Podcast
Questions and Answers
What condition is indicated by the kidney secreting excess bicarbonate?
What condition is indicated by the kidney secreting excess bicarbonate?
- Hyponatraemia
- Hypokalemia
- Dehydration
- Alkalosis (correct)
Which of the following symptoms is commonly associated with severe cases in this condition?
Which of the following symptoms is commonly associated with severe cases in this condition?
- Confusion (correct)
- Nausea and vomiting
- Persistent cough
- Severe headache
What investigation is used to show a 'soup dish appearance' indicating significant gastric dilation?
What investigation is used to show a 'soup dish appearance' indicating significant gastric dilation?
- CT scan
- Barium meal (correct)
- MRI
- Ultrasound
In response to hypokalemia, which electrolyte exchange occurs to maintain balance?
In response to hypokalemia, which electrolyte exchange occurs to maintain balance?
What is the recommended intervention in all cases of this condition?
What is the recommended intervention in all cases of this condition?
What condition is characterized by the replacement of normal squamous epithelium with metaplastic columnar mucosa?
What condition is characterized by the replacement of normal squamous epithelium with metaplastic columnar mucosa?
Which complication of GERD is more likely to occur due to long-term reflux episodes?
Which complication of GERD is more likely to occur due to long-term reflux episodes?
What is the prognosis for patients with Barrett’s esophagus concerning the risk of developing adenocarcinoma?
What is the prognosis for patients with Barrett’s esophagus concerning the risk of developing adenocarcinoma?
Which symptom is associated with acute mucosal inflammation and typically seen in erosive esophagitis?
Which symptom is associated with acute mucosal inflammation and typically seen in erosive esophagitis?
What is the most common cause of strictures in the esophagus related to GERD?
What is the most common cause of strictures in the esophagus related to GERD?
What is a common symptom indicating advanced disease in a patient?
What is a common symptom indicating advanced disease in a patient?
Which lymph nodes are involved in lymphatic spread?
Which lymph nodes are involved in lymphatic spread?
What complication might result from recurrent laryngeal nerve infiltration?
What complication might result from recurrent laryngeal nerve infiltration?
What investigation is most sensitive for determining tumor depth?
What investigation is most sensitive for determining tumor depth?
What is a clinical sign often observed in patients with advanced carcinoma?
What is a clinical sign often observed in patients with advanced carcinoma?
What procedure should be urgently performed in a middle-aged patient with dysphagia or odynophagia?
What procedure should be urgently performed in a middle-aged patient with dysphagia or odynophagia?
Which statement about the prognosis of advanced disease is correct?
Which statement about the prognosis of advanced disease is correct?
What is an indication for staging investigations?
What is an indication for staging investigations?
What is the most common timeframe for ulcers to heal with proper treatment?
What is the most common timeframe for ulcers to heal with proper treatment?
Which substances should be eliminated to aid in the treatment of duodenal ulcers?
Which substances should be eliminated to aid in the treatment of duodenal ulcers?
Which component is NOT part of the triple therapy for eradication of H.pylori?
Which component is NOT part of the triple therapy for eradication of H.pylori?
What is considered a main disadvantage of medical treatment for duodenal ulcers?
What is considered a main disadvantage of medical treatment for duodenal ulcers?
Which is an indication for surgical treatment of gastric ulcers?
Which is an indication for surgical treatment of gastric ulcers?
Which of the following represents a strategy to prevent ulcer relapse?
Which of the following represents a strategy to prevent ulcer relapse?
What is one of the main surgical options for a patient with chronic duodenal ulcers?
What is one of the main surgical options for a patient with chronic duodenal ulcers?
What is a key component of quadruple therapy for H.pylori eradication?
What is a key component of quadruple therapy for H.pylori eradication?
Which diagnostic method is considered the gold standard for diagnosing GERD and NERD?
Which diagnostic method is considered the gold standard for diagnosing GERD and NERD?
What must be excluded before diagnosing GERD via upper endoscopy?
What must be excluded before diagnosing GERD via upper endoscopy?
Which of the following is a reason for providing palliative treatment?
Which of the following is a reason for providing palliative treatment?
What indicates a low pH reading in 24-hour pH studies for diagnosing GERD?
What indicates a low pH reading in 24-hour pH studies for diagnosing GERD?
Which diagnostic method has no role in diagnosing GERD?
Which diagnostic method has no role in diagnosing GERD?
What surgical approach is associated with performing a three-stage esophagectomy?
What surgical approach is associated with performing a three-stage esophagectomy?
What is the value of esophageal manometry in the context of GERD?
What is the value of esophageal manometry in the context of GERD?
In which scenario would a one-field oesophago-gastric resection be indicated?
In which scenario would a one-field oesophago-gastric resection be indicated?
What is a component of the neoadjuvant therapy plus curative approach?
What is a component of the neoadjuvant therapy plus curative approach?
What is a potential negative result of upper endoscopy when diagnosing NERD?
What is a potential negative result of upper endoscopy when diagnosing NERD?
Why is impedance pH metry included in the diagnostic approach for GERD?
Why is impedance pH metry included in the diagnostic approach for GERD?
Which incision is used to mobilize the cervical esophagus in the treatment of cervical esophageal cancer?
Which incision is used to mobilize the cervical esophagus in the treatment of cervical esophageal cancer?
What does the presence of alarm symptoms indicate in a patient with chronic GERD?
What does the presence of alarm symptoms indicate in a patient with chronic GERD?
What technique is commonly used for the best palliation in palliative treatment?
What technique is commonly used for the best palliation in palliative treatment?
Which of the following complications would most likely require bad general condition for a surgical intervention?
Which of the following complications would most likely require bad general condition for a surgical intervention?
What type of esophagectomy is indicated for lesions below the carina?
What type of esophagectomy is indicated for lesions below the carina?
Flashcards
Erosive Esophagitis
Erosive Esophagitis
Erosive esophagitis is an inflammation of the lining of the esophagus caused by GERD. It occurs when stomach acid repeatedly irritates the esophageal lining, leading to damage and ulceration.
Esophageal Stricture
Esophageal Stricture
A narrowing of the esophagus caused by scar tissue formation due to chronic acid reflux. It makes it difficult to swallow.
Barrett's Esophagus (BE)
Barrett's Esophagus (BE)
Barrett's esophagus (BE) is a condition where the normal lining of the lower esophagus is replaced by a different type of lining similar to the stomach or intestines. It's a precancerous condition, meaning it can increase the risk of esophageal cancer over time.
Lower Esophageal Sphincter (LES)
Lower Esophageal Sphincter (LES)
Signup and view all the flashcards
Common GERD Symptoms
Common GERD Symptoms
Signup and view all the flashcards
Dysphagia
Dysphagia
Signup and view all the flashcards
Odynophagia
Odynophagia
Signup and view all the flashcards
Esophagogastroduodenoscopy (EGD)
Esophagogastroduodenoscopy (EGD)
Signup and view all the flashcards
Endoscopic Ultrasound (EUS)
Endoscopic Ultrasound (EUS)
Signup and view all the flashcards
Tracheoesophageal Fistula
Tracheoesophageal Fistula
Signup and view all the flashcards
Virchow's Lymph Node
Virchow's Lymph Node
Signup and view all the flashcards
CT Scan of Chest and Abdomen
CT Scan of Chest and Abdomen
Signup and view all the flashcards
Patient Fitness Assessment
Patient Fitness Assessment
Signup and view all the flashcards
Upper Endoscopy with Biopsy
Upper Endoscopy with Biopsy
Signup and view all the flashcards
24-hour Esophageal pH Studies
24-hour Esophageal pH Studies
Signup and view all the flashcards
Diagnosing GERD with pH Studies
Diagnosing GERD with pH Studies
Signup and view all the flashcards
24-hour pH Studies for NERD & Atypical Symptoms
24-hour pH Studies for NERD & Atypical Symptoms
Signup and view all the flashcards
Impedance pH Metry
Impedance pH Metry
Signup and view all the flashcards
Esophageal Manometry
Esophageal Manometry
Signup and view all the flashcards
Barium Swallow (Trendelenburg position)
Barium Swallow (Trendelenburg position)
Signup and view all the flashcards
Barium Swallow for GERD Diagnosis
Barium Swallow for GERD Diagnosis
Signup and view all the flashcards
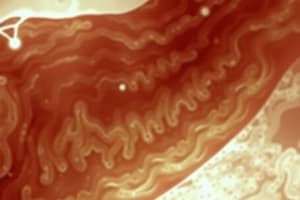
Dilated Stomach
Dilated Stomach
Signup and view all the flashcards
Succusion Splash
Succusion Splash
Signup and view all the flashcards
Visible Peristaltic Waves
Visible Peristaltic Waves
Signup and view all the flashcards
Hypokalemia
Hypokalemia
Signup and view all the flashcards
Alkalosis
Alkalosis
Signup and view all the flashcards
Curative Esophagectomy
Curative Esophagectomy
Signup and view all the flashcards
Neoadjuvant Therapy
Neoadjuvant Therapy
Signup and view all the flashcards
Adjuvant Therapy
Adjuvant Therapy
Signup and view all the flashcards
Three-Stage Esophagectomy (McKeown Operation)
Three-Stage Esophagectomy (McKeown Operation)
Signup and view all the flashcards
Two-Stage Esophagectomy (Ivor-Lewis Operation)
Two-Stage Esophagectomy (Ivor-Lewis Operation)
Signup and view all the flashcards
One-Field Oesophago-Gastric Resection
One-Field Oesophago-Gastric Resection
Signup and view all the flashcards
Palliative Treatment
Palliative Treatment
Signup and view all the flashcards
Endoscopic Stenting
Endoscopic Stenting
Signup and view all the flashcards
Chronic Duodenal Ulcer Treatment
Chronic Duodenal Ulcer Treatment
Signup and view all the flashcards
Histamine (H2) Blockers
Histamine (H2) Blockers
Signup and view all the flashcards
Sucralfate
Sucralfate
Signup and view all the flashcards
Triple Therapy (H. pylori Eradication)
Triple Therapy (H. pylori Eradication)
Signup and view all the flashcards
Proton Pump Inhibitor (PPI)
Proton Pump Inhibitor (PPI)
Signup and view all the flashcards
Intractability (Chronic Gastric Ulcer)
Intractability (Chronic Gastric Ulcer)
Signup and view all the flashcards
Indications for Surgery (Chronic Gastric Ulcer)
Indications for Surgery (Chronic Gastric Ulcer)
Signup and view all the flashcards
Study Notes
Upper GIT Surgery
- Esophagus - page 1
- Bariatric surgery - page 1
- Stomach - page 1
- Minimally invasive surgeries - page 1
- Hepatobiliary surgery - page 1
- Gall bladder - page 1
- Pancreas - page 1
- Liver - page 1
- Spleen - page 1
Esophagus
- Gastroesophageal reflux disease - page 2
- Hiatus Hernia - page 2
- Esophageal Webs - page 2
- Achalasia of the Esophagus - page 2
- Esophageal Diverticula - page 2
- Esophageal Tumors - page 2
- Esophageal Perforation - page 2
Upper GIT Surgery
- Upper esophageal sphincter (UES) - page 3
- Lower esophageal sphincter (LES) - page 3
- Muscularis propria of upper 1/3 - page 3
- Peristalsis - page 3
- Primary - page 3
- Secondary - page 3
- Tertiary - page 3
- Dysphagia - page 3
- Most of esophageal lesions - page 3
- Benign Lesions - page 3
- Diseases of the Esophagus - page 3
- SCC - page 3
- Malignant lesions - page 3
GERD (Gastroesophageal reflux Disease)
- Factors preventing or causing GERD - page 4
- Lower esophageal sphincter (LES) - page 4
- Components of LES - page 4
- Esophageal clearance - page 4
- Delayed gastric emptying - page 4
- Age, All ages, but M/C > 40year -Sex: ♂ = - GERD presentations (3 classes of symptoms) - page 4
- Typical symptoms - page 4
- Alarming S/S - page 4
- Atypical symptoms - page 4
- Complications of GERD - page 4
UPPER GIT SURGERY
- Investigations- page 5
- Diagnosis GERD - page 5
- Diagnosis of GERD - page 5
- Diagnosis of NERD/Atypical symptoms - page 5
UPPER GIT SURGERY
- Diagnostic evaluation - page 6
- Conservative/Medical ttt - page 6
- Goals of therapy - page 6
- Preventive complications - page 6
- Therapy - page 6
- Surgery - page 6
- Treatment - page 6
- Endoscopic ttt - page 6
- Ttt of complications - page 6
H2-Receptor Antagonists (H2B) - page 7
- Ranitidine 150-300 mg tab - page 7
- Famotidine 20-40 mg tab - page 7
- Proton pump inhibitor (PPI) - page 7
- Pantoprazole - page 7
- Esomeprazole - page 7
- Ccc - page 7
Laparoscopic fundoplication - page 7
- Types fundoplication - page 7
- Complications- page 7
Hiatus Hernia - page 8
- Type I (80%) - page 8
- Sliding hiatal hernia - page 8
- Symptomatic - page 8
- Type II - page 8
- Paraesophageal hiatus hernia - page 8
- GEJ in abdomen - page 8
- Complications: - page 8
- Treatment: - page 8
- Esophageal Webs - page 8
- Circumferential mucosal folds - page 8
- Etiology: - page 8
- Esophageal Web Upper esophagus - page 8
Achalasia of the Esophagus - page 9
- Pathophysiology & Etiology - page 9
- Chest X-ray - page 9
- Upper GIT Endoscopy - page 9
- LES pressure - page 9
- Tertiary contractions - page 9
- Lost peristalsis - page 9
- Fundic air bubble - page 9
- Bird or Parrot Beak: - page 9
- Sigmoid Esophagus - page 9
- Differential diagnosis - page 9
Treatment of achalasia - page 10
- Pharmacotherapy (Botulinum injection) - page 10
- Method - page 10
- Complications - page 10
- Pneumatic balloon dilatation - page 10
- Method- page 10
- Disadvantages- page 10
- Indications - page 10
- Surgery (Open - laparscopic) - page 10
- Open - page 10
- Laparoscopic - page 10
Esophageal Diverticula - page 11
- Site - page 11
- Etiology - page 11
- Clinical Picture - page 11
- Complications - page 11
- Treatment - page 11
- Diagnosis - page 11
Esophageal Tumors - page 12
- Benign Esophageal Neoplasms - page 12
- Malignant Esophageal Neoplasms - page 12
- PDFs - page 12
- Radiology - page12
- Mac -page 12
- Spread -page12
Investigations- page 13
- For primary lesion - page 13
- For staging & to assess operability - page 13
- Assessment Patient Fitness - page 13
Palliative treatment - page 14
- Indications - page 14
- Palliative measures - page 14
- Neoadjuvant therapy - page 14
Complications of Esophagectomy - page 15
- Early Postoperative - page 15
- Late Postoperative - page 15
- Siewert classification - page 15
- Causes - page 15
- Investigations - page 15
- Lines of treatment - page 15
Grades of Obesity - page 16
- Grades of Obesity - page 16
- Co-morbidities of obesity - page 16
Medical complications (co-morbidities of obesity) - page 17
- Type II DM - page 17
- Hypertension - page 17
- Hypertriglyceridemia & hypercholesterolemia - page 17
- CVS - page 17
- Respirtory - page 17
- GIT - page 17
- Other complications - page 17
- Other grading system - page 17
Types and Indications of Bariatric Surgery - page 18
- Restrictive Surgery - page 18
- Laparoscopic adjustable gastric banding (LAGB) - page 18
- Gastric placation - page 18
- Bulk eaters - page 18
- Indications - page 18
- Procedure - page 18
- Advantages - page 18
- Disadvantages & Complications - page 18
- Vertical band gastroplasty (VBG) - page 18
- Combined restrictive and malabsorptive - page 18
Technique: Sleeve Gastrectomy - page 19
- Advantages - page 19
- Disadvantages & complications - page 19
- Late complications - page 19
Roux-en-Y gastric bypass (RYGB) - page 20
- One Anastomosis (Mini) Gastric bypass (OAGB) - page 20
- Technique - page 20
- Ccc & diadv- page 20
- Outcome - page 20
Malabsorptive Surgery - page 21
- Bilio-pancreatic Diversion (BPD) - page 21
- BPD with duodenal switch DS - page 21
Acute Gastric Dilatation - page 23
- Acute Peptic Ulcer - page 23
- Chronic Duodenal ulcer - page 24
- Chronic gastric ulcer - page 24
- Bleeding peptic ulcer - page 24
- Perforated peptic ulcer - page 24
- Gastric outlet obstruction (GOO)- page 24
Chronic Duodenal Ulcer - page 25
- Age, Sex - page 25
- Etiology - page 25
- Patho - page 25
- Number - page 25
- Site -page 25
Chronic Gastric Ulcers - page 25
- Incidence - page 25
- Etiology - page 25
- Patho - page 25
- C/O(Chronic Duodenal Ulcer) -page 26
- O/E -page 26
- Inv - page 26
- Diagnosis - page 26
- TTT- page 26
Bleeding peptic ulcer - page 30
- Inv - page 30
- Ttt - page 30
Perforated peptic ulcer - page 30
- Causes - page 30
- Investigations - page 30
- Lines of treatment - page 30
Pyloric Stenosis - page 33
- C/O - page 33
- Clinical Picture - page 33
- Investigations - page 33
- Treatment - page 33
Tumors of the Stomach - page 34
- Benign Esophageal Neoplasms- page 34
- Malignant Esophageal Neoplasms- page 34
- PDFs - page 34
- Pathology - page 34
- Spread - page 34
- Prognosis - page 34
Carcinoma of the stomach - page 34
- Benign Esophageal Neoplasms- page 34
- Malignant Esophageal Neoplasms- page 34
- PDFs - page 34
- Epidemiology - page 34
- Pathology -page 34
Pathology of Tumors of the Stomach - page 35
- Gross pathology - page 35
- Microscopic picture - page 35
- Intestinal Type - page 35
Investigations - page 36
- For primary lesion - page 36
- For staging & to assess operability - page 36
- Gastric carcinoma - page 36
Tumours of the Body & Fundus - page 37
- Principles of radical surgery - page 37
- Treatment - page 37
Carcinoma of the Body and Tail of the Pancreas - page 38
- Epidemiology - page 38
- Etiology - page 38
- Pathology - page 38
- Clinical Picture - page 38
- Malignant Obstructive Jaundice- page 38
Pathology of Pancreatic Tumors - page 39
- Gross pathology - page 39
- Microscopic picture - page 39
- Intestinal Type - page 39
- Diffuse Type - page 39
- Presentation usually precedes metastasis - page 39
- Investigations - Page 39
- Routine laboratory of O.J. - Page 39
- Abdominal U.S - Page 39
- Other investigations - Page 39
Pancreatic Ascites - page 39
- Def - page 39
- Etiology - page 39
- Pathology - page 39
- Clinical picture- page 39
- Investigations -Page 39
- Treatment - page 39
Chronic Duodenal Ileus - page 39
- Definition - page 39
- Etiology - page 39
- C/P - page 39
- Investigations - page 39
- Treatment - page 39
Haematemesis - page 40
- Causes - page 40
- Investigations - page 40
- Treatment - page 40
Miscellaneous causes of haematemesis - page 41
- Mallory Weiss tear - page 41
- Dieulafoy Gastric Lesion - page 41
- Aortic enteric fistula- page 41
Postgastrectomy Syndromes - page 42
- Reflux Alkaline - page 42
- Afferent Loop Syndrome - page 42
- Dumping Syndrome - page 42
- Treatments of dumping syndrome - page 42
- Nutritional disturbances - page 42
Minimal Invasive Surgery (MIS) - page 43
- Small wounds - page 43
- Minimizing the surgical trauma - page 43
- Minimizing blood loss - page 43
- All these factors- page 43
Preparation for laparoscopic or robotic surgery - page 44
- History - page 44
- Examination - page 44
- Pre-medication & Prophylaxis - page 44
- Urinary catheters & nasogastric tubes - page 44
- Informed consent - page 44
Surgical Principles of MIS - page 45
- Meticulous care in the creation of a pneumoperitoneum - page 45
Laparoscopic Instruments- page 46
- Disadvantages & Complications- page 46
- Complications: - page 46
- Contraindications- page 46
Laparoscopic staging for abdominal malignancies - page 47
- Aim - page 47
- Indications page 47
- Contraindications- page 47
- Early disease- page 47
- Local disease- page 47
- Advanced disease- page 47
- Metastatic disease- page 47
Tumours of the Body & Fundus - page 47
Bile Duct Injury- page 58
- Etiology - page 58
- Presentation (oj dt traumatic stricture)- page 58
- Investigations - page 58
- Treatment - page 58
Primary Sclerosing Cholangitis (PSC) - page 59
- Etiopathophysiology - page 59
- Epidemiology - page 59
- Diagnosis - page 59
Carcinoma of the Gallbladder - page 59
- Etiology - page 59
- Pathology - page 59
- Clinical Picture - page 59
- Treatment - page 59
Calcular Obstructive Jaundice - page 54
- Clinical picture - page 54
- Sequelae & Complications - page 54
Lab of Chronic Calcular Cholecystitis - page 52
- Investigations - page 52
Chronic Calcular Cholecystitis - page 50
- Acute Calcular Cholecystitis - page 50
- Complications of Acute - page 51
- Etiology- page 51
- Calcular Obstructive Jaundice - page 53
- Clinical C/O - page 53
- Common bile duct stones - page 53
- Sequelae & Complications - page 54
- Differential diagnosis of calcular obstructive jaundice - page 54
Pyogenic Liver Abscess - page 80
- Etiology - page 80
- Presentation - page 80
- Inv- page 80
- Ttt -page 80
- CT/US- guided percutaneous aspiration - page 81
- Medical treatment - page 81
- Complications - page 81
Benign Liver Tumors - page 82
- Liver Hemangioma - page 82
- Focal nodular hyperplasia - page 82
- Hepatocellular adenoma (HCA) - page 82
Hepatic focal lesions - page 77
- Cystic - page 77
- solid - page 77
- Malignant - page 77
- Secondary (metastatic) - page 77
- Liver cysts - page 77
Hepatocellular Carcinoma (HCC) - page 84
Secondary Liver Tumors - page 88
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.