Podcast
Questions and Answers
What is the primary action of levothyroxine?
What is the primary action of levothyroxine?
- Inhibits the synthesis of thyroid hormones
- Blocks the release of thyroid hormone
- Acts as an agonist at nuclear T3 receptors
- Acts as a precursor to active thyroid hormone T3 (correct)
Which of the following medications is NOT a thyroid hormone replacement therapy?
Which of the following medications is NOT a thyroid hormone replacement therapy?
- Levothyroxine
- Liotrix
- Liothyronine
- Methimazole (correct)
Which of the following drugs can increase levothyroxine metabolism?
Which of the following drugs can increase levothyroxine metabolism?
- Propylthiouracil
- Phenytoin (correct)
- Calcium carbonate
- Iron salts
Which of the following conditions is NOT an indication for thyroid hormone replacement therapy?
Which of the following conditions is NOT an indication for thyroid hormone replacement therapy?
What is the primary concern regarding the narrow therapeutic index of thyroid hormone drugs?
What is the primary concern regarding the narrow therapeutic index of thyroid hormone drugs?
What is the mechanism of action of propylthiouracil and methimazole?
What is the mechanism of action of propylthiouracil and methimazole?
Which of the following drugs is most likely to affect the pharmacodynamic effect of levothyroxine?
Which of the following drugs is most likely to affect the pharmacodynamic effect of levothyroxine?
Which of the following factors can inhibit the GI absorption of levothyroxine?
Which of the following factors can inhibit the GI absorption of levothyroxine?
What is the half-life of liothyronine (T3) in a euthyroid individual?
What is the half-life of liothyronine (T3) in a euthyroid individual?
Which of the following statements is TRUE regarding the use of thyroid hormone replacement therapy for pituitary TSH suppression?
Which of the following statements is TRUE regarding the use of thyroid hormone replacement therapy for pituitary TSH suppression?
Which of the following medications is MOST likely to increase the need for warfarin dose adjustment in a patient with hypothyroidism?
Which of the following medications is MOST likely to increase the need for warfarin dose adjustment in a patient with hypothyroidism?
Which of these is an example of a common side effect of thyroid hormone replacement therapy?
Which of these is an example of a common side effect of thyroid hormone replacement therapy?
Which of the following drugs can inhibit peripheral deiodinase, thereby impairing the activation of T4 to T3?
Which of the following drugs can inhibit peripheral deiodinase, thereby impairing the activation of T4 to T3?
What is the primary reason why changing thyroid hormone preparations is not recommended?
What is the primary reason why changing thyroid hormone preparations is not recommended?
Which of the following drugs is primarily used to treat hyperthyroidism?
Which of the following drugs is primarily used to treat hyperthyroidism?
What is the primary mechanism of action of Iodides (KI, NaI) in the treatment of hyperthyroidism?
What is the primary mechanism of action of Iodides (KI, NaI) in the treatment of hyperthyroidism?
What is the primary hormone synthesized by the thyroid gland that is crucial for regulating metabolism?
What is the primary hormone synthesized by the thyroid gland that is crucial for regulating metabolism?
Which medication is commonly used to treat hyperthyroidism by inhibiting the thyroid's hormone production?
Which medication is commonly used to treat hyperthyroidism by inhibiting the thyroid's hormone production?
What is the mechanism of action for propranolol when used in the context of thyroid storm?
What is the mechanism of action for propranolol when used in the context of thyroid storm?
What biological process does the hypothalamus initiate to influence the production of thyroid hormones?
What biological process does the hypothalamus initiate to influence the production of thyroid hormones?
Which drug acts as an adjuvant treatment during a thyroid storm?
Which drug acts as an adjuvant treatment during a thyroid storm?
Which of the following statements about levothyroxine is false?
Which of the following statements about levothyroxine is false?
What structural feature differentiates anti-thyroid drugs from thyroid hormones?
What structural feature differentiates anti-thyroid drugs from thyroid hormones?
What is the typical action of sodium iodine when used therapeutically?
What is the typical action of sodium iodine when used therapeutically?
What is the primary function of thyroid hormones T3 and T4?
What is the primary function of thyroid hormones T3 and T4?
Which factor is necessary for the synthesis of thyroid hormones?
Which factor is necessary for the synthesis of thyroid hormones?
What effect does T3 have on catecholamine activity?
What effect does T3 have on catecholamine activity?
What happens when outer ring de-iodination of T4 occurs?
What happens when outer ring de-iodination of T4 occurs?
Which statement best describes the composition of thyroid hormones?
Which statement best describes the composition of thyroid hormones?
What role do glucocorticoids play in the regulation of the HPT axis?
What role do glucocorticoids play in the regulation of the HPT axis?
What is the main use of recombinant human TSH (Thyrogen®) in clinical practice?
What is the main use of recombinant human TSH (Thyrogen®) in clinical practice?
What physiological effect is associated with severe hypothyroidism during pregnancy?
What physiological effect is associated with severe hypothyroidism during pregnancy?
Which statement about T3 is correct?
Which statement about T3 is correct?
What is the primary mechanism of action for thyroid hormones like T4?
What is the primary mechanism of action for thyroid hormones like T4?
What is the mechanism of action of potassium iodide in treating thyroid conditions?
What is the mechanism of action of potassium iodide in treating thyroid conditions?
Which of the following is a contraindication for administering radioactive iodine (Iodotope)?
Which of the following is a contraindication for administering radioactive iodine (Iodotope)?
Which adverse effect is associated with the use of radioactive iodine?
Which adverse effect is associated with the use of radioactive iodine?
What is a significant interaction when using propylthiouracil (PTU)?
What is a significant interaction when using propylthiouracil (PTU)?
How does fluoroborate function as an ionic inhibitor?
How does fluoroborate function as an ionic inhibitor?
What is a common side effect of potassium iodide therapy?
What is a common side effect of potassium iodide therapy?
What primary condition is treated with antithyroid drugs like methimazole?
What primary condition is treated with antithyroid drugs like methimazole?
What is a notable pharmacokinetic property of propylthiouracil (PTU)?
What is a notable pharmacokinetic property of propylthiouracil (PTU)?
What is the role of T3 in relation to T4 when binding to thyroid receptors?
What is the role of T3 in relation to T4 when binding to thyroid receptors?
In terms of competitive inhibition, which ion is NOT typically used?
In terms of competitive inhibition, which ion is NOT typically used?
Which factor is NOT listed as a regulator of thyroid function?
Which factor is NOT listed as a regulator of thyroid function?
What is the primary mechanism by which thioamides such as propylthiouracil exert their therapeutic effect?
What is the primary mechanism by which thioamides such as propylthiouracil exert their therapeutic effect?
How does hyperthyroidism affect plasma LDL levels?
How does hyperthyroidism affect plasma LDL levels?
Which step is NOT part of the biosynthesis of thyroid hormones?
Which step is NOT part of the biosynthesis of thyroid hormones?
What is a common effect of thyrotoxicosis on insulin sensitivity?
What is a common effect of thyrotoxicosis on insulin sensitivity?
Which of the following is a preferred treatment approach for younger patients with hyperthyroidism?
Which of the following is a preferred treatment approach for younger patients with hyperthyroidism?
What is the rationale for using levothyroxine in small doses in elderly patients?
What is the rationale for using levothyroxine in small doses in elderly patients?
Which of the following medications is NOT considered an antithyroid drug used to treat hyperthyroidism?
Which of the following medications is NOT considered an antithyroid drug used to treat hyperthyroidism?
What is the primary goal of levothyroxine replacement therapy in patients with hypothyroidism?
What is the primary goal of levothyroxine replacement therapy in patients with hypothyroidism?
In the context of the provided information, what is the reason for the elevated TSH level in the 69-year-old man with a history of myocardial infarction and recurrent ventricular arrhythmia?
In the context of the provided information, what is the reason for the elevated TSH level in the 69-year-old man with a history of myocardial infarction and recurrent ventricular arrhythmia?
Which of the following factors may influence the thyroxine dose in a patient with hypothyroidism and a history of myocardial infarction and recurrent ventricular arrhythmia?
Which of the following factors may influence the thyroxine dose in a patient with hypothyroidism and a history of myocardial infarction and recurrent ventricular arrhythmia?
What is the preferred treatment approach for hyperthyroidism in older patients with cardiac disease?
What is the preferred treatment approach for hyperthyroidism in older patients with cardiac disease?
Why is levothyroxine preferred over liothyronine in the management of hypothyroidism?
Why is levothyroxine preferred over liothyronine in the management of hypothyroidism?
Flashcards
TR binding to DNA before ligand binding
TR binding to DNA before ligand binding
Thyroid hormone receptors (TRs) bind to DNA (specifically to thyroid response elements, TRE, via their DNA-binding domain, TR-DBD) before binding to a ligand.
T3 & T4 transport to the nucleus
T3 & T4 transport to the nucleus
Free T3 and T4 are transported into the cell and then translocate to the nucleus.
Ligand Binding to TR
Ligand Binding to TR
Ligand binding to TR happens through the ligand-binding domain (TR-LBD). T3 has a higher binding affinity to TR than T4.
Co-repressor dissociation
Co-repressor dissociation
Signup and view all the flashcards
Multiple TR Subtypes
Multiple TR Subtypes
Signup and view all the flashcards
Endocrine Axis
Endocrine Axis
Signup and view all the flashcards
Hypothalamus-Pituitary-Thyroid (HPT) Axis
Hypothalamus-Pituitary-Thyroid (HPT) Axis
Signup and view all the flashcards
HPT Axis Function
HPT Axis Function
Signup and view all the flashcards
Thyroid Hormone Synthesis
Thyroid Hormone Synthesis
Signup and view all the flashcards
Thyroid Hormone Analogs
Thyroid Hormone Analogs
Signup and view all the flashcards
Anti-thyroid Drugs
Anti-thyroid Drugs
Signup and view all the flashcards
Thionamide Anti-thyroid Drugs
Thionamide Anti-thyroid Drugs
Signup and view all the flashcards
Beta Blockers in Hyperthyroidism
Beta Blockers in Hyperthyroidism
Signup and view all the flashcards
HPT Axis
HPT Axis
Signup and view all the flashcards
Thyrotropin-Releasing Hormone (TRH)
Thyrotropin-Releasing Hormone (TRH)
Signup and view all the flashcards
Thyroid-Stimulating Hormone (TSH)
Thyroid-Stimulating Hormone (TSH)
Signup and view all the flashcards
Thyroxine (T4)
Thyroxine (T4)
Signup and view all the flashcards
Triiodothyronine (T3)
Triiodothyronine (T3)
Signup and view all the flashcards
Negative Feedback Loop
Negative Feedback Loop
Signup and view all the flashcards
Hypothyroidism
Hypothyroidism
Signup and view all the flashcards
Hyperthyroidism
Hyperthyroidism
Signup and view all the flashcards
Thyrotropin Alpha (Thyrogen®)
Thyrotropin Alpha (Thyrogen®)
Signup and view all the flashcards
Nuclear Receptor Mechanism
Nuclear Receptor Mechanism
Signup and view all the flashcards
Peripheral Deiodination
Peripheral Deiodination
Signup and view all the flashcards
Thyroid Binding Globulin (TBG)
Thyroid Binding Globulin (TBG)
Signup and view all the flashcards
Levothyroxine (Synthroid)
Levothyroxine (Synthroid)
Signup and view all the flashcards
Liothyronine (Cytomel)
Liothyronine (Cytomel)
Signup and view all the flashcards
Liotrix (Thyrolar)
Liotrix (Thyrolar)
Signup and view all the flashcards
Hashimoto's Thyroiditis
Hashimoto's Thyroiditis
Signup and view all the flashcards
Propylthiouracil (PTU)
Propylthiouracil (PTU)
Signup and view all the flashcards
Methimazole (Tapazole)
Methimazole (Tapazole)
Signup and view all the flashcards
Carbimazole
Carbimazole
Signup and view all the flashcards
Desiccated Thyroid Extract (Armour Thyroid)
Desiccated Thyroid Extract (Armour Thyroid)
Signup and view all the flashcards
Monocarboxylic Acid Transporter (MCT)
Monocarboxylic Acid Transporter (MCT)
Signup and view all the flashcards
Phenytoin (Dilantin)
Phenytoin (Dilantin)
Signup and view all the flashcards
Amiodarone (Cordarone)
Amiodarone (Cordarone)
Signup and view all the flashcards
Ionic inhibitors
Ionic inhibitors
Signup and view all the flashcards
Radioactive Iodine (I131)
Radioactive Iodine (I131)
Signup and view all the flashcards
Graves' disease
Graves' disease
Signup and view all the flashcards
Anti-thyroid drugs (Thioamides)
Anti-thyroid drugs (Thioamides)
Signup and view all the flashcards
Potassium Iodide (KI)
Potassium Iodide (KI)
Signup and view all the flashcards
Perchlorate
Perchlorate
Signup and view all the flashcards
Delayed hypothyroidism
Delayed hypothyroidism
Signup and view all the flashcards
Why is levothyroxine preferred over liothyronine in treating hypothyroidism?
Why is levothyroxine preferred over liothyronine in treating hypothyroidism?
Signup and view all the flashcards
What is the mechanism of action of levothyroxine?
What is the mechanism of action of levothyroxine?
Signup and view all the flashcards
What are two major indications for levothyroxine?
What are two major indications for levothyroxine?
Signup and view all the flashcards
How is levothyroxine therapy monitored?
How is levothyroxine therapy monitored?
Signup and view all the flashcards
Why do we use levothyroxine in small doses in elderly patients?
Why do we use levothyroxine in small doses in elderly patients?
Signup and view all the flashcards
Why is the TSH elevated in a patient with hypothyroidism?
Why is the TSH elevated in a patient with hypothyroidism?
Signup and view all the flashcards
What factors might affect the thyroxine dose in a patient?
What factors might affect the thyroxine dose in a patient?
Signup and view all the flashcards
What is the goal of levothyroxine replacement therapy?
What is the goal of levothyroxine replacement therapy?
Signup and view all the flashcards
Study Notes
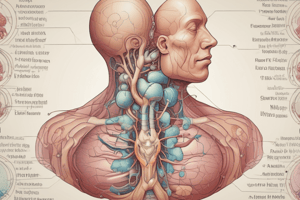
Endocrine Pharmacology: Thyroid Hormone Analogs & Inhibitors
- Thyroid hormones (T3 and T4) are crucial for metabolic processes, and their biosynthesis and regulation are crucial to understand
- The hypothalamus-pituitary-thyroid (HPT) axis plays a vital role in this regulation by triggering hormone production
- The hypothalamus releases TRH, which stimulates the pituitary to release TSH
- The thyroid gland produces T3 and T4 in response to TSH
- T3 and T4 have broad physiological effects impacting growth, development, metabolism, and cardiovascular function
- Iodide is essential for thyroid hormone synthesis; its uptake, oxidation, and incorporation into tyrosine molecules are carefully regulated steps
- Thyroid hormone analogs and inhibitors are used to treat hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid)
- Hypothyroidism is treated using synthetic T3 or T4, while hyperthyroidism is treated using drugs like methimazole or propylthiouracil that inhibit T3 and T4 synthesis or block their release
Hypothyroidism
- Symptoms of hypothyroidism include dry skin, coarse hair, puffy face, slow heartbeat, constipation, and weight gain
- Common treatments include desiccated thyroid, L-T4 (levothyroxine), and L-T3 (liothyronine)
- Issues like increased clotting factor catabolism affect anticoagulants.
Hyperthyroidism
- Symptoms of hyperthyroidism include hair loss, bulging eyes, enlarged thyroid, sweating, rapid heartbeat, weight loss, and tremor
- Treatments for hyperthyroidism include drugs like propylthiouracil (PTU) and methimazole (MMI) to inhibit thyroid hormone synthesis, or radioactive iodine to destroy thyroid tissue
- Beta-blockers, like propranolol, can help to control rapid heart rate and other symptoms.
Thyroid Hormone Synthesis and Regulation
- The hypothalamus produces TRH to stimulate the pituitary to release TSH
- TSH stimulates the thyroid gland to produce T3 and T4
- Thyroid hormones exert feedback loops on both the pituitary and hypothalamus
- Iodine is crucial for thyroid hormone synthesis
- T3 is more potent than T4, and T3 is more active than T4
Drugs to Treat Thyroid Hormone Deficiency
- Levothyroxine (T4) is often the treatment
- Liothyronine (T3) can be used in certain cases
- Dessicated thyroid (a natural extract) is rare
- Proper dosage and monitoring of thyroid hormone replacement are crucial; potential drug interactions can occur
Drugs to Treat Thyroid Hormone Excess
- Propylthiouracil (PTU)
- Methimazole
- Potassium iodide (KI)
- Radioactive iodine (I-131)
- Beta-blockers (used to manage symptoms)
Thyroid Storm
- Life-threatening exacerbation of hyperthyroidism
- Elevated thyroid hormone levels, often caused by stress
- Adjunctive therapy with drugs like propranolol to manage symptoms
Important Considerations and Clinical Implications
- Iodine intake affects thyroid hormone synthesis
- Medical conditions and other medication use must be considered when dosing thyroid-related medications.
- The doctor's monitoring is essential to adapt thyroid hormone levels
Laboratory Tests
- TSH (Thyroid-Stimulating Hormone)
- T3 and T4 (free and total)
- Thyroid-related tests must be monitored to maintain appropriate hormone levels.
Additional Information
- Important drug interactions with various medications
- Specific details on different drugs (e.g., PTU, MMI) to treat both hypothyroidism and hyperthyroidism
- Diagnostic and therapeutic management techniques are essential to consider
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.