Podcast
Questions and Answers
What is the primary function of the alkaline mucus barrier in the gastroduodenal mucosal system?
What is the primary function of the alkaline mucus barrier in the gastroduodenal mucosal system?
Which of the following mechanisms contributes to the maintenance of the epithelial cell barrier in the gastroduodenal mucosal system?
Which of the following mechanisms contributes to the maintenance of the epithelial cell barrier in the gastroduodenal mucosal system?
What is the main function of HCO3- in the gastroduodenal mucosal system?
What is the main function of HCO3- in the gastroduodenal mucosal system?
In what way does the high rate of mucosal blood flow contribute to the protection of the gastroduodenal mucosa?
In what way does the high rate of mucosal blood flow contribute to the protection of the gastroduodenal mucosa?
Signup and view all the answers
What is the approximate time frame for epithelial cell turnover in the gastroduodenal mucosa?
What is the approximate time frame for epithelial cell turnover in the gastroduodenal mucosa?
Signup and view all the answers
What type of cells are involved in restitution?
What type of cells are involved in restitution?
Signup and view all the answers
Which of the following is NOT a result of prostaglandins generated by COX1 activity?
Which of the following is NOT a result of prostaglandins generated by COX1 activity?
Signup and view all the answers
What is the immediate consequence of cell damage in the GI epithelium?
What is the immediate consequence of cell damage in the GI epithelium?
Signup and view all the answers
What is the role of arachidonic acid in barrier regulation?
What is the role of arachidonic acid in barrier regulation?
Signup and view all the answers
What is the effect of COX2 activity in the context of barrier regulation?
What is the effect of COX2 activity in the context of barrier regulation?
Signup and view all the answers
How does restitution differ from normal epithelial cell coverage?
How does restitution differ from normal epithelial cell coverage?
Signup and view all the answers
Which of these events occurs in a sequential order starting with cell damage?
Which of these events occurs in a sequential order starting with cell damage?
Signup and view all the answers
Which of these factors directly contribute to the inflammatory response in the GI tract?
Which of these factors directly contribute to the inflammatory response in the GI tract?
Signup and view all the answers
Which of the following gastrointestinal structures can send afferent signals to the Vomiting Center?
Which of the following gastrointestinal structures can send afferent signals to the Vomiting Center?
Signup and view all the answers
What effect do non-specific NSAIDs have on the gastrointestinal tract?
What effect do non-specific NSAIDs have on the gastrointestinal tract?
Signup and view all the answers
What is the primary mechanism by which bloodborne toxins induce vomiting?
What is the primary mechanism by which bloodborne toxins induce vomiting?
Signup and view all the answers
Which species are physiologically capable of vomiting?
Which species are physiologically capable of vomiting?
Signup and view all the answers
What is the role of prestatcyclin in the cardiovascular system?
What is the role of prestatcyclin in the cardiovascular system?
Signup and view all the answers
Which of the following is NOT a potential cause of vomiting?
Which of the following is NOT a potential cause of vomiting?
Signup and view all the answers
What is the primary difference between COX-2-specific inhibitors and non-specific NSAIDs?
What is the primary difference between COX-2-specific inhibitors and non-specific NSAIDs?
Signup and view all the answers
What is the physiological effect of thromboxane A2?
What is the physiological effect of thromboxane A2?
Signup and view all the answers
Which of the following is NOT a source of circulating toxins that may trigger the chemoreceptor trigger zone (CTZ)?
Which of the following is NOT a source of circulating toxins that may trigger the chemoreceptor trigger zone (CTZ)?
Signup and view all the answers
What is the primary physiological function of the chemoreceptor trigger zone (CTZ)?
What is the primary physiological function of the chemoreceptor trigger zone (CTZ)?
Signup and view all the answers
During the retching stage of vomiting, which of the following occurs?
During the retching stage of vomiting, which of the following occurs?
Signup and view all the answers
Which of the following events is responsible for the characteristic forceful expulsion of vomit during the vomiting stage?
Which of the following events is responsible for the characteristic forceful expulsion of vomit during the vomiting stage?
Signup and view all the answers
Which of the following best describes the difference between vomiting and regurgitation?
Which of the following best describes the difference between vomiting and regurgitation?
Signup and view all the answers
Which of these is a potential metabolic consequence of protracted vomiting?
Which of these is a potential metabolic consequence of protracted vomiting?
Signup and view all the answers
What is the role of the vagus nerve (VC) in the process of vomiting?
What is the role of the vagus nerve (VC) in the process of vomiting?
Signup and view all the answers
Which of the following is a characteristic of projectile vomiting?
Which of the following is a characteristic of projectile vomiting?
Signup and view all the answers
In the early stage of protracted vomiting, what is the primary cause of metabolic alkalosis?
In the early stage of protracted vomiting, what is the primary cause of metabolic alkalosis?
Signup and view all the answers
What is the primary mechanism by which hypokalemia develops during the early stage of protracted vomiting?
What is the primary mechanism by which hypokalemia develops during the early stage of protracted vomiting?
Signup and view all the answers
Which of the following is NOT a physiological system contributing to the gastroduodenal mucosal barrier?
Which of the following is NOT a physiological system contributing to the gastroduodenal mucosal barrier?
Signup and view all the answers
Which of the following is NOT a stimulus to increase circulating aldosterone?
Which of the following is NOT a stimulus to increase circulating aldosterone?
Signup and view all the answers
Study Notes
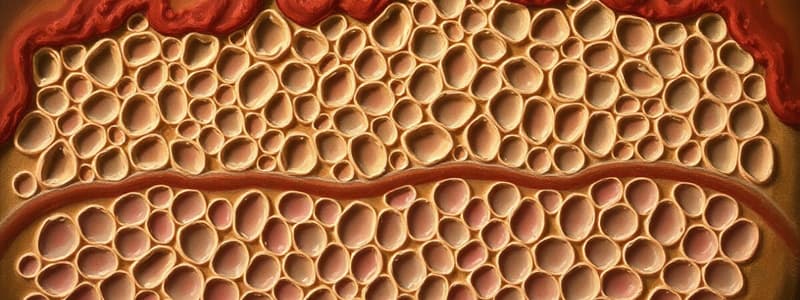
Gastroduodenal Mucosal Barrier
- The gastroduodenal mucosal barrier protects the epithelium from gastric acid
- It is maintained by 3 physiological systems
Alkaline Mucus Barrier
- Secretion of mucus from surface mucus cells
- Secretion of bicarbonate from surface mucus cells into the mucus layer
- Stomach: Chloride/bicarbonate exchange by surface epithelium
- Duodenum: CFTR and Chloride/bicarbonate exchange
High Rate of Mucosal Blood Flow
- Supports the metabolic rate of epithelial cells
- Provides a source of bicarbonate
- Removes hydrogen ions crossing tight junctions
- The hydrogen ions are diluted and neutralized by the extracellular fluid.
Epithelial Cell Barrier, Restitution, and Turnover
- Tight junctions restrict the exposed apical/luminal surface
- Rapid cell turnover occurs every 3-5 days
- Restitution after damage occurs within minutes
Role of Prostaglandins
- Local damage to the GI epithelium (acid, abrasion) and submucosal elements (fibroblasts) release phospholipase A, which generates arachidonic acid.
- Cells containing cyclooxygenase 1 and 2 (COX1 and COX2) generate prostaglandins from arachidonic acid.
- COX1 activity stimulates all three physiological barriers
- COX2 activity is important in pain perception
Ulcerogenic Action of Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- Non-specific NSAIDs (aspirin, phenylbutazone, ibuprofen) inhibit both COX enzymes.
- This leads to pain relief, but reduces alkaline mucus production, blood flow, and restitution.
- COX-2 specific inhibitors (like Rimadyl for dogs) provide pain relief without impacting protective prostaglandins.
Pathophysiology of Vomiting
- Species differences exist in the ability to vomit.
- Carnivores and omnivores can vomit, while ruminants (physiological regurgitation of cud and pathological abomasal reflux) have different characteristics.
- Horses, rabbits, and guinea pigs (other rodents) cannot vomit.
Vomiting Reflex
- The vomiting center is located in the medulla's reticular formation.
- It mediates nausea, retching, and vomiting.
- Inputs to the vomiting center include: Vestibular apparatus, Visceral afferents, and Blood-born toxins (via the chemoreceptor trigger zone).
Process of Vomiting
- Vomiting occurs in stages: nausea, retching, and vomiting.
- Nausea includes experiences like salivation and proximal stomach relaxation.
- Retching is a preparatory phase involving stomach relaxation and pylorus contraction.
- Vomiting involves sustained abdominal muscle contraction and forced inspiratory movement.
- The pressure gradient created helps expel the vomitus from the stomach to the esophagus.
Metabolic Consequences of Protracted Vomiting
- Protracted vomiting leads to hypovolemia due to loss of isotonic, acidic fluid in vomitus.
- Early stage results in metabolic alkalosis (loss of gastric HCl, increased blood pH), hypokalemia (K+ loss in vomitus and urine), and a shift of H+ ions into cells.
- Late stage leads to metabolic acidosis due to hypovolemia, decreased tissue perfusion, and anaerobic glycolysis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the gastroduodenal mucosal system, focusing on functions, protective mechanisms, and cell turnover. This quiz covers important aspects such as the roles of alkaline mucus, HCO3-, and the impact of blood flow on mucosal protection. Prepare to delve into cellular processes and the effects of different compounds in gastric health.