Podcast
Questions and Answers
What distinguishes juxtamedullary nephrons from cortical nephrons?
What distinguishes juxtamedullary nephrons from cortical nephrons?
- Juxtamedullary nephrons are found primarily in the cortex.
- Juxtamedullary nephrons have a longer loop of Henle and a vasa recta. (correct)
- Juxtamedullary nephrons lack a vasa recta.
- Juxtamedullary nephrons have a shorter loop of Henle.
Which statement about the countercurrent mechanism is correct?
Which statement about the countercurrent mechanism is correct?
- It does not play a role in urine concentration.
- It is only found in cortical nephrons.
- It is enhanced by the proximity of the loop of Henle and the vasa recta. (correct)
- It involves fluid flowing in the same direction in the loop of Henle.
What role does the ascending limb of the loop of Henle play in the countercurrent mechanism?
What role does the ascending limb of the loop of Henle play in the countercurrent mechanism?
- It limits the flow of fluids to the collecting duct.
- It helps to increase osmolarity by absorbing water.
- It is permeable to salts but not water. (correct)
- It is highly permeable to both salts and water.
How does the countercurrent system affect osmolarity in the kidney?
How does the countercurrent system affect osmolarity in the kidney?
What consequence does the high osmolarity in the inner medulla have on urine composition?
What consequence does the high osmolarity in the inner medulla have on urine composition?
What is the primary function of the proximal convoluted tubule (PCT)?
What is the primary function of the proximal convoluted tubule (PCT)?
How does the descending limb of the Loop of Henle function?
How does the descending limb of the Loop of Henle function?
What role do ADH and aldosterone play in the distal convoluted tubule (DCT)?
What role do ADH and aldosterone play in the distal convoluted tubule (DCT)?
What happens to urine concentration if the proximal convoluted tubule (PCT) is removed?
What happens to urine concentration if the proximal convoluted tubule (PCT) is removed?
Which process occurs in the distal convoluted tubule (DCT)?
Which process occurs in the distal convoluted tubule (DCT)?
What characterizes the counter-current mechanism in urine concentration?
What characterizes the counter-current mechanism in urine concentration?
What is the main role of the collecting duct?
What is the main role of the collecting duct?
Which of the following statements is true regarding the Loop of Henle?
Which of the following statements is true regarding the Loop of Henle?
Which cells are responsible for forming the filtration membrane in the Bowman's capsule?
Which cells are responsible for forming the filtration membrane in the Bowman's capsule?
What defines tubular secretion in the renal system?
What defines tubular secretion in the renal system?
Flashcards
Cortical Nephron
Cortical Nephron
A type of nephron with a shorter loop of Henle and lacking a vasa recta.
Juxtamedullary Nephron
Juxtamedullary Nephron
A type of nephron with a longer loop of Henle and a vasa recta.
Countercurrent Mechanism
Countercurrent Mechanism
A process in the nephron that helps concentrate urine by using opposite flows in the loop of Henle and vasa recta.
Loop of Henle
Loop of Henle
Signup and view all the flashcards
Vasa Recta
Vasa Recta
Signup and view all the flashcards
Glomerular Filtration
Glomerular Filtration
Signup and view all the flashcards
Tubular Reabsorption
Tubular Reabsorption
Signup and view all the flashcards
Loop of Henle
Loop of Henle
Signup and view all the flashcards
Counter-current Mechanism
Counter-current Mechanism
Signup and view all the flashcards
Distal Convoluted Tubule (DCT)
Distal Convoluted Tubule (DCT)
Signup and view all the flashcards
Collecting Duct
Collecting Duct
Signup and view all the flashcards
Tubular Secretion
Tubular Secretion
Signup and view all the flashcards
Proximal Convoluted Tubule (PCT)
Proximal Convoluted Tubule (PCT)
Signup and view all the flashcards
Removal of PCT
Removal of PCT
Signup and view all the flashcards
Renal Calculi
Renal Calculi
Signup and view all the flashcards
Study Notes
Excretory Products and Their Elimination
- The lecture focuses on excretory products and their elimination, specifically urine formation and the counter-current mechanism
- The session is important as it's a key topic in examinations
- The focus is on urine formation, which includes glomerular filtration, tubular reabsorption, and tubular secretion
Glomerular Filtration
- The process where the blood is filtered through the glomerular filtration membrane and forms filtrate
Tubular Reabsorption
- Essential nutrients and a large volume of water are reabsorbed from the filtrate in the proximal convoluted tubule (PCT)
- PCT is lined with simple cuboidal brush-bordered epithelium, which increases surface area for reabsorption
- The PCT reabsorbs 70-80% of water and electrolytes, as well as essential nutrients
- The PCT also plays a role in maintaining pH and ionic balance by secreting hydrogen ions, ammonia, and reabsorbing bicarbonate ions
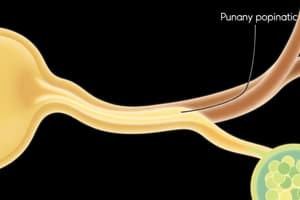
Loop of Henle
- The descending limb is permeable to water only, while the ascending limb is permeable to electrolytes only
- Water moves out of the descending limb due to the high osmolality of the interstitial fluid, resulting in concentrated filtrate
- The ascending limb reabsorbs electrolytes, leading to dilute filtrate
- Sodium ion reabsorption is active, while chloride ion reabsorption is passive
Distal Convoluted Tubule (DCT)
- The DCT is the site for conditional reabsorption, regulated by hormones like ADH (released from the posterior pituitary) and aldosterone (from the adrenal cortex)
- ADH and aldosterone regulate water and electrolyte reabsorption in response to body fluid concentrations
- DCT also secretes potassium and hydrogen ions, while reabsorbing bicarbonate
Collecting Duct
- This duct extends from the cortex to the medulla, reabsorbing significant amounts of water to form concentrated urine
- The collecting duct also plays a role in pH and ionic balance through the selective secretion of hydrogen and potassium ions
- Urea, a waste product, is secreted from the collecting duct and reabsorbed in the ascending limb of Henle's loop, maintaining the high osmolality of the interstitial fluid
Counter-Current Mechanism
- The counter-current mechanism is a process that concentrates urine in the medulla
- It involves the counter-current flow of filtrate in the loop of Henle and the counter-current flow of blood in the vasa recta
- The mechanism creates a concentration gradient in the medulla, which helps in reabsorbing water from the collecting duct, thereby concentrating the urine
Key Points to Remember
- Tubular secretion occurs in PCT, DCT, and the collecting duct
- Renal calculi are crystals of oxalate and calcium salts that form stones in the kidney
- Podocytes are specialized cells of the Bowman's capsule that form the filtration membrane
Removal of PCT
- The removal of the PCT results in a significantly diluted urine due to the reduced reabsorption of water and electrolytes.
Types of Nephrons
-
Cortical nephrons have a shorter loop of Henle and lack a vasa recta.
-
Juxtamedullary nephrons have a longer loop of Henle and have a vasa recta.
-
The vasa recta plays a role in maintaining the concentration gradient in the medulla.
-
The counter-current mechanism is more effective in juxtamedullary nephrons due to their longer loop of Henle. ### Countercurrent Mechanism
-
The countercurrent mechanism is a process that occurs in the juxtamedullary nephrons of mammals.
-
All mammals have the ability to form concentrated urine.
-
The loop of Henle, vasa recta, medullary interstitium, and collecting duct all contribute to the countercurrent mechanism.
-
The loop of Henle is a U-shaped tube with descending and ascending limbs.
-
Fluid flows in opposite directions in the descending and ascending limbs of the loop of Henle, creating a "countercurrent" flow.
-
The vasa recta, a network of capillaries that surrounds the loop of Henle, also exhibits countercurrent flow.
-
The vasa recta and loop of Henle are located in the medulla of the kidney.
-
The ascending limb of the loop of Henle is permeable to salts but not water.
-
The vasa recta and the loop of Henle are located in close proximity, which facilitates the countercurrent mechanism.
-
Countercurrent flow helps to maintain an increased osmolarity toward the inner medullary interstitium.
-
The osmolarity increases from 300 mOsmol/L in the cortex to 1200 mOsmol/L in the inner medulla.
-
Solutes move from high to low concentration.
-
The countercurrent system prevents solutes from diffusing back into the ascending limb, maintaining the high osmolarity in the medulla.
-
The high osmolarity in the medulla facilitates the reabsorption of water from the collecting tubule, which results in concentrated urine.
-
The collecting duct is permeable both to solutes and water.
-
The countercurrent system helps to conserve water in the body.
-
The countercurrent mechanism plays a crucial role in the formation of concentrated urine.
-
As the filtrate moves through the collecting tubule, water is drawn out into the medullary interstitium due to the high osmolarity, resulting in concentrated urine.
-
The osmolarity of the filtrate entering the proximal convoluted tubule is 300 mOsmol/L, and the osmolarity of the urine leaving the collecting duct is 1200 mOsmol/L.
-
The osmolarity of the final urine is four times more concentrated than the initial filtrate.
-
Sodium ions (Na+) and urea are crucial for maintaining the concentration gradient in the medulla.
Regulation of Kidney Function
- Kidney function is regulated through a hormonal feedback mechanism involving:
- Hypothalamus
- Juxtaglomerular apparatus (JGA)
- Heart
Hormonal Regulation by Hypothalamus
- The hypothalamus is activated when there is a change in blood volume, body fluid volume, or ionic concentration.
- Osmoreceptors in the body are activated when there is a change in fluid volume.
- Osmoreceptors send signals to the hypothalamus.
- The hypothalamus releases antidiuretic hormone (ADH), also known as vasopressin.
- ADH is released from the posterior pituitary gland.
- ADH acts on the distal convoluted tubule and collecting tubule, promoting water reabsorption.
- Water reabsorption increases blood volume, which increases blood pressure.
- This increase in blood pressure inhibits ADH release, creating a negative feedback loop.
ADH (Antidiuretic Hormone)
- ADH promotes water reabsorption from the distal convoluted tubule and collecting tubule.
- ADH increases the permeability of the collecting duct to water, allowing more water to move back into the blood.
- ADH is an antidiuretic hormone, meaning it reduces urine output.
- The reabsorption of water facilitated by ADH is known as facilitated reabsorption.
Blood Pressure Regulation - Renin-Angiotensin-Aldosterone system (RAAS)
- Angiotensinogen is produced in the liver, it is initially inactive.
- Renin, released by JG cells in the juxtaglomerular apparatus in the kidneys, converts angiotensinogen into Angiotensin I.
- Angiotensin I is converted into Angiotensin II by Angiotensin Converting Enzyme (ACE), primarily found in the lungs.
- Angiotensin II functions as:
- Vasoconstrictor: It directly constricts blood vessels, increasing blood pressure.
- Stimulator of Aldosterone: Angiotensin II acts on the adrenal cortex, stimulating aldosterone release.
- Stimulator of ADH: Angiotensin II can also stimulate the release of ADH, which further increases water reabsorption.
- Aldosterone, secreted by the adrenal cortex, increases the reabsorption of sodium ions in the DCT, leading to increased water reabsorption and increased blood volume.
- This increase in blood volume ultimately increases blood pressure and then increases glomerular filtration rate (GFR).
- The RAAS system is primarily a corrective mechanism: It activates when the body's blood volume decreases, blood pressure decreases, or GFR decreases in order to restore homeostasis.
Antagonism to RAAS
- Atrial Natriuretic Factor (ANF), secreted by the heart's atria, acts as an antagonist to the RAAS system:
- Vasodilation: ANF causes dilation of blood vessels, thereby reducing blood pressure.
- Increased GFR: It also increases GFR, allowing more water and sodium to be excreted in urine.
- Ultimately, ANF reduces blood pressure and blood volume, acting as a counter-regulatory mechanism to RAAS and facilitating the excretion of excess water and sodium.
Micturition (Urination):
- Micturition is the process of expelling urine from the urinary bladder.
- Urinary bladder: A pear-shaped, muscular organ that stores urine and expels it.
- Ureters: Tubes that carry urine from the kidneys to the urinary bladder.
- Urethra: The tube that carries urine from the bladder to the outside of the body.
- Urinary bladder wall: Contains smooth muscle (detrusor muscle), connective tissue, and epithelial lining.
- Internal and external urethral sphincters: Control urine flow. The internal sphincter is involuntary, and the external sphincter is voluntary.
- Stretch receptors: Located in the urinary bladder wall, they detect bladder distension.
- When urine accumulates: The bladder stretches and the stretch receptors send signals to the spinal cord via sensory nerves.
- The spinal cord relays these signals to the brain: The brain then sends signals back to the bladder via motor nerves, triggering the detrusor muscle to contract and the internal urethral sphincter to relax.
- This contraction: increases pressure in the bladder, forcing urine out through the open urethra.
- Voluntary control: The external urethral sphincter allows for voluntary control of urination.
- Normally, micturition is a reflex: Controlled by the spinal cord and the brain.
Key Points:
- RAAS: Renin-Angiotensin-Aldosterone system.
- JG cells: Juxtaglomerular cells, located in the kidneys.
- DCT: Distal convoluted tubule, part of the nephron.
- ACE: Angiotensin-converting enzyme.
- ANP: Atrial natriuretic peptide.
- GFR: Glomerular filtration rate.
- Micturition: Process of urination.
- Detrusor muscle: Smooth muscle in the bladder wall.
- Internal urethral sphincter: Involuntary.
- External urethral sphincter: Voluntary. ### The Excretory System
- The excretory system removes waste products from the body.
- The excretory system is responsible for maintaining a stable internal environment and helps in removing urea, excess salts, and water from the body.
- The excretory system includes the kidneys, ureters, urinary bladder, and urethra.
- The kidneys are the primary organs of the excretory system.
- The kidneys filter blood and produce urine.
- Kidneys are bean-shaped organs located on either side of the vertebral column.
- The kidneys have three distinct regions: the cortex, the medulla, and the pelvis.
- The cortex is the outer region of the kidney, the medulla is the inner region, and the pelvis is the innermost region.
- The functional unit of the kidney is the nephron.
- Each kidney has about one million nephrons.
- The nephron consists of a glomerulus, Bowman’s capsule, proximal convoluted tubule, Henle’s loop, distal convoluted tubule, and collecting duct.
- The glomerulus is a cluster of capillaries that filter blood.
- Bowman’s capsule surrounds the glomerulus and collects the filtered fluid.
- The proximal convoluted tubule reabsorbs water, glucose, amino acids, and other nutrients.
- Henle’s loop establishes a concentration gradient in the medulla, allowing for the reabsorption of water.
- The distal convoluted tubule regulates the balance of ions like sodium and potassium.
- The collecting duct carries urine to the renal pelvis.
- The nephron is responsible for filtering blood, reabsorbing nutrients, and excreting waste products.
The Mechanism of Urine Formation
- Urine formation involves three main processes: glomerular filtration, tubular reabsorption, and tubular secretion.
- Glomerular filtration is the process in which blood is filtered in the glomerulus, where water, glucose, amino acids, and other small molecules pass into Bowman's capsule, while blood cells and large proteins remain in the blood.
- Tubular reabsorption is the process in which essential substances like glucose, amino acids, water, and salts are reabsorbed back into the blood from the tubular fluid.
- Tubular secretion is the process in which waste products like urea, creatinine, and certain drugs are actively transported from the blood into the tubular fluid.
- The final product of urine formation is urine, which contains waste products and excess water.
The Micturition Reflex
- The micturition reflex is the process of urination.
- When the urinary bladder fills with urine, stretch receptors in the bladder wall are activated.
- The stretch receptors send sensory signals to the CNS.
- The CNS sends motor signals back to the urinary bladder, causing the smooth muscles of the bladder wall to contract.
- The internal sphincter of the urethra relaxes, allowing urine to flow out of the bladder.
- The external sphincter, which is under voluntary control, can also relax to allow for urination.
Properties of Urine
- Urine is typically transparent and light yellow.
- It has a characteristic pungent odor.
- Urine is hypertonic in nature, meaning it has a higher concentration of solutes compared to blood.
- The pH of urine is slightly acidic, around 6.
- Urine mainly composed of water (90-92%), followed by urea.
- The average daily output of urine is 1 to 1.5 litres.
- The average daily output of urea is 25 to 30 grams.
Abnormal Urine Composition
- Glycosuria: Presence of glucose in urine, often observed in diabetes mellitus.
- Ketonuria: Presence of ketone bodies in urine, also seen in diabetes mellitus.
- Uremia: Excess urea in urine and blood, indicating kidney failure.
- Albuminuria: Presence of albumin in urine, often indicative of glomerulonephritis.
- Hematuria: Presence of blood in urine, which may be due to various conditions.
- Anuria: Complete or almost complete absence of urine production.
- Dysuria: Painful or difficult urination.
Other Organs Involved in Excretion
- Lungs: Excrete carbon dioxide (around 200mL per minute) and water.
- Liver: Produces bile, which contains bilirubin, biliverdin, cholesterol, degraded hormones, steroids, vitamins, and drugs. These substances are passed into the intestines and excreted with feces.
- Skin: Sweat glands produce sweat, which contains water, urea, and lactic acid. Sweat helps in thermoregulation and excretion of waste products. Sebaceous glands secrete sebum, an oily substance containing steroids, hydrocarbons, and waxes, which provides a protective layer for the skin.
Disorders of the Excretory System
- Kidney failure: When kidney function is impaired, leading to accumulation of waste products in the blood, a condition known as uremia. It can cause severe health problems and need dialysis or kidney transplantation.
- Renal calculi (Kidney stones): Solid masses formed in the kidneys composed of insoluble salts like oxalates. They can block the urinary tract causing pain and discomfort.
- Glomerulonephritis: Inflammation of the glomeruli, often caused by bacterial or viral infections, leading to protein leakage in urine and potential for kidney failure.
Hemodialysis (Artificial Kidney)
- Hemodialysis is a treatment for kidney failure, which involves filtering blood to remove excess waste products and fluids.
- A hemodialysis machine contains a dialyzer, which is a container filled with a dialysis fluid.
- The dialysis fluid has a similar composition to blood plasma, but lacks urea.
- The patient's blood passes through a semipermeable membrane in the dialyzer, allowing urea and other waste products to diffuse from the blood into the dialysis fluid.
- The filtered blood is then returned to the patient's body.
- Hemodialysis is a temporary measure and requires frequent sessions.
- Long-term management of kidney failure may require a kidney transplant.
Kidney Transplantation
- Kidney transplantation involves replacing a failing kidney with a healthy one from a donor.
- The donor can be a living relative (allograft) or a deceased person (allograft).
- The best option is an identical twin (isograft) where immune rejection risk is minimal.
- Prior to transplantation, blood group compatibility and Human Leukocyte Antigen (HLA) matching are crucial to minimize rejection.
- HLA matching ensures similarity between donor and recipient organs.
Rejection of Kidney Transplants
- The body's immune system can reject a transplanted kidney.
- Rejection is a risk for both allografts and xenografts.
- Rejection is largely mediated by cell-mediated immunity with T-cells playing a key role.
Conclusion
The excretory system plays a crucial role in maintaining homeostasis and eliminating waste products from the body. Understanding its anatomy and functions is important for comprehending health and diseases related to this system, especially kidney failure and its management.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.