inflamed lining
Peptic Ulcer
- Occurs in the stomach or duodenum
- Caused by H. pylori or overuse of NSAID drugs
Pyloric Stenosis
- Narrow opening between the stomach and duodenum
- Thickened pyloric sphincter can cause projectile vomiting in infants born before their due date
- Can also occur in adults with unresolved peptic ulcers that harden over time
Pathogenesis of H. Pylori
-
Transmitted via stomach-to-oral contact, such as sharing food with someone infected
-
Urease bacterium produces an enzyme that allows it to remain dormant
-
Urea turns into NH3, creating an alkaline environment, neutralizing stomach acid
-
Associated conditions include cancer/lymphoma of the stomach lining
-
Diagnosed via fast, specific, and noninvasive tests such as urea breath or stool sample
-
Medications include triple therapy (2 antibiotics and a proton pump inhibitor)
-
Clarithromycin is used, but resistance to H. pylori is emerging
-
Amoxicillin or metronidazole is given if penicillin allergy
-
Pantoprazole(PPI) is given to reduces uric acid in the stomach
-
Quadruple therapy with bismuth given if patient is immunocompromised
Dumping Syndrome
- Can occur after a gastric bypass to shrink the stomach for weight loss
- A part of the jejunum is bypassed, reducing nutrient absorption
- Accelerated gastric emptying causes food to leave the stomach too quickly
- Extreme diarrhea and rapid dehydration are common symptoms
- Rapid absorption pulls water and electrolytes out of cells, leading to dehydration
- Vitamin deficiencies can occur due to bypassing the jejunum
- Management includes avoiding sugar on an empty stomach and eating smaller, more frequent meals
Inflammatory Bowel Disease (IBS)
- A non-inflammatory condition affecting affects 15% of humans
- Manifestations include abnormal contractions of the large intestinal wall
- Changes in bowel habits
- Pain/discomfort in the left quadrant of the abdomen
- Males experience diarrhea, while females experience constipation
- Pain relieved after a bowel movement rules out rectal cancer
Predisposing Factors
- Stress interfering with the brain-gut axis (Vagus nerve controls peristaltic movement)
- Gut microbiome imbalances
- Broad-spectrum antibiotic use
- Food allergies
- 5-HT imbalance (serotonin)
- Splenic flexure syndrome: intestine kinks, trapping material
Intestinal Obstructions
- Inguinal hernia involves a twist
- More common in males due to heavy lifting
- Volvulus involves any twist leading to ischemia or necrosis due to lack of perforation
- When tissue dies, bacteria can cause sepsis
- The pathophysiology is an autoimmune response in white blood cells from the gut triggered by bacteria
Crohn's Disease
- Colposcopy reveals inflammation patches in the GI tract from mouth to anus
- Fissures (deep cracks/lesions) cause porridge-like stool
- Can result in malabsorption of nutrients in the small intestine, specifically the jejunum
- Fissures can cause a fistula combining the small & large intestine
Ulcerative Colitis
- Inflamed continuous lesions ulcerate innermost lining, causing bloody stool
- A lower GI bleed causes blood that is bright red
- Anemia results from iron loss
- Complications include toxic megacolon, requiring surgical removal
- Additional complications include rectovaginal and enterovesicle fistulas
Celiac Disease
- An autoimmune condition w/sensitivity to wheat, rye, barley (gluten = protein)
- The body creates antibodies after gluten is broken down into gliadin/binds w/tissue transglutaminase
Acute Appendicitis
- Inflamed appendix due to obstruction
- The appendix becomes reservoir of bacteria
- Is most often obstructed by fecaliths (hard fecal matter)
- Fecalith cuts the appendix, it can result in appendicitis
- Gastro patients can get appendicitis through an infection
- A neoplasm pinching the neck of the tumor
- Use of ozempic
- Manifestations include pain in the RLQ and belly button
- Firm upon palpation
Cholelithiasis
- More common in fair-skinned females/Indigenous
- Birth control(estrogen/progesterone): estrogen slows down the gallbladder, which leads to stone formation
- Biliary sludge often precedes cholelithiasis : calcium bilirubin ate, cholesterol micro crystals, and mucin.
- Usually a result of cholesterol delayed gallbladder emptying
- Larger calculi is worse
- Cholecystitis is an infection of the biliary system
- List the three types of cholelithiasis
- Which type is most common?
- Which type has a strong association with female hormones?
- Which type is associated with conditions that cause hemolysis?
- Define: biliary colic
- Locate the abdominal pain caused by cholelithiasis, and where it can radiate.
Treatment strategies
- Describe the goal of using an NG tube with intermittent suctioning.
- Describe lithotripsy
- Describe cholecystectomy
Cholestasis
- Gallstones in the gallbladder can get stuck in the cystic duct and cause obstruction
- Gallstones can also get stuck in the common bile duct
- Biles can get stuck in the duodenum, backing up into the liver
- Clay-colored stool can be observed due to blockage preventing excreatio
Acute Pancreatitis
- This medical conditions traps digestive enzymes, preventing proper nutrient absorption
- The digestive enzymes will start digesting the pancreas
- This results in inflammation then necrosis
- Precipitating factors:
- Activation of pancreatic enzymes inside the pancreatic ducts (e.g., trypsin, peptidase, elastase, amylase, lipase)
- Autodigestion of pancreatic tissue
- Tissue necrosis
- The pancreas becomes irritated from some source (or by eating)
- Number one trigger for acute pancreatitis is gall stones
- The second trigger is alcohol use
- High triglycerides is a third trigger
- Mumps, medications are factors
- Too much fat or oil will irritate the pancreas
- Post ERCP can trigger
ERCP
- Can trigger pancreas to irritate
- When it bends in the direction of the curving
- To check for an obstruction/irritation or inflammation of the procedure Causing an inflammatory response releasing plasma leading to hypovolemic shock/neurogenic shock
- When it bends in the direction of the curving
- You cannot vasocontrict right away
Complications
- DIC (Disseminated Intravascular Coagulation) ARDS (acute respiratory distress syndrome) Septic shock Peritinitis
- Blood test lipase and amylase test are required
Endoscopic Retrograde Cholangiopancreatography
Chronic Pancreatitis
- Long term inflammation of pancreas will lead to fibrosis in tests
Etiology:
- Alcohol Use
- Smoking
- Gallstones
Manifestations For Chronic Pancreatitis:
- Abdonimal Pain with vomiting/nausea
- Weight Loss
- No appetite (Can't absorb)
- Steatorrhea (fatty stool)
- Secondary Diabetes
Cirrhosis Triggers:
- Hep B, C, or D infections will most likely bleed
- Auto Immune
- AlH (autoimmune herpetitis)
- PBC (primary biliary cholangis) automatic destruction of intrahepatic bile ducts
- PSC (primary sclerosis cholangitis)
Metabolic:
- NAFLD (non alcoholic fatty liver disease)
- resistance to blood flow through liver that's scarred/ non working
- Hepatocytes are no longer working due to poor blood circulation leading to liver cell cancer
Genetics
- HH (Heredity Hemochromatosis) Iron over load
- Wilson's disease (copper over load in liver)
- AlAT anti-tripsin deficiency genetics that give you liver damage
Cholangitis (PBC):
- Immune destruction of bile ducts.
Functions Of The Liver
- Functions Explanation
- Digestion
- Excretion
- Nutrient storage, convert harmful chemicals, synthesis of new molecules, transform hormones.
- Bile neutralizes acids so fats can digest & be emulsified.
- Bile contains bile pigments
- Store fat as glycogen - transforms nutrients into others
- Liver removes ammonia circulation & turns into urea that pee’s out
Portal Circulation
- How blood affects the liver Step 1:
- Liver is scarred- blood can’t flow, high pressure to portal
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.