Podcast
Questions and Answers
What is the primary role of the trophozoite form of Entamoeba histolytica?
What is the primary role of the trophozoite form of Entamoeba histolytica?
- To reproduce in water
- To remain non-pathogenic
- To invade intestinal tissues (correct)
- To undergo encystation
Which form of Entamoeba histolytica is characterized as small, spherical, and non-feeding?
Which form of Entamoeba histolytica is characterized as small, spherical, and non-feeding?
- Precystic (correct)
- Cyst
- Binucleate
- Trophozoite
What happens to the precystic form of Entamoeba histolytica under conditions of compromised immunity?
What happens to the precystic form of Entamoeba histolytica under conditions of compromised immunity?
- It remains non-pathogenic
- It undergoes division into smaller forms
- It forms a thicker cyst wall
- It becomes motile and pathogenic (correct)
Which of the following is NOT a characteristic of the cystic form of Entamoeba histolytica?
Which of the following is NOT a characteristic of the cystic form of Entamoeba histolytica?
How does Entamoeba histolytica typically enter the human body?
How does Entamoeba histolytica typically enter the human body?
In its cystic form, how many nuclei can a mature cyst of Entamoeba histolytica contain?
In its cystic form, how many nuclei can a mature cyst of Entamoeba histolytica contain?
What is the diameter range of the trophozoite form of Entamoeba histolytica?
What is the diameter range of the trophozoite form of Entamoeba histolytica?
What role do food handlers play in the transmission of Entamoeba histolytica?
What role do food handlers play in the transmission of Entamoeba histolytica?
What is the primary method by which trophozoites invade the intestinal wall?
What is the primary method by which trophozoites invade the intestinal wall?
What triggers the excystation of cysts in the host's small intestine?
What triggers the excystation of cysts in the host's small intestine?
What leads to the formation of flask-shaped ulcers in the intestine?
What leads to the formation of flask-shaped ulcers in the intestine?
How do houseflies and cockroaches contribute to the spread of infection?
How do houseflies and cockroaches contribute to the spread of infection?
What is the outcome when trophozoites do not invade the host tissues?
What is the outcome when trophozoites do not invade the host tissues?
What characterizes the stool of a person with amoebic dysentery?
What characterizes the stool of a person with amoebic dysentery?
What facilitates the penetration of trophozoites into the sub-mucosa?
What facilitates the penetration of trophozoites into the sub-mucosa?
What happens to the cysts once they are ingested by a new host?
What happens to the cysts once they are ingested by a new host?
What is the primary symptom of amoebic dysentery?
What is the primary symptom of amoebic dysentery?
Which organ is NOT typically affected by trophozoites in amoebic dysentery?
Which organ is NOT typically affected by trophozoites in amoebic dysentery?
What diagnostic method is used to identify Entamoeba histolytica?
What diagnostic method is used to identify Entamoeba histolytica?
Which of the following is a common preventive measure for amoebic dysentery?
Which of the following is a common preventive measure for amoebic dysentery?
What symptom indicates the presence of abscesses in the liver caused by amoebic dysentery?
What symptom indicates the presence of abscesses in the liver caused by amoebic dysentery?
What is the recommended treatment for temporary relief of amoebic dysentery?
What is the recommended treatment for temporary relief of amoebic dysentery?
What type of sanitation efforts are municipalities responsible for to prevent amoebic dysentery?
What type of sanitation efforts are municipalities responsible for to prevent amoebic dysentery?
What is the significance of Charcot-Leyden crystals in stool analysis?
What is the significance of Charcot-Leyden crystals in stool analysis?
Flashcards are hidden until you start studying
Study Notes
Morphology
- Entamoeba histolytica has three forms: trophozoite, precystic, and cyst.
- Trophozoite: Active and motile form, measuring 20-30μ in diameter, characterized by a thin plasmalemma and a structured cytoplasm (ectoplasm and endoplasm).
- Precystic form: Smaller (12-15μ), non-motile, non-feeding, resembles trophozoite without food vacuoles, can become pathogenic if host immunity is compromised.
- Cysts: Rounded and encased in a resistant wall, measuring 10-20μ in diameter. Contains glycogen masses and chromatoid bodies. Nucleus divides from uninucleate to tetranucleate.
Transmission, Excystation, and Metacystic Development
- Infection occurs via ingestion of contaminated food or water containing tetranucleate cysts.
- Infected food handlers and feces in open areas contribute to contamination.
- Houseflies and cockroaches can transfer cysts to uncovered food.
- Cysts survive gastric juices and undergo excystation in the small intestine after 5-6 hours, releasing tetranucleate amoeba (metacyst).
- Metacysts divide by binary fission to form 8 small uninucleate amoebulae, which can invade intestinal tissue or undergo encystation.
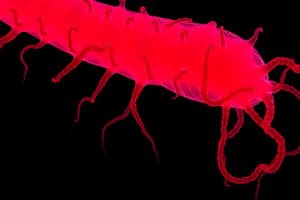
Clinical Features and Pathogenesis
- E. histolytica resides harmlessly in the large intestine but can become pathogenic if gut resistance decreases.
- Pathogenic magna forms invade the intestinal wall, creating flask-shaped ulcers filled with debris, lymphocytes, blood, and bacteria.
- Tissue erosion occurs through histolysis and cytolysis caused by trophozoite-secreted proteolytic enzymes (histolysin).
- Ruptured ulcers lead to blood and debris entering the intestinal lumen, causing amoebic dysentery characterized by acidic, foul-smelling stools mixed with blood.
- Trophozoites can spread to other organs, leading to abscess formation and conditions like amoebic hepatitis, which can result in fatal complications.
Laboratory Diagnosis
- Diagnosis of amoebiasis relies on microscopic examination of cysts in stool, trophozoites in fresh stool, or tissue.
- Detection of antibodies against E. histolytica in blood can be performed using enzyme-linked immunosorbent assay (ELISA).
- Presence of "Charcot-Leyden" crystals in stool suggests E. histolytica infection.
Prevention (Prophylaxis) and Treatment
- Prevention: Hygiene practices are essential, including handwashing, food protection from pests, avoiding open defecation, and ensuring safe water supply.
- Municipal hygiene efforts include monitoring food handlers, covering food articles, treating human waste, and maintaining sanitation.
- Treatment: Emetine is effective for temporary relief of amoebic dysentery. Dehydroemetine, a synthetic derivative, can also be used for treatment, though achieving permanent cure may require ongoing management due to potential relapses.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.