Podcast
Questions and Answers
In Type 1 Diabetes, what physiological process leads to diabetic ketoacidosis (DKA) when insulin is missed?
In Type 1 Diabetes, what physiological process leads to diabetic ketoacidosis (DKA) when insulin is missed?
- The body's shift to fat metabolism, leading to ketone production and acidosis. (correct)
- Increased glucose uptake by cells, causing cellular dehydration.
- The liver's inability to convert glycogen to glucose, causing an energy deficit.
- Excessive insulin production, resulting in hypoglycemia and subsequent acid build-up.
Which of the following assessment findings would lead you to suspect Hyperosmolar Hyperglycemic Nonketotic Syndrome (HHNS) in a patient?
Which of the following assessment findings would lead you to suspect Hyperosmolar Hyperglycemic Nonketotic Syndrome (HHNS) in a patient?
- Blood glucose of 50 mg/dL, diaphoresis, and tremors.
- Blood glucose of 700 mg/dL, severe dehydration, and altered mental status. (correct)
- Rapid onset of confusion, pale skin, and a history of skipping meals.
- Fruity-smelling breath, Kussmaul respirations, and blood glucose of 300 mg/dL.
A patient with a history of Type 1 Diabetes is found unresponsive. You suspect hypoglycemia. After administering IV glucose, the patient remains unresponsive. Which of the following is the MOST appropriate next step?
A patient with a history of Type 1 Diabetes is found unresponsive. You suspect hypoglycemia. After administering IV glucose, the patient remains unresponsive. Which of the following is the MOST appropriate next step?
- Prepare to administer IM glucagon, if available, to help raise blood sugar levels. (correct)
- Administer another dose of IV glucose, as a single dose is often insufficient.
- Apply a nasal cannula at 6LPM and reassess in 5 minutes.
- Begin immediate transport and contact medical control to consider other possible causes.
What is the underlying cause of hemophilia, leading to uncontrolled bleeding?
What is the underlying cause of hemophilia, leading to uncontrolled bleeding?
During the primary assessment of a patient with suspected hyperglycemia, what finding related to breathing would be MOST concerning and indicate the need for immediate intervention?
During the primary assessment of a patient with suspected hyperglycemia, what finding related to breathing would be MOST concerning and indicate the need for immediate intervention?
What is the primary treatment for a conscious patient experiencing hypoglycemia?
What is the primary treatment for a conscious patient experiencing hypoglycemia?
Why is minimizing movement a critical aspect of emergency care for a patient with hemophilia?
Why is minimizing movement a critical aspect of emergency care for a patient with hemophilia?
Which of the following is the MOST immediate risk associated with Deep Vein Thrombosis (DVT)?
Which of the following is the MOST immediate risk associated with Deep Vein Thrombosis (DVT)?
In assessing a patient with a suspected endocrine emergency, which question from the SAMPLE history is MOST relevant to ask?
In assessing a patient with a suspected endocrine emergency, which question from the SAMPLE history is MOST relevant to ask?
What is the primary function of insulin in regulating blood sugar levels?
What is the primary function of insulin in regulating blood sugar levels?
A patient presents with severe pain in their leg, recent surgery, and a history of smoking. What condition should you suspect?
A patient presents with severe pain in their leg, recent surgery, and a history of smoking. What condition should you suspect?
A patient with a known history of hemophilia is reporting internal bleeding. Besides rapid transport, what is the MOST important step?
A patient with a known history of hemophilia is reporting internal bleeding. Besides rapid transport, what is the MOST important step?
Which of the following is the correct classification of the pancreas?
Which of the following is the correct classification of the pancreas?
What is the primary cause of Type 2 Diabetes?
What is the primary cause of Type 2 Diabetes?
What is the first step in scene size-up and primary assessment?
What is the first step in scene size-up and primary assessment?
What are the symptoms of hypoglycemia?
What are the symptoms of hypoglycemia?
What SAMPLE question would be most pertinent in an endocrine emergency?
What SAMPLE question would be most pertinent in an endocrine emergency?
A patient presents with excessive thirst, hunger, and urination. What symptoms are they experiencing?
A patient presents with excessive thirst, hunger, and urination. What symptoms are they experiencing?
A patient presents with fruity-smelling breath and Kussmaul respirations. What treatment is needed immediately?
A patient presents with fruity-smelling breath and Kussmaul respirations. What treatment is needed immediately?
What is the inherited cause of Sickle Cell Anemia?
What is the inherited cause of Sickle Cell Anemia?
What is the treatment for Sickle Cell Crisis?
What is the treatment for Sickle Cell Crisis?
What is the primary risk of untreated kidney stones?
What is the primary risk of untreated kidney stones?
What should one check in a patient who is a dialysis patient?
What should one check in a patient who is a dialysis patient?
In the mnemonic DUMBELS (Diarrhea, Urination, Miosis, Bradycardia, Bronchospasm, Emesis, Lacrimation, Salivation), what does DUM stand for?
In the mnemonic DUMBELS (Diarrhea, Urination, Miosis, Bradycardia, Bronchospasm, Emesis, Lacrimation, Salivation), what does DUM stand for?
What does the OPQRST acronym stand for when it comes to medical assessment?
What does the OPQRST acronym stand for when it comes to medical assessment?
Flashcards
Endocrine System
Endocrine System
Controls body functions via hormones.
Pancreas
Pancreas
Regulates blood sugar by producing insulin and glucagon.
Insulin
Insulin
Lowers blood sugar and helps glucose enter cells.
Glucagon
Glucagon
Signup and view all the flashcards
Type 1 Diabetes
Type 1 Diabetes
Signup and view all the flashcards
Type 2 Diabetes
Type 2 Diabetes
Signup and view all the flashcards
Diabetic Ketoacidosis (DKA)
Diabetic Ketoacidosis (DKA)
Signup and view all the flashcards
HHNS
HHNS
Signup and view all the flashcards
Causes of Hyperglycemia
Causes of Hyperglycemia
Signup and view all the flashcards
Polyuria, Polydipsia, Polyphagia
Polyuria, Polydipsia, Polyphagia
Signup and view all the flashcards
Kussmaul Respirations
Kussmaul Respirations
Signup and view all the flashcards
DKA signs
DKA signs
Signup and view all the flashcards
HHNS signs
HHNS signs
Signup and view all the flashcards
Causes of Hypoglycemia
Causes of Hypoglycemia
Signup and view all the flashcards
Sickle Cell Disease
Sickle Cell Disease
Signup and view all the flashcards
Hemophilia
Hemophilia
Signup and view all the flashcards
Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis (DVT)
Signup and view all the flashcards
Pulmonary Embolism
Pulmonary Embolism
Signup and view all the flashcards
Toxicology
Toxicology
Signup and view all the flashcards
Poison
Poison
Signup and view all the flashcards
Toxin
Toxin
Signup and view all the flashcards
Inhalation
Inhalation
Signup and view all the flashcards
Absorption
Absorption
Signup and view all the flashcards
Ingestion
Ingestion
Signup and view all the flashcards
Injection
Injection
Signup and view all the flashcards
Study Notes
Endocrine System Overview
- The endocrine system regulates body functions via hormones.
- The pancreas regulates blood sugar by producing insulin and glucagon.
- Insulin lowers blood sugar and helps glucose enter cells.
- Glucagon raises blood sugar when it's low
Diabetes Mellitus
- Diabetes Mellitus is the name for a group of metabolic disorders in which the body does not produce enough insulin or use it effectively.
Type 1 Diabetes
- It’s an autoimmune disorder
- The body does not produce insulin and requires external insulin to survive.
- Often diagnosed in childhood.
- Complications include:
- Diabetic ketoacidosis (DKA) is a condition that can occur if insulin is missed.
- High blood sugar can lead to ketone production, resulting in acidosis.
Type 2 Diabetes
- Cells become resistant to insulin.
- Obesity and lifestyle factors are linked to Type 2.
- Treatments involve diet, exercise, oral medications, or insulin.
- A complication is Hyperosmolar Hyperglycemic Nonketotic Syndrome (HHNS).
Diabetic Emergencies
Hyperglycemia (High Blood Sugar)
- Causes of hyperglycemia include too much food and not enough insulin.
- Stress and infection can be a cause
- Poor medication compliance can be a factor
- Signs and Symptoms include:
- Gradual onset
- Excessive urination, thirst, hunger (polyuria, polydipsia, polyphagia)
- Warm, dry skin
- Fruity-smelling breath (DKA)
- Kussmaul respirations (deep, rapid breathing)
- Treatment usually includes fluids and insulin in a hospital setting, and supplemental oxygen if there is respiratory distress
Diabetic Ketoacidosis (DKA) - Type 1
- Blood glucose is usually > 400 mg/dL.
- Fat metabolism leads to ketone buildup, leading to metabolic acidosis.
- Signs include Kussmaul respirations, fruity breath, and altered mental status.
HHNS - Type 2
- Blood Glucose > 600 mg/dL
- Involves severe dehydration, confusion, and dark urine
- No ketones present
Hypoglycemia (Low Blood Sugar)
- Causes of hypoglycemia include too much insulin or medication.
- Skipping meals
- Increased exercise can cause it
- Signs & Symptoms include:
- Rapid onset
- Pale, sweaty skin
- Altered mental status, seizures, unconsciousness
- Tachycardia, dizziness
- Treatment includes:
- Oral glucose, if the person is conscious
- If unconscious, administer IV glucose or IM glucagon
- Rapid transport if unresponsive
Hematologic Emergencies
Sickle Cell Disease
- It’s an inherited disorder, mostly in African, Caribbean, South American populations.
- Misshapen RBCs block blood flow, causing painful crises.
- Complications include vaso-occlusive crises (severe pain), infections, stroke, or organ failure.
- Treatment includes:
- High-flow oxygen (12-15 L/min)
- Pain management (hospital)
- Fluids, transport
Hemophilia
- Due to a lack of clotting factors, leading to uncontrolled bleeding.
- It’s more common in males.
- Emergency Care:
- Be alert for internal bleeding.
- Minimize movement.
- Transport ASAP
Deep Vein Thrombosis (DVT)
- Blood clot in a deep vein (usually leg).
- Risk factors: Surgery, immobility, smoking, obesity.
- Major risk: Pulmonary embolism (clot travels to lungs).
- Treatment:
- Anticoagulants (hospital care)
- Preventive measures: Compression stockings, movement
Assessment & Management
- Scene Size Up: Check for insulin pumps, syringes
- Take standard precautions
- Primary Assessment:
- Airway & Breathing:
- Kussmaul respirations may indicate DKA
- Shallow, rapid breathing may indicate Hypoglycemia
- Circulation:
- Dry, warm skin → Hyperglycemia
- Pale, moist skin → Hypoglycemia
- Airway & Breathing:
- Secondary Assessment:
- Check blood glucose if available
- Look for medical alert bracelets
- Ask SAMPLE Questions, e.g., Do you take insulin or pills? Have you eaten today? Have you had any recent illness, stress, or unusual activity?
Emergency Treatment Overview
- Hypoglycemia: Rapid onset, sweating, confusion is treated with glucose.
- Hyperglycemia: Gradual onset, thirst, fruity breath requires transport.
- Sickle Cell: Pain crisis + oxygen needed.
- Hemophilia: Risk of severe bleeding needs transport ASAP.
- When in doubt, check blood sugar levels.
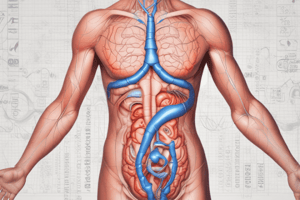
Overview of the Abdominal Systems
Major Organ Systems
- Gastrointestinal System: Digestion, absorption, and waste elimination.
- Urinary System: Filters waste, regulates fluid balance, and removes excess fluids.
- Reproductive System: Includes male and female reproductive organs.
Solid vs. Hollow Organs
- Solid Organs: Liver, spleen, pancreas, kidneys, ovaries; injury can cause shock and bleeding.
- Hollow Organs: Stomach, intestines, bladder, gallbladder; rupture can cause peritonitis (infection of abdominal cavity).
Gastrointestinal System & Emergencies
Key Components of the GI System
- Stomach: Breaks down food using gastric juices.
- Liver: Filters toxins, produces bile, stores glucose.
- Gallbladder: Stores and releases bile for fat digestion.
- Small Intestine: Absorbs nutrients (duodenum, jejunum, ileum).
- Large Intestine (Colon): Absorbs water, forms stool.
- Spleen: Stores blood, filters old RBCs (not part of digestion).
Common GI Conditions
Peritonitis
- Inflammation of the peritoneum (lining of the abdominal cavity).
- Causes: Blood, bile, pus, or bacteria leakage into the abdomen.
- Symptoms: Severe pain, distention, fever, nausea, vomiting.
Peptic Ulcer Disease (PUD)
- Erosion of stomach lining due to acid, NSAIDs, or H. pylori bacteria.
- Symptoms: Burning pain, nausea, vomiting, upper GI bleeding.
Gallstones & Cholecystitis
- Gallstones block bile duct, leading to gallbladder inflammation.
- Symptoms: RUQ pain, worse after fatty meals, nausea, vomiting.
Appendicitis
- Inflammation of the appendix, risk of rupture.
- Symptoms: RLQ pain, rebound tenderness, fever, nausea, vomiting.
Pancreatitis
- Inflammation of the pancreas, often due to alcohol or gallstones.
- Symptoms: LUQ pain radiating to back, nausea, vomiting, distention.
Diverticulitis
- Inflamed pockets in the colon due to trapped feces.
- Symptoms: LLQ pain, fever, chills, nausea, changes in bowel habits.
Gastrointestinal Bleeding
- Upper GI Bleed (Stomach/Esophagus) causes vomiting blood, black stools.
- Lower GI Bleed (Colon/Rectum) causes bright red blood in stool.
- Causes: Ulcers, esophageal varices, diverticulitis, cancer.
Esophageal Varices
- Swollen veins in esophagus (often from liver disease).
- Symptoms: Vomiting bright red blood, jaundice, shock signs.
Gastroenteritis
- Inflammation of stomach/intestines (viral or bacterial).
- Symptoms: Diarrhea, nausea, vomiting, fever, cramps.
Hernias
- Organ protrudes through abdominal wall.
- Strangulated hernias cut off blood flow, which is an emergency.
- Symptoms: Sudden pain, discoloration, non-reducible mass.
Urinary System & Emergencies
Key Components of the Urinary System
- Kidneys: Filter blood, regulate fluids.
- Ureters: Transport urine to bladder.
- Bladder: Stores urine.
- Urethra: Eliminates urine from body.
Common Urinary Conditions
Urinary Tract Infections (UTIs)
- Bladder infection due to bacteria.
- Symptoms: Painful urination, frequent urge, cloudy urine, fever, can progress to pyelonephritis (kidney infection) if untreated.
Kidney Stones
- Crystals form in kidney, blocking ureters.
- Symptoms: Severe flank pain, hematuria (blood in urine), nausea.
Acute & Chronic Kidney Failure
- Acute Kidney Failure: Sudden loss of function, reversible with treatment.
- Chronic Kidney Failure: Irreversible, requires dialysis or transplant.
- Symptoms: Edema, confusion, lethargy, ammonia breath odor.
EMS Assessment & Management
- Observe for trauma, environmental factors
- Airway & Breathing: Monitor for distress, vomiting.
- Circulation: Check for shock signs (tachycardia, hypotension, pale skin).
- Secondary Assessment:
- OPQRST: Onset, Provocation, Quality, Radiation, Severity, Time.
- SAMPLE History: Medications (NSAIDs?), alcohol use, prior conditions.
Palpate Abdomen: Quadrant pain can indicate specific conditions.
- RUQ: Gallbladder (Cholecystitis), Liver (Hepatitis)
- LUQ: Pancreatitis, Spleen Injury
- RLQ: Appendicitis
- LLQ: Diverticulitis
- Treatment & Transport:
- Shock Management: Oxygen, position of comfort, rapid transport.
- Pain Control: Avoid oral meds, allow hospital to manage.
- Dialysis Patients: Monitor AV fistula sites for bleeding.
Key Takeaways:
- Rapid assessment and transport are necessary.
- Abdominal pain with shock signs means emergency.
- Flank pain, hematuria = Kidney stones
- Black stools = Upper GI Bleed; Red blood = Lower GI Bleed
- Always consider peritonitis in severe abdominal pain! When in doubt, transport immediately!
Introduction to Toxicology
- Toxicology is the study of toxic or poisonous substances.
- A poison is any substance that can damage body structures or impair function.
- A toxin is a poisonous substance produced by bacteria, animals, or plants.
- Routes of Exposure:
- Inhalation (gases, fumes)
- Absorption (skin contact)
- Ingestion (swallowed)
- Injection (drugs, venom)
- EMS Role in Toxicology:
- Recognize poisoning symptoms.
- Identify the poison if possible.
- Contact Poison Control for guidance.
- Provide emergency care and transport.
Routes of Poison Exposure & Treatment
Inhaled Poisons
- Inhaled poisons include carbon monoxide, chlorine gas, and fumes.
- Symptoms include respiratory distress, dizziness, headache, and confusion.
- Remove patients from exposure.
- Provide high-flow oxygen and transport immediately.
Absorbed Poisons (Surface Contact)
- Absorbed poisons include industrial chemicals, plant toxins, and acids.
- Symptoms include skin irritation, burns, rashes, and systemic effects.
- Treatment includes:
- Remove clothing and brush off dry chemicals.
- Flush with water for 15-20 minutes.
- Avoid contaminating yourself.
Ingested Poisons
- Ingested poisons include: medications, household cleaners, food poisoning.
- Symptoms: Burns around mouth, vomiting, abdominal pain, and altered mental status.
- Treatment includes assessing ABCs, considering activated charcoal (if protocol allows), and transporting and notifying Poison Control.
Injected Poisons
- Include: Drug overdoses, insect/reptile venom.
- Symptoms include: Local swelling, pain, dizziness, weakness, and shock symptoms.
- Treatment: Monitor airway and breathing.
Specific Poisons & Overdoses
Carbon Monoxide (CO) Poisoning
- Colorless, odorless gas from fires, vehicle exhaust.
- Symptoms: Headache, dizziness, confusion, cherry-red skin (late sign).
- Treatment: High-flow oxygen, hyperbaric therapy (hospital setting).
Alcohol Intoxication & Withdrawal
- Effects: CNS depression, liver damage.
- Symptoms:
- Intoxication: Slurred speech, uncoordinated movements.
- Withdrawal: Delirium tremens (DTs) – hallucinations, seizures, and tremors.
- Treatment: Airway support, fluids, and transport.
Opioid Overdose (Heroin, Fentanyl, Morphine)
- Symptoms: Pinpoint pupils, respiratory depression, unconsciousness.
- Treatment: Administer Naloxone (Narcan) per protocol, airway support, and high-flow oxygen.
Sedative-Hypnotics (Benzodiazepines, Barbiturates)
- Examples: Valium, Xanax, Rohypnol.
- Symptoms: Drowsiness, confusion, and respiratory depression.
- Treatment: Airway support and transport.
Stimulants (Cocaine, Meth, Ecstasy)
- Symptoms: Increased heart rate, hypertension, paranoia, and seizures.
- Treatment: Keep patient calm, transport, and monitor vitals.
Hallucinogens (LSD, PCP, Mushrooms)
- Symptoms: Visual hallucinations, anxiety, paranoia.
- Treatment: Provide reassurance and minimize stimulation.
Cholinergic (Pesticides, Nerve Agents)
- Mnemonic: DUMBELS.
- Diarrhea
- Urination
- Miosis (pupil constriction)
- Bradycardia, bronchospasm
- Emesis (vomiting)
- Lacrimation (tears)
- Salivation, seizures
- Treatment: DuoDote Auto-Injector (Atropine + Pralidoxime) and oxygen with airway support.
Emergency Assessment & Management
- Scene Size-Up: Look for pill bottles, chemicals, and paraphernalia; ensure scene safety.
- Primary Assessment:
- ABCs: Airway, Breathing, Circulation.
- Provide oxygen and ventilation if needed.
- Secondary Assessment:
- Obtain SAMPLE history: What was taken? When and how much? Any treatments given?
- Look for track marks, burns, and pinpoint pupils.
- Treatment & Transport Considerations:
- Contact Poison Control for guidance.
- Manage symptoms, not just the poison.
- Transport for further evaluation.
Key Takeaways:
- Recognize poisoning early - Altered mental status is common!
- Assess route of exposure (inhalation, absorption, ingestion, injection).
- Use activated charcoal if indicated (not for acids, alkalis, or petroleum).
- Naloxone (Narcan) reverses opioid overdoses.
- Call Poison Control for all toxic exposures.
- When in doubt, provide oxygen and rapid transport!
Medical Emergencies
Introduction to Medical Emergencies
- Medical emergencies include illnesses or conditions caused by disease.
- Trauma emergencies include physical injuries.
- Some people experience both types of emergencies.
Types of Medical Emergencies:
- Respiratory Emergencies: Affect breathing and oxygen supply, e.g., asthma, COPD, pneumonia, pulmonary edema.
- Cardiovascular Emergencies: Affect the heart and circulation, e.g., heart attack, congestive heart failure, hypertension.
- Neurologic Emergencies: Affect the brain and nervous system, e.g., stroke, seizures, syncope.
- Gastrointestinal & Urologic Emergencies: Involve digestive and urinary systems, e.g., appendicitis, diverticulitis, pancreatitis, kidney stones.
- Endocrine Emergencies: Often related to diabetes complications, e.g., diabetic ketoacidosis (DKA), hypoglycemia.
- Hematologic Emergencies: Related to blood disorders, e.g., sickle cell disease, clotting disorders.
- Immunologic Emergencies: Involve allergic reactions and immune responses, e.g., anaphylaxis.
- Toxicologic Emergencies: Involve poisoning and substance abuse, e.g., drug overdose, chemical poisoning.
- Psychological & Behavioral Emergencies: Mental health-related crises, e.g., suicidal ideation, anxiety disorders.
- Gynecologic Emergencies: Conditions affecting female reproductive organs, e.g., ectopic pregnancy, pelvic inflammatory disease.
Patient Assessment Process:
- Scene Size-up:
- Ensure scene safety.
- Use standard precautions (PPE).
- Determine Nature of Illness (NOII).
- Primary Assessment:
- General Impression: Appearance, level of distress.
- Level of Consciousness: AVPU scale (Alert, Verbal, Pain, Unresponsive).
- Airway: Open and clear?
- Breathing: Rate, depth, effort.
- Circulation: Skin color, pulse, bleeding.
- History Taking (SAMPLE & OPQRST)
- SAMPLE History:
- Signs & Symptoms
- Allergies
- Medications
- Past Medical History
- Last Oral Intake
- Events Leading to Illness
- OPQRST for Pain Assessment:
- Onset
- Provocation
- Quality
- Radiation
- Severity
- Time
- Secondary Assessment
- Focused Exam for conscious patients.
- Head-to-Toe Exam for unconscious patients.
- Take Vital Signs:
- Pulse, Respirations, Blood Pressure
- Oxygen Saturation (Pulse Oximetry)
- Blood Glucose Level (if indicated)
- Reassessment:
- Monitor changes in patient condition.
- Check interventions (oxygen, medication, transport decisions).
Management & Transport Considerations:
- Transport Decision:
- Critical patients are a rapid transport.
- Consider closest appropriate facility.
- Mode of Transport:
- Ground Ambulance: EMTs and Paramedics.
- Air Transport: Critical Care Team for severe cases.
- Infectious Disease Precautions:
- Standard Personal Protective Equipment (PPE) (gloves, masks, eye protection).
- Special precautions for respiratory infections (N95 mask).
- Special Considerations:
- Patients with multiple conditions (heart disease + diabetes).
- Elderly patients may have vague or atypical symptoms.
- Pediatric patients require different assessments.
Infectious Diseases Overview
Common Infectious Diseases:
- Influenza: Viral respiratory illness.
- HIIV/AIDS: Bloodborne virus affecting immunity.
- Hepatitis: Liver infection (A, B, C types).
- Meningitis: Inflammation of the meninges (brain covering).
- Tuberculosis (TB): Chronic lung infection requiring N95 mask protection.
- MRSA: Antibiotic-resistant bacterial infection.
Epidemics & Pandemics:
- Epidemic: Local outbreak of disease.
- Pandemic: Global spread of an illness (e.g., COVID-19).
Travel-Related Infections:
- Always ask about recent travel history and to consider tropical diseases (malaria, Zika, Ebola).
Key Takeaways:
Medical emergencies vary widely; thorough assessment is key! SAMPLE and OPQRST help guide history-taking. Always prioritize Airway, Breathing, Circulation (ABCs). Use PPE for infection control (gloves, mask, eye protection). Rapid transport for unstable patients is critical. Be aware of emerging infectious diseases and global outbreaks. When in doubt, transport and reassess!
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.