Podcast
Questions and Answers
What is the typical progression of exercises used to treat radicular symptoms?
What is the typical progression of exercises used to treat radicular symptoms?
- Strengthening exercises, flexibility, pelvic-neutral exercises, and extension exercises
- Pelvic-neutral exercises, flexibility, strengthening exercises, and extension exercises
- Flexibility, strengthening exercises, pelvic-neutral exercises, and extension exercises
- Extension exercises, flexibility, strengthening exercises, and pelvic-neutral exercises (correct)
A facet joint in flexion is closed.
A facet joint in flexion is closed.
False (B)
What happens if radicular symptoms worsen during treatment?
What happens if radicular symptoms worsen during treatment?
You must re-evaluate the current exercises.
A facet joint in extension is ______________________.
A facet joint in extension is ______________________.
Match the following types of disc lesions with their corresponding locations:
Match the following types of disc lesions with their corresponding locations:
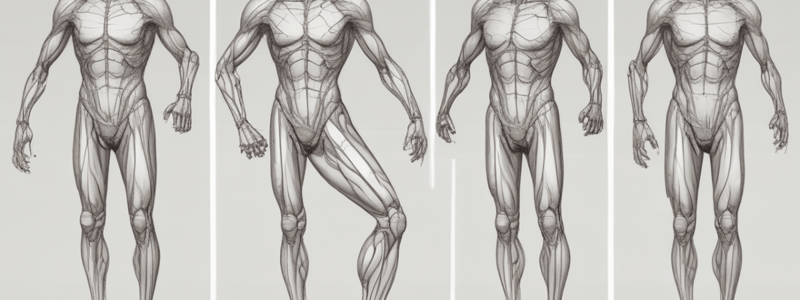
What is the characteristic arrangement of muscles in the Upper and Lower Crossed Syndromes?
What is the characteristic arrangement of muscles in the Upper and Lower Crossed Syndromes?
People with upper crossed syndrome often have lower crossed syndrome as well.
People with upper crossed syndrome often have lower crossed syndrome as well.
What is the result of hip flexor tightness in Lower Crossed Syndrome?
What is the result of hip flexor tightness in Lower Crossed Syndrome?
Upper Crossed Syndrome is associated with a forward head with _______________ cervical lordosis.
Upper Crossed Syndrome is associated with a forward head with _______________ cervical lordosis.
Match the following conditions with their associated injuries:
Match the following conditions with their associated injuries:
What are the three main regions of the vertebral column?
What are the three main regions of the vertebral column?
The spinal cord and nerve roots are located in the sacrum.
The spinal cord and nerve roots are located in the sacrum.
What is the primary function of the intervertebral discs?
What is the primary function of the intervertebral discs?
The transverse and spinous processes are attachments for _______________.
The transverse and spinous processes are attachments for _______________.
Match the following muscles with their location in the body:
Match the following muscles with their location in the body:
Which muscles provide spinal stability?
Which muscles provide spinal stability?
Core instability is linked to acute and chronic knee injuries.
Core instability is linked to acute and chronic knee injuries.
What are some common issues in low back pain?
What are some common issues in low back pain?
Maintaining correct posture is primarily a ______________________ activity.
Maintaining correct posture is primarily a ______________________ activity.
Match the following muscles with their primary fibre type:
Match the following muscles with their primary fibre type:
What is the first step in treating weakened muscles?
What is the first step in treating weakened muscles?
A maintenance program for patients should be created after the goals of the program are achieved.
A maintenance program for patients should be created after the goals of the program are achieved.
What are the two primary components of a maintenance program for patients with formerly tight and weak muscles?
What are the two primary components of a maintenance program for patients with formerly tight and weak muscles?
Signs and symptoms of sprains and strains include ______________________ during contraction.
Signs and symptoms of sprains and strains include ______________________ during contraction.
Match the following types of injuries with their characteristic signs and symptoms:
Match the following types of injuries with their characteristic signs and symptoms:
What should be avoided during weeks 0-6 post-injury in downhill skiing crash rehabilitation?
What should be avoided during weeks 0-6 post-injury in downhill skiing crash rehabilitation?
Overuse injuries such as bursitis and tendinopathies are caused by faulty biomechanics through repetitive motion.
Overuse injuries such as bursitis and tendinopathies are caused by faulty biomechanics through repetitive motion.
What typically causes ITB syndrome?
What typically causes ITB syndrome?
During weeks 6-8 post-injury, the rehabilitation program includes ______________________.
During weeks 6-8 post-injury, the rehabilitation program includes ______________________.
Match the following exercises with their corresponding time frames in the rehabilitation program:
Match the following exercises with their corresponding time frames in the rehabilitation program:
What is the outcome of a compromised ligament sprain?
What is the outcome of a compromised ligament sprain?
The outer core muscles include the transverse abdominis and diaphragm.
The outer core muscles include the transverse abdominis and diaphragm.
What does the Thomas Test measure?
What does the Thomas Test measure?
What is the outcome of maintaining pelvic neutral?
What is the outcome of maintaining pelvic neutral?
Muscle imbalances can cause soft tissue injuries and pain around the pelvis, hip, and thigh.
Muscle imbalances can cause soft tissue injuries and pain around the pelvis, hip, and thigh.
Abdominal hollowing facilitates the activation of ______________________ and multifidus.
Abdominal hollowing facilitates the activation of ______________________ and multifidus.
What is typically observed with lumbar lordosis?
What is typically observed with lumbar lordosis?
Muscle imbalances are characterized by tightness of a muscle group and ______________________ of the antagonist muscle group.
Muscle imbalances are characterized by tightness of a muscle group and ______________________ of the antagonist muscle group.
Match the following tests with their descriptions:
Match the following tests with their descriptions:
Match the following special tests with their purposes:
Match the following special tests with their purposes:
What percentage of total force required for overhead activities is contributed by the lower extremities and trunk?
What percentage of total force required for overhead activities is contributed by the lower extremities and trunk?
A posterior pelvic tilt places the hips in slight flexion.
A posterior pelvic tilt places the hips in slight flexion.
What happens when the gluteus medius is weak during single leg stance?
What happens when the gluteus medius is weak during single leg stance?
Hip muscles, especially hip extensors, abductors, and _______________, contribute to core stability during single leg activities.
Hip muscles, especially hip extensors, abductors, and _______________, contribute to core stability during single leg activities.
Match the following hip positions with their corresponding effects on the pelvic tilt:
Match the following hip positions with their corresponding effects on the pelvic tilt:
What are the three bones that form the pelvis?
What are the three bones that form the pelvis?
The sacroiliac joints (SIJ's) have a wide range of movement.
The sacroiliac joints (SIJ's) have a wide range of movement.
What is the importance of lumbopelvic-hip stability?
What is the importance of lumbopelvic-hip stability?
The lumbopelvic-hip complex includes the _______________________________________ spine, pelvis, and hips.
The lumbopelvic-hip complex includes the _______________________________________ spine, pelvis, and hips.
Match the following terms with their descriptions:
Match the following terms with their descriptions:
What is the typical mechanism of injury for Patellar Tendinopathy?
What is the typical mechanism of injury for Patellar Tendinopathy?
Iliotibial Band (ITB) Syndrome is usually caused by posterior pelvic tilt.
Iliotibial Band (ITB) Syndrome is usually caused by posterior pelvic tilt.
What is the outcome of maintaining pelvic neutral?
What is the outcome of maintaining pelvic neutral?
Knee Osteoarthritis is characterized by a breakdown of ______________________.
Knee Osteoarthritis is characterized by a breakdown of ______________________.
Match the following tests with their descriptions:
Match the following tests with their descriptions:
What is the primary function of the intervertebral discs?
What is the primary function of the intervertebral discs?
Total joint replacement is used as an 'end of the road' treatment option for knee OA.
Total joint replacement is used as an 'end of the road' treatment option for knee OA.
Patellofemoral Pain Syndrome is characterized by tenderness over the ______________________ facet of the patella.
Patellofemoral Pain Syndrome is characterized by tenderness over the ______________________ facet of the patella.
What is the outcome of a compromised ligament sprain?
What is the outcome of a compromised ligament sprain?
What is the primary function of the collateral ligaments in the knee?
What is the primary function of the collateral ligaments in the knee?
The patella glides inferiorly during knee extension.
The patella glides inferiorly during knee extension.
What is the screw-home mechanism in the knee?
What is the screw-home mechanism in the knee?
The quadriceps angle (Q-angle) is formed by a line from the _____________ to the middle patella and a line from the middle patella to the tibial tuberosity.
The quadriceps angle (Q-angle) is formed by a line from the _____________ to the middle patella and a line from the middle patella to the tibial tuberosity.
What is the primary cause of ligament sprains in the knee?
What is the primary cause of ligament sprains in the knee?
Match the following types of ligament sprains with their corresponding mechanisms:
Match the following types of ligament sprains with their corresponding mechanisms:
What is a common injury that can cause significant functional limitations in the knee joint?
What is a common injury that can cause significant functional limitations in the knee joint?
The knee is one of the least frequently injured joints in the body.
The knee is one of the least frequently injured joints in the body.
What are some common knee and thigh injuries?
What are some common knee and thigh injuries?
The knee is one of the most frequently injured joints in the body, causing significant ______________________ limitations.
The knee is one of the most frequently injured joints in the body, causing significant ______________________ limitations.
Match the following knee and thigh injuries with their descriptions:
Match the following knee and thigh injuries with their descriptions:
What is an important aspect of rehabilitation after a knee injury?
What is an important aspect of rehabilitation after a knee injury?
The knee joint is not essential for daily activities.
The knee joint is not essential for daily activities.
Why is it important to rehabilitate the knee and thigh properly after an injury?
Why is it important to rehabilitate the knee and thigh properly after an injury?
What is the primary function of the subtalar joint?
What is the primary function of the subtalar joint?
Pes Planus is characterized by an abnormally high longitudinal arch.
Pes Planus is characterized by an abnormally high longitudinal arch.
What is the name of the joint that connects the talus and calcaneus bones?
What is the name of the joint that connects the talus and calcaneus bones?
The lower leg has _______________ muscle compartments.
The lower leg has _______________ muscle compartments.
Match the following deformities with their characteristics:
Match the following deformities with their characteristics:
Ankle ligament sprains are one of the least common sports injuries.
Ankle ligament sprains are one of the least common sports injuries.
What is the result of supination of the foot?
What is the result of supination of the foot?
How many extrinsic muscles of the lower leg and foot are there?
How many extrinsic muscles of the lower leg and foot are there?
What is a common sign of a Soleus Strain?
What is a common sign of a Soleus Strain?
Achilles Tendinopathy is a sign of poor footwear.
Achilles Tendinopathy is a sign of poor footwear.
What is Medial Tibial Stress Syndrome (MTSS) also known as?
What is Medial Tibial Stress Syndrome (MTSS) also known as?
Plantar Fasciitis is a common injury that affects the ________________ surface of the foot.
Plantar Fasciitis is a common injury that affects the ________________ surface of the foot.
What is a common mechanism of injury for Achilles Tendinopathy?
What is a common mechanism of injury for Achilles Tendinopathy?
Medial Tibial Stress Syndrome (MTSS) is typically treated with rest and ice-massage.
Medial Tibial Stress Syndrome (MTSS) is typically treated with rest and ice-massage.
Match the following injuries with their corresponding signs and symptoms:
Match the following injuries with their corresponding signs and symptoms:
What is the primary function of the plantar aponeurosis?
What is the primary function of the plantar aponeurosis?
What is a common underlying cause of Medial Tibial Stress Syndrome (MTSS)?
What is a common underlying cause of Medial Tibial Stress Syndrome (MTSS)?
What is the most common mechanism of injury (MOI) for ankle ligament sprains?
What is the most common mechanism of injury (MOI) for ankle ligament sprains?
Grade III ankle sprains are the most common type of ankle sprain.
Grade III ankle sprains are the most common type of ankle sprain.
What is the primary goal of treatment for ankle sprains?
What is the primary goal of treatment for ankle sprains?
The _______________ ligament is commonly sprained in lateral ankle sprains.
The _______________ ligament is commonly sprained in lateral ankle sprains.
Match the following types of ankle sprains with their corresponding grades:
Match the following types of ankle sprains with their corresponding grades:
What is the primary cause of medial ankle sprains?
What is the primary cause of medial ankle sprains?
Syndesmosis sprains occur between the tibia and fibula.
Syndesmosis sprains occur between the tibia and fibula.
What is the typical location of a gastrocnemius strain?
What is the typical location of a gastrocnemius strain?
Study Notes
Functional Anatomy and Rehabilitation of the Vertebral Column
Vertebral Column Structure
- Consists of Cervical spine (C1-C7), Thoracic spine (T1-T12), Lumbar spine (L1-L5), Sacrum (S1-S5), and Coccyx
- Components: Intervertebral discs (shock absorbers), Ligaments (stability), Muscles (movement), Spinal cord, nerve roots, and peripheral nerves
Functional Anatomy and Biomechanics
- Movements: Flexion, lateral flexion, extension (limited), and rotation
- C3-L5: Transverse and spinous processes (attachments for ligaments and muscles)
- Articular processes
Intervertebral Discs (IVDs)
- Contain nociceptive fibers, contributing to pain
- Both IVDs and facets can contribute to pain
Muscles of the Back
- Superficial: [list of muscles]
- Deep: [list of muscles]
- Anterior Trunk: [list of muscles]
- Trunk: [list of muscles]
General Rehabilitation Considerations
- Exercise rehabilitation should be commenced early
- Includes posture, stability, flexibility, strength, and endurance exercises
- Posture examination: Standing and sitting posture
- Include body mechanics/ADLs (e.g., picking up objects from the floor, sit to stand)
- Gait examination: ROM, strength, special tests, palpation, outcome measures
Rehabilitation Techniques
- Soft Tissue Mobilisation: used to release trigger points in muscles, providing pain relief
- Flexibility Exercises: generally held for 30 seconds or more, repeated several times daily, to restore muscle imbalances, improve posture, and regain lost joint ROM
- Posture, Core, and Stabilisation Exercises: core (lumbo-pelvic-hip complex) provides spinal stability, increases intra-abdominal pressure, and involves transverse abdominis, multifidus, pelvic floor, and diaphragm
Disc Lesions and Radiculopathy
- L4/5 IVD and L5/S1 IVD
- Treatment: use of extension exercises, flexibility, strengthening exercises, and pelvic-neutral exercises
Facet Injuries
- Can be difficult to identify
- Often require investigative skills to identify
- Facet impingement and positional dysfunction: facet restriction can occur from an impingement following a traumatic event
Upper and Lower Crossed Syndromes
- Feature a cross-pattern arrangement of weak and tight muscles
- Upper Crossed Syndrome: forward head, upper cervical lordosis, thoracic kyphosis, protracted and winged scapulae, and internally rotated or abducted shoulders
- Lower Crossed Syndrome: excessive anterior pelvic tilt, hyperextension of the knees, and hip flexor tightness
- Treatment: patient education, postural changes, soft-tissue treatments, correction of muscle imbalances with flexibility and strengthening exercises
Sprains and Strains
- Signs and symptoms: tenderness on palpation, painful during contraction
- Treatment: REST, ice, compression, elevation, and rehabilitation exercises
Functional Anatomy and Rehabilitation of the Pelvis and Hip
Functional Anatomy and General Considerations
- The pelvis is composed of the left and right hemipelvis, joined at the pubic symphysis and sacroiliac joints (SIJs)
- The lumbopelvic-hip complex includes the spine, pelvis, and hips, with each segment influencing the other in terms of alignment and function
- The pelvis can tilt anteriorly or posteriorly, affecting the position of the hips and lumbar spine
- A total of 4-6 degrees of movement is possible at the SIJs, which can become hyper- or hypomobile
Sacroiliac Stabilization
- Sacroiliac stabilization is important for the transmission of forces through the kinetic chain and prevention of back and pelvic pain
- Three components of sacroiliac stabilization: form closure (anatomical stability of pelvic ring), force closure (muscles provide stability), and neuromotor control (proper activation and sequential recruitment of muscles)
- Ligament sprain compromises form closure, and focus is on improving force closure through strengthening and activation exercises to re-establish lumbopelvic-hip stability
The Core
- The core consists of inner (deep) core muscles (transverse abdominis, diaphragm, multifidus, and pelvic floor) and outer core muscles (erector spinae, rectus abdominis, external oblique, gluteal muscles, and thoracolumbar fascia)
- Core instability is linked to knee injuries, ankle sprains, and patellofemoral pain syndrome
- Hip muscles not only provide hip motion but also influence pelvis and trunk motion
Pelvic Neutral
- Pelvic neutral serves as a platform for lumbopelvic-hip stability and extremity performance
- The pelvis is stable when it is in pelvic neutral, which minimizes injury risk and optimizes load transfer
- Maintaining pelvic neutral in all activities is important for optimal function
Combining Local and Global Core Muscles
- Abdominal hollowing facilitates transverse abdominis and multifidus activation, but does not activate outer core muscles
- Abdominal bracing activates outer core muscles, and progressive exercises should be incorporated into functional activities
Pathological Sacral Alignment – Movement Tests
- Investigation of the sacroiliac region should include posture, alignment, and lumbar spine range of motion
- Tests for sacroiliac joint dysfunction include the standing forward-bend test, seated forward-bend test, kinetic test (Gillet test), and others
Here are the study notes for the text:
Functional Anatomy and Rehabilitation of the Knee and Thigh
Introduction
- Knee injuries are common and can cause significant functional limitations
- Knee joint is a complex structure that relies on sound function for daily activities such as walking, standing, and sitting
- Need to examine the entire kinetic chain to understand knee injuries, as restrictions or weakness in surrounding joints can contribute to knee pain
Knee Structure
- Tibiofemoral joint: concave tibial platform and convex femur
- Knee joint capsule surrounds the joint and merges with collateral ligaments
- Collateral ligaments provide medial, lateral, and rotational stability
- Cruciate ligaments provide anterior-posterior and rotational stability
- Medial and lateral meniscus cushion the joint, deepen the socket, and provide joint congruity
- Screw-home mechanism occurs in the last 30° of extension, where the tibia rotates laterally and the femur rotates medially
Patellofemoral Joint
- Patella sits in the femoral groove and glides superiorly during knee extension and inferiorly during knee flexion
- Patella stability is maintained by static (femoral groove, patellofemoral ligaments) and active (quadriceps) structures
- Quadriceps angle (Q-angle) is the angle formed by a line from the ASIS to the middle patella and a line from the middle patella to the tibial tuberosity
Factors Affecting Post-Injury Strength
- Oedema shuts down quadriceps function and is proportional to the quantity of fluid
- Pain can cause reflex inhibition and reduced muscle output
- Ambulation can cause weakness and bad habits to develop
Ligament Sprains
- Most knee ligament injuries result from an external force
- Anterior cruciate ligament (ACL) sprains are common, particularly in females
- Signs and symptoms of a grade 3 ACL rupture include a "pop" sound, immediate disability, knee instability, rapid swelling, and a positive anterior drawer test
- Treatment for ACL sprains includes PRICER, definitive diagnosis, arthroscopic examination, and reconstruction surgery
Posterior Cruciate Ligament (PCL) Sprain
- Mechanisms include external force and hyperextension
- Signs and symptoms include a "pop" sound, tenderness in the popliteal area, laxity in the posterior "sag" drawer, and rapid swelling
- Treatment includes PRICER, definitive diagnosis, arthroscopic examination, and reconstruction surgery
Collateral Ligament Sprains (MCL and LCL)
- Mechanisms include external force and rotation
- Non-surgical treatment includes bracing, crutches, active ROM exercises, and strength training
Meniscal Injuries
- Mechanisms include rotation while weight-bearing on the leg
- Signs and symptoms include severe pain, loss of movement, and peripheral tears
- Treatment includes conservative management vs. surgical repair/meniscectomy
Patellofemoral Pain Syndrome (PFPS)
- Mechanisms include lateral tracking of the patella, tight hamstrings, and excessive foot pronation
- Signs and symptoms include tenderness over the lateral facet of the patella, swelling, stiffness, and crepitus
- Treatment includes strengthening the VMO, adductors, and abductors, improving core strength, and stretching hamstrings and ITB
Iliotibial Band (ITB) Syndrome
- Mechanisms include postural problems, tight quads, and hip flexors
- Signs and symptoms include sharp stabbing pain over the lateral knee area
- Treatment includes addressing predisposing factors, training volume, posture education, flexibility and strength exercises, and corticosteroid injection
Patellar Tendinopathy (Jumper's Knee)
- Mechanisms include sudden or forceful repetitive knee extension
- Signs and symptoms include pain and tenderness at the inferior pole of the patella
- Treatment includes ice, correcting muscle strength and flexibility imbalances, eccentric strength training, and corticosteroid injection
Quadriceps Contusion ("Corky")
- Mechanisms include direct blow to the thigh
- Signs and symptoms include pain, loss of function, stiffness, and weakness
- Treatment includes PRICER, gentle passive stretching, and surgical intervention in extreme cases
Knee Osteoarthritis
- Characterized by a breakdown of articular cartilage, inflammation, narrowing of the joint space, and osteophyte formation
- Treatment includes normalizing biomechanics, increasing physical activity levels, reducing body mass if overweight or obese, pain medication, corticosteroid injection, and total joint replacement
Knee - Special Tests
- Patellar Grinding Test
- Anterior Draw Test
- Posterior Draw Test
- Valgus Stress Test
- Varus Stress Test
- Apley's Test
- McMurray's Test
Functional Anatomy and Biomechanics of the Ankle and Foot
- The lower leg consists of the tibia, fibula, and four muscle compartments.
- The tibia has a proximal tibiofemoral joint and tibial tuberosity (patella tendon), and a distal talocrural (ankle) joint that allows for plantarflexion and dorsiflexion.
- The subtalar joint, located between the talus and calcaneus, enables pronation and supination.
- Supination involves foot adduction, plantarflexion, and inversion, while pronation involves foot abduction, dorsiflexion, and eversion.
Muscle Function
- There are 12 extrinsic and 11 intrinsic muscles of the lower leg and foot.
Common Structural Deformities
- Pes Cavus: an abnormally high longitudinal arch, resulting in a rigid foot position with limited force absorption, increasing the risk of stress fractures and overuse injuries.
- Pes Planus: an abnormally low longitudinal arch, which may be rigid or flexible, and can cause little supination during gait, placing rotational stress on the hip, knee, plantar fascia, and Achilles tendon.
Ankle Ligament Sprains
- Ankle ligament sprains are one of the most common sports injuries, with a high risk in jumping sports (e.g., basketball, netball, volleyball) and running, especially on rough or uneven surfaces.
- Early treatment enhances recovery time.
- The most common mechanism of injury is inversion and plantarflexion.
- The ligaments commonly sprained are the anterior talofibular ligament, calcaneofibular ligament, and posterior talofibular ligament.
- Grading of ankle ligament sprains:
- Grade I: stretching of the anterior talofibular ligament, with mild pain and disability, and no loss of function.
- Grade II: tearing of the anterior talofibular ligament, with a tearing sensation, diffuse swelling, and point tenderness.
- Grade III: severe pain, diffuse swelling, and tenderness over the entire lateral ankle, with all three ligaments torn.
Lateral Ankle Sprains
- Treatment for Grade I sprains:
- PRICE (protection, rest, ice, compression, and elevation)
- Gentle ROM exercises
- Gradual weight-bearing
- Taping
- Rehabilitation exercises
- Treatment for Grade II sprains:
- PRICER (protection, rest, ice, compression, elevation, and rehabilitation)
- X-ray
- Crutches
- Air cast or camboot
- PF/DF exercises
- ROM and proprioceptive exercises
- 1-2 weeks of resumed weight-bearing
- Taping
- Graduated rehabilitation
- Treatment for Grade III sprains:
- PRICER
- Short walking cast for 4-6 weeks
- Similar to Grade II but with a longer healing time
- Problems can remain for 8-10 months
- Or surgery due to severe laxity and instability
Medial Ankle Sprains
- Medial ankle sprains are less common (<10% of ankle sprains) and often occur due to pronated or hypermobile feet.
- Mechanism of injury: usually ankle eversion.
- Signs and symptoms: pain, inability to weight-bear, and 2nd and 3rd degree sprains can cause significant instability.
Syndesmosis Sprain
- Syndesmosis sprains occur between the tibia and fibula, including the anterior talofibular ligament, posterior talofibular ligament, and interosseous membrane.
- Signs and symptoms: tenderness and swelling at the junction of the tibia and fibula, pain on weight-bearing, and talus may slip laterally and be unstable.
Gastrocnemius Strain
- Medial head at the musculotendinous junction is the most common site of injury.
- Mechanism of injury: quick starts and stops during sports (e.g., tennis, squash).
- Signs and symptoms: sudden pain in the calf, difficulty walking, especially on toes, local tenderness, and swelling.
- Treatment: PRICE, AROM/gentle stretches, and rehabilitation exercises to prevent scarring and repeated rupture.
Soleus Strain
- Signs and symptoms: pain located deep in the calf, pain triggered by tiptoe walking, bruising may appear on the medial border of the tibia, and deep local tenderness over the injured area.
- Treatment: PRICE, AROM/gentle stretches, and training the muscle to pain threshold with increasing load.
Achilles Tendinopathy
- Causes: overuse, prolonged and repeated stress, increased mileage, poor shoes, uneven surfaces, and pes cavus.
- Prevention: warm-up and stretching of both gastrocnemius and soleus, good quality training and competition shoes, and heel wedge if tension is felt in the Achilles tendon.
- Signs and symptoms: pain and swelling, crepitus felt over the tendon, erythema, weakness in plantarflexion, restricted dorsiflexion, and point tenderness.
Medial Tibial Stress Syndrome (MTSS)
- Also known as "shin splints" or "exercise-related leg pain."
- Causes: malalignment of the foot or lower leg, muscle fatigue, overuse stress, and sudden changes in training habits.
- Signs and symptoms: tenderness over the middle to distal medial margin of the tibia, pain occurring after activity, pain affecting performance, and local inflammation.
- Treatment: rest and ice-massage, taping, alternate heat and cold, stretching gastrocnemius, soleus, and deep PF's, aquatic rehabilitation, and orthotics.
Plantar Fasciitis
- One of the most common foot injuries, affecting the plantar aponeurosis, a thick fibrous band covering the plantar surface of the foot.
- Causes: pes cavus, pronated feet, increased mileage, poor shoes, and restricted dorsiflexion.
- Signs and symptoms: heel pain under load, morning stiffness, tenderness on pressure, pain if standing on tiptoes or heels, and sometimes heel spurs form.
- Treatment: rest and ice in acute stages, crutches to decrease load, tape to unload, checking shoes, and self-massage.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Quiz on functional anatomy and rehabilitation, covering topics related to EHR520 Week 5. Test your knowledge of human anatomy and rehabilitation techniques.