Podcast
Questions and Answers
Which of the following best describes the typical location of the thyroid gland in mammals?
Which of the following best describes the typical location of the thyroid gland in mammals?
- Cranial to the trachea at the level of the fifth tracheal ring.
- Caudal to the trachea at the level of the first or second tracheal ring. (correct)
- Ventral to the larynx near the hyoid apparatus.
- Dorsal to the esophagus near the thoracic inlet.
What structural feature characterizes the microanatomy of the thyroid gland?
What structural feature characterizes the microanatomy of the thyroid gland?
- Interspersed islands of endocrine cells within connective tissue.
- Cuboidal cells arranged around a central lumen filled with colloid.
- Clusters of lymphocytes surrounding blood vessels.
- Numerous sac-like structures called thyroid follicles. (correct)
What is the primary component of the colloid found within thyroid follicles?
What is the primary component of the colloid found within thyroid follicles?
- A suspension of calcium phosphate crystals.
- A dilute solution of electrolytes.
- A viscous liquid rich in protein. (correct)
- A gel matrix containing glycosaminoglycans.
Which cells secrete calcitonin?
Which cells secrete calcitonin?
What is the primary regulator of calcitonin secretion?
What is the primary regulator of calcitonin secretion?
Which molecule is the precursor for T3 and T4 synthesis in the thyroid gland?
Which molecule is the precursor for T3 and T4 synthesis in the thyroid gland?
In thyroid hormone synthesis, iodide is transported into the thyroid follicle cells via which mechanism?
In thyroid hormone synthesis, iodide is transported into the thyroid follicle cells via which mechanism?
What is the role of thyroid peroxidase in thyroid hormone synthesis?
What is the role of thyroid peroxidase in thyroid hormone synthesis?
What is the product of combining one molecule of MIT (monoiodotyrosine) with one molecule of DIT (diiodotyrosine)?
What is the product of combining one molecule of MIT (monoiodotyrosine) with one molecule of DIT (diiodotyrosine)?
How are T3 and T4 stored within the thyroid gland?
How are T3 and T4 stored within the thyroid gland?
Which of the following stimulates the secretion of thyroid hormones?
Which of the following stimulates the secretion of thyroid hormones?
How are T3 and T4 transported in the blood?
How are T3 and T4 transported in the blood?
Once T4 enters a target cell, what typically happens to it?
Once T4 enters a target cell, what typically happens to it?
How are thyroid hormones cleared from the plasma?
How are thyroid hormones cleared from the plasma?
What is the primary action of thyroid hormones on cellular metabolism?
What is the primary action of thyroid hormones on cellular metabolism?
How do thyroid hormones affect the basal metabolic rate (BMR) of cells?
How do thyroid hormones affect the basal metabolic rate (BMR) of cells?
What effect do thyroid hormones have on carbohydrate metabolism?
What effect do thyroid hormones have on carbohydrate metabolism?
What condition can hyperthyroidism cause?
What condition can hyperthyroidism cause?
Which clinical sign would be associated with hypothyroidism?
Which clinical sign would be associated with hypothyroidism?
What is a goiter?
What is a goiter?
Which of the following is a primary cause of hypothyroidism in dogs?
Which of the following is a primary cause of hypothyroidism in dogs?
Which of the following is an example of a goitrogen?
Which of the following is an example of a goitrogen?
What is the most common endocrinopathy of cats?
What is the most common endocrinopathy of cats?
What are the key hormones for regulating cellular metabolism that are controlled by the thyroid?
What are the key hormones for regulating cellular metabolism that are controlled by the thyroid?
What is the role of thyroglobulin (Tg) within the thyroid gland?
What is the role of thyroglobulin (Tg) within the thyroid gland?
Which condition results from iodine dificiency in cattle?
Which condition results from iodine dificiency in cattle?
A deficiency in iodine leads to:
A deficiency in iodine leads to:
When thyroid hormone levels are high in the blood, what happens to TRH secretion?
When thyroid hormone levels are high in the blood, what happens to TRH secretion?
What is the main function of HPT axis?
What is the main function of HPT axis?
A cat presents with significant weight loss despite an increased appetite, along with hyperactivity and a slightly elevated heart rate. Which condition is most likely?
A cat presents with significant weight loss despite an increased appetite, along with hyperactivity and a slightly elevated heart rate. Which condition is most likely?
A dog that has been undergoing glucocorticoid treatment tests for hypothyroidism via a blood test. Should the test results be considered reliable?
A dog that has been undergoing glucocorticoid treatment tests for hypothyroidism via a blood test. Should the test results be considered reliable?
A dairy farmer reports that several newborn calves in their herd are born hairless and weak, with some being stillborn. Which nutritional deficiency is most likely the cause?
A dairy farmer reports that several newborn calves in their herd are born hairless and weak, with some being stillborn. Which nutritional deficiency is most likely the cause?
Which of the following adjustments would occur to maintain normal thyroid hormone levels during pregnancy, given the increased catabolism of T4 and T3?
Which of the following adjustments would occur to maintain normal thyroid hormone levels during pregnancy, given the increased catabolism of T4 and T3?
How does the action of thyroid hormones on beta adrenergic receptors in cardiac tissue influence cardiac output?
How does the action of thyroid hormones on beta adrenergic receptors in cardiac tissue influence cardiac output?
Under conditions of severe iodine deficiency, why does the hyperplastic thyroid gland eventually fail to compensate for adequate thyroid hormone production?
Under conditions of severe iodine deficiency, why does the hyperplastic thyroid gland eventually fail to compensate for adequate thyroid hormone production?
A researcher is studying the expression of specific genes in response to thyroid hormone stimulation in cultured hepatocytes. They observe that some genes are upregulated rapidly, while others show a delayed response. Which mechanism best explains the observed difference in timing?
A researcher is studying the expression of specific genes in response to thyroid hormone stimulation in cultured hepatocytes. They observe that some genes are upregulated rapidly, while others show a delayed response. Which mechanism best explains the observed difference in timing?
Flashcards
Thyroid Glands
Thyroid Glands
Glands located caudally to the trachea, shaped like a butterfly.
Thyroid Follicles
Thyroid Follicles
Structures composed of follicular epithelial cells that synthesize thyroid hormones.
Colloid (Thyroid)
Colloid (Thyroid)
A viscous, protein-rich liquid filling thyroid follicles, containing thyroglobulin where thyroid hormones are stored.
Parafollicular Cells (C-cells)
Parafollicular Cells (C-cells)
Signup and view all the flashcards
Calcitonin
Calcitonin
Signup and view all the flashcards
HPT Axis
HPT Axis
Signup and view all the flashcards
TRH (Thyrotropin-Releasing Hormone)
TRH (Thyrotropin-Releasing Hormone)
Signup and view all the flashcards
TSH (Thyroid-Stimulating Hormone)
TSH (Thyroid-Stimulating Hormone)
Signup and view all the flashcards
Tyrosine
Tyrosine
Signup and view all the flashcards
Thyroglobulin (TG)
Thyroglobulin (TG)
Signup and view all the flashcards
Iodide Transport
Iodide Transport
Signup and view all the flashcards
Thyroglobulin Storage
Thyroglobulin Storage
Signup and view all the flashcards
Thyroid Peroxidase
Thyroid Peroxidase
Signup and view all the flashcards
Iodine Organification
Iodine Organification
Signup and view all the flashcards
Hormone coupling
Hormone coupling
Signup and view all the flashcards
T3/T4 secretetion
T3/T4 secretetion
Signup and view all the flashcards
Thyroid Hormone Transportation
Thyroid Hormone Transportation
Signup and view all the flashcards
Hormone Conjugation
Hormone Conjugation
Signup and view all the flashcards
Hormone metabolism
Hormone metabolism
Signup and view all the flashcards
Carbohydrate & Fat metablolism
Carbohydrate & Fat metablolism
Signup and view all the flashcards
Hyperthyroidism
Hyperthyroidism
Signup and view all the flashcards
Hypothyroidism
Hypothyroidism
Signup and view all the flashcards
Goiter
Goiter
Signup and view all the flashcards
T4
T4
Signup and view all the flashcards
T3
T3
Signup and view all the flashcards
Study Notes
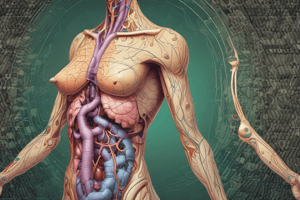
Endocrine - Thyroid
- The presentation covers the cellular biology and homeostasis of the endocrine system, specifically focusing on the thyroid gland.
- VP 2025 and Clara Camargo, DVM, Cert AqV are associated with this material.
Learning Objectives
- Locate the thyroid glands and briefly describe both its macro and microanatomy.
- Describe the regulation, synthesis, secretion, transport, and metabolic clearance of thyroid hormones.
- Describe the effects of the thyroid hormones on target tissues.
- Understand the symptoms of the main pathologies related to the thyroid hormones, including hyperthyroidism, hypothyroidism, and goiter.
Endocrine Glands
- Key endocrine glands include the hypothalamus, pineal gland, parathyroid, adenohypophysis, thyroid, pancreas, adrenal glands, ovaries, and testicles.
- The thyroid produces T3, T4, and calcitonin
Hormone Chemical Structure
- Amines are hormones derived from the modification of amino acids and are generally hydrophilic, except for thyroid hormones, which are hydrophobic.
- Thyroid hormones (T3 and T4) are derived from the amino acid tyrosine, as are catecholamines (dopamine, norepinephrine, epinephrine).
- The half-life of epinephrine is about 1 minute, while thyroxine (T4) has a half-life of 7-10 days.
- T3 and T4 require carrier proteins like thyroxine-binding globulin (TBG) and albumin for transport in the blood.
- Catecholamines bind to cell membrane receptors, whereas thyroid hormones bind to nuclear receptors.
Thyroid Gland Anatomy
- The thyroid gland is a butterfly-shaped gland located caudal to the trachea, typically at the level of the first or second tracheal ring in most mammals.
Thyroid Gland Microanatomy
- Thyroid tissue consists of numerous sac-like structures called thyroid follicles, which vary in size and have follicular epithelial cells arranged in a circular pattern that synthesize thyroid hormones.
Thyroid Gland Colloid
- The follicles are filled with colloid, a viscous liquid rich in protein (thyroglobulin, which is a glycoprotein) produced by the follicular epithelial cells.
- Thyroid hormones are stored in the colloid, which allows mammals to withstand periods of iodine deprivation without immediate effects on thyroid hormone production.
Thyroid Gland Parafollicular or C-Cells
- Parafollicular cells, or C-cells, are located outside the follicles, and secrete calcitonin, a peptide hormone involved in the regulation of calcium and phosphate metabolism.
- Calcitonin secretion is primarily regulated by blood calcium levels and is not directly controlled by the HP axis.
- When blood calcium levels are high, calcium sensors on the parafollicular cells trigger the release of calcitonin to help reduce calcium levels.
HPT Axis
- The hypothalamus responds to various stimuli, including cold weather, leptin (produced by adipose tissue during TAG gain), and lactation.
- The most important regulator of TRH secretion is thyroid hormone itself.
- Thyroid hormones also provide negative feedback directly on the adenohypophysis, causing reduced secretion of TSH.
- The concentration of T4 and T3 in blood and brain creates a negative feedback loop to the hypothalamus and anterior pituitary.
Thyroid Hormone Synthesis
- Tyrosine, a component of thyroglobulin.
- Iodine (I²) is essential.
- Thyroglobulin is synthesized within the follicle epithelial cells.
- Tyrosine combines with iodine to form thyroid hormones.
Thyroid Hormone Synthesis - Iodide
- Iodine (I²) comes from the diet and is converted to iodide (I-) in the intestinal tract before being transported to the thyroid follicle cells.
- Thyroid follicle cells trap iodide (I-) via a secondary active transport process using a Na+/I- cotransporter, where sodium provides the driving force to bring iodide into the cell.
- Intracellular iodide concentration is 25 – 200 times higher than outside the cell.
Thyroid Hormone Synthesis - Thyroid Peroxidase
- Oxidation of iodide to elemental iodine (l- → l²)
- Tyrosine iodination (Iodine combines to the tyrosine residue on thyroglobulin protein with the help of thyroid peroxidase)
- If 1 l² molecule attaches = MONOIODOTYROSINE (MIT)
- If 2 l² molecules attach = DIIODOTYROSINE (DIT)
Thyroid Hormone Synthesis - Fusion
- Fusion of two iodinated tyrosines
- 1 DIT + 1 DIT = T4 or Tetraiodothyronine or Thyronine or Thyroxine (4 iodine molecules)
- 1 MIT + 1 DIT = T3 or Triiodothyronine (3 iodine molecules)
Thyroid Hormone Storage
- T3 and T4 remain attached to thyroglobulin molecules and are stored in the colloid until secretion, offering a unique storage that allows the thyroid to maintain a large hormone reserve.
- T4 is preferentially produced by the thyroid follicle cells when iodine is sufficient; normally, the thyroid hormone is synthesized at a ratio of 4:1 (T4/T3)
- During iodine deficiency, the ratio may shift to 1:3 (T4/T3).
- A major source of T3 is peripheral deiodination of T4 in target tissues via enzyme-dependent deiodinases.
Thyroid Hormone Secretion
- TSH, secreted by the anterior pituitary, stimulates the secretion of thyroid hormones.
- Iodinated thyroglobulin is endocytosed back into the follicular epithelial cells and undergoes proteolysis, liberating both T4 and T3.
- Lysosomes fuse to thyroglobulin vesicles, leading to enzymes cleaving T3 and T4.
- Iodine atoms on iodinated tyrosine residues of thyroglobulin are efficiently recycled within the follicle cell to iodinate new thyroglobulin molecules.
- T3 & T4 freely pass through the thyroid follicle cell membrane into the surrounding capillaries due to their lipophilic nature.
Thyroid Hormone Transport
- Thyroid hormones are transported in the blood plasma attached to proteins, specifically thyroxine-binding globulin (TBG) and albumin, both synthesized in the liver.
- Only a small amount of hormone is free in the blood plasma.
- Free T4 and T3 are available to diffuse into the target cells
- Once free T4 enters the target cell, most of it is converted to T3 by iodothyronine deiodinases in the target cell cytosol.
- Reverse T3 (rT3) can be formed depending on the position of iodine; this is an inactive form of the hormone produced in high amounts in peripheral tissues during disease states.
Thyroid Hormone Transport - Equilibrium
- The equilibrium between free and bound hormone in the blood plasma is shifted by physiological, pharmacological, or pathological conditions such as catabolism during pregnancy and the use of certain drugs.
- Adjustments to maintain a normal amount of free hormone occur rapidly with declines in the rate of metabolism or stimulation of thyroid hormone secretion through the release of TSH.
- Reference values of free T4 and T3 vary for different species.
Hormone Clearance
- T4 and T3 hormones are cleared from the plasma through conjugation (formation of sulfates and glucuronides, mainly in the liver) and deiodination (metabolic breakdown by tissues, mainly in the liver, skeletal muscle, and kidneys).
- Conjugation involves the formation of sulfates and glucuronides majorly in the liver.
- Metabolites are excreted via the liver into bile (subsequently in feces) or via the kidney into the urine.
- A decreased metabolic clearance rate can lead to an excessively high concentration of thyroid hormones in the blood, potentially causing symptoms of hyperthyroidism, such as in liver disease.
Thyroid Hormone Actions
- They are primary factors for the control of cellular metabolism.
- Binds to nuclear receptors and initiate mRNA transcription.
- Important for the normal activity of all tissues.
- The mechanism of action is not fully understood but is being investigated through pathological conditions (hypo or hyperthyroidism).
Thyroid Hormone cellular actions
- There is an increase in the quantity of mitochondria and rate of synthesis.
- BMR is the minimal rate of energy expenditure per unit time at rest.
- Cellular enzymes increase activity in response to thyroid hormones.
- There is an increase in O2 consumption and heat production.
- Weight loss in hyperthyroidism, weight gain in hypothyroidism
Actions of thyroid hormones - metabolism
- There is an increase in absorption of glucose
- Facilitates the movement of glucose into fat and muscle tissues
- Increases lypolysis and mobilises fat, for fatty acids to become available for B-oxidation.
- Stimulates a reduction in plasma cholesterol and liver fat.
- Can cause hyperlipidemia
Thyroid Hormone Action
- Thyroid hormones affect gastrointestinal (GI) functions, increasing appetite, food intake, and GI motility; hyperthyroidism can cause diarrhea due to hypermotility.
- Skin integrity is maintained by thyroid hormones.
- Hypothyroid animals often exhibit hair loss, changes in skin and hair color, and are predisposed to developing skin infections.
Action of thyroid hormones - Growth
- Influence occurs through the nervous system (CNS). Reduced quantities may reduced mental abilities and lethargy in animals.
- GH can lead to dwarfism through hypothyroidism.
- Increase blood flow and cardiac output through the use of catecholamines.
- Increases the numbers of beta adrenergic receptors on a heart
- Improves heart rate and heart excitability.
- Can induce metamorphosis in amphibians and fish larvae.
Thyroid Pathologies
- Hyperthyroidism is most common in cats and is caused by hyperplasia or tumors (adenomas) of the thyroid gland, typically affecting middle-aged to older cats.
- It is characterized by autonomous growth of thyroid follicles due to abnormalities in the signal transduction of the thyroid cell.
- Hypermetabolism causes increased heart rates, weight loss, increased appetite (polyphagia), increased thirst/urination (polydipsia/polyuria), vomiting/diarrhea, shedding, unkempt appearance, and hyperactivity.
Thyroid Pathologies cont.
- Hypothyroidism is more common in dogs and causes a general reduction in metabolic rate, characterized by slow heart rate, decreased body temperature, infertility, weight gain, and slower mental ability.
Primary causes of hypothyroidism in dogs include:
- lymphocytic thyroiditis (inflammation).
- congenital thyroid dysgenesis (inherited defects in the hypothalamic-pituitary-thyroid axis).
- T4 transport defects.
- goitrogens.
- iodine deficiency.
- autoimmune thyroiditis. Secondary causes include:
- pituitary tumors.
- radiation therapy.
- glucocorticoids.
Hypothyroidism
- Lethargy and obesity
- Reproductive disorders
- Bradycardia
- Fatigue
- Cold intolerance
Iodine deficiency
- Caused by Inadequate dietary intake and consumption of feeds that cause intereferences with the thyroid gland (Goitrogens)
- Goitrogens are brassicas, white clover pastures.
- It is most prevalent in cattles sheep and goats
Iodine deficiency effects
- In severe cases the organ is unable to cope.
- Animals becaome inappetant, and display a slow heart rate
- Animals undergo reduces fertility and fetus' become hypothyroid.
- Enlargement of the thyroid
- Calves and lambds can be born hairelss and weak
Thyroid Diagnosis
- Total T4 and T3
- Free T4 and T3
- T3 suppression test
- Reverse T3
- Antibodies (T3 and T4, thyroglobulin)
- TRH and TSH
- Genetic test (TPO gene mutation)
- Drugs affecting the thyroid hormones
- Understanding these points help in diagnosis:
- Chemical structure of the hormones
- Synthesis and regulation
- How do they travel in the blood circulation
- Signal transduction
- Hormone clearance
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.