Podcast
Questions and Answers
Match the type of injury with the appropriate splintage type:
Match the type of injury with the appropriate splintage type:
Patella Dislocation = Vacuum splint Tibia/Fibula shaft # = Long leg box splint Ankle # = Short leg vacuum splint Clavicle = Self splintage
Match the splintage type with its usage context:
Match the splintage type with its usage context:
Long leg vacuum splint = Tibia/Fibula shaft # Triangular sling = Humerus Short box splint = Foot #’s Kendrick Traction splint = Femur #
Match the injury to its non-usage conditions:
Match the injury to its non-usage conditions:
Femoral # = Cannot use Kendrick Traction splint if # to ankle Patella Dislocation = May spontaneously relocate when splinting Radius # = Use vacuum splint for forearm # Ulna = Use short box splint
Match the type of splint with its specifics:
Match the type of splint with its specifics:
Match the injury category with the related splint specifics:
Match the injury category with the related splint specifics:
Match the type of fracture with its description:
Match the type of fracture with its description:
Match the definition with the correct term related to joint injuries:
Match the definition with the correct term related to joint injuries:
Match the type of soft tissue injury with its characteristics:
Match the type of soft tissue injury with its characteristics:
Match the type of fracture to its alternative name:
Match the type of fracture to its alternative name:
Match the injury type with the typical example:
Match the injury type with the typical example:
Match the condition with its impact on bone health:
Match the condition with its impact on bone health:
Match the type of injury with the symptom:
Match the type of injury with the symptom:
Match the term with its treatment approach:
Match the term with its treatment approach:
Match the assessment methods for neurovascular status with their corresponding descriptions:
Match the assessment methods for neurovascular status with their corresponding descriptions:
Match the six ‘P’s of ischaemia with their corresponding symptoms:
Match the six ‘P’s of ischaemia with their corresponding symptoms:
Match the types of management for musculoskeletal injuries with their descriptions:
Match the types of management for musculoskeletal injuries with their descriptions:
Match the conditions that require time-critical assessment with the corresponding actions:
Match the conditions that require time-critical assessment with the corresponding actions:
Match the types of splinting with their intended purposes:
Match the types of splinting with their intended purposes:
Match the features of ischaemia with their types:
Match the features of ischaemia with their types:
Match the management steps for soft tissue injuries with their actions:
Match the management steps for soft tissue injuries with their actions:
Match the pain-related considerations with their definitions:
Match the pain-related considerations with their definitions:
Match the following musculoskeletal injury complications with their descriptions:
Match the following musculoskeletal injury complications with their descriptions:
Match the following injury types with their blood loss estimates:
Match the following injury types with their blood loss estimates:
Match the recommendations with their purpose in managing musculoskeletal injuries:
Match the recommendations with their purpose in managing musculoskeletal injuries:
Match the following consequences with their potential impact on a patient:
Match the following consequences with their potential impact on a patient:
Match the following statements with their relevance to musculoskeletal injuries:
Match the following statements with their relevance to musculoskeletal injuries:
Match the type of force with its description in musculoskeletal injuries:
Match the type of force with its description in musculoskeletal injuries:
Match the type of musculoskeletal injury with its example:
Match the type of musculoskeletal injury with its example:
Match the concept of pain management to its relevance:
Match the concept of pain management to its relevance:
Match the mechanism of injury with its characteristics:
Match the mechanism of injury with its characteristics:
Match the clinical action with its description in musculoskeletal injury assessment:
Match the clinical action with its description in musculoskeletal injury assessment:
Match the type of treatment interventions with their description:
Match the type of treatment interventions with their description:
Match the term related to injury with its definition:
Match the term related to injury with its definition:
Match the factor affecting musculoskeletal injuries with its impact:
Match the factor affecting musculoskeletal injuries with its impact:
Flashcards are hidden until you start studying
Study Notes
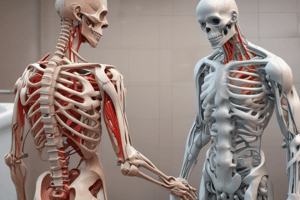
Introduction to Musculoskeletal Injuries
- Common injuries in the musculoskeletal (M/S) system range from sprains to fractures.
- Patients typically present with distress and pain; early pain management is crucial when feasible.
Mechanism of Injury (MOI)
- Determine MOI by analyzing direction, magnitude, and duration of force applied to the injury.
- A comprehensive review of MOI aids in predicting specific injury patterns.
Types of Forces
- Direct Force: Breaks occur at the impact point when force exceeds soft tissue limits.
- Indirect Force: Force travels through the skeleton to reach a weak point, leading to fractures.
Types of Fractures
- Closed Fractures:
- Also known as simple fractures, no skin puncture occurs.
- Compound Fractures:
- Open fractures where bone protrudes through the skin.
Pathological Fractures
- Frequent in older individuals, often occurring from minor trauma (e.g., falls).
- Conditions like cancer or osteoporosis increase fracture risk from minimal injuries.
Dislocations
- Defined as abnormal separation of joint surfaces; can occur alone or with fractures.
- Muscle spasms may lead to joint locking.
Sprains and Strains
- Sprains: Injury to ligaments, can involve partial or complete tears.
- Strains: Overstretching or tearing of muscle fibers and/or tendons.
- Sprains can be mistaken for fractures; immobilization is typically advised.
Management of Musculoskeletal Injuries
- Conduct an ABCDE assessment; identify time-critical injuries.
- Check for neurovascular status (Motor, Sensory, Circulation - MSC) before and after any manipulation.
- Remove tight clothing or jewelry; offer pain management as needed.
Six ‘P’s of Ischaemia
- Pain: Severe pain not alleviated by splinting or pain relief.
- Pallor: Indicates compromised blood flow.
- Paralysis: Loss of movement in the affected limb.
- Paraesthesia: Altered sensation.
- Pulselessness: Absence of peripheral pulses.
- Perishing Cold: Affected limb feels cold to touch.
Importance of Splinting
- Reduces pain and hemorrhage, protects blood vessels and nerves.
- Prevents further damage to surrounding tissues; supports the affected area.
Types of Splints for Injuries
- Neck of Femur: Figure of eight splint with padding.
- Shaft of Femur: Kendrick Traction splint; not for certain related fractures.
- Patella Dislocation: Vacuum and long leg box splints.
Time-Critical Injuries
- Mid shaft femoral fractures can result in significant blood loss, ranging from 500-2000 ml for open fractures.
- Pelvic fractures can lead to over 1000 ml blood loss.
Complications from Musculoskeletal Injuries
- Potential complications include bleeding, nerve/muscle/artery damage, infection, tissue loss, long-term disability, and compartment syndrome.
Conclusion
- Musculoskeletal injuries can cause significant pain and distress; effective splinting improves circulation care during transport to medical facilities.
- Continuous assessment of less visible life-threatening issues is essential in injury management.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.