Podcast
Questions and Answers
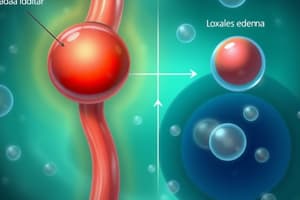
Which mechanism primarily drives fluid out of capillaries?
Which mechanism primarily drives fluid out of capillaries?
- Oncotic pressure
- Lymphatic drainage
- Hydrostatic pressure (correct)
- Colloid osmotic pressure
What type of edema fluid is characterized by a high protein content, often seen in inflammation?
What type of edema fluid is characterized by a high protein content, often seen in inflammation?
- Lymphatic fluid
- Exudate (correct)
- Transudate
- Pitting edema
Which condition is NOT a typical cause of pulmonary edema?
Which condition is NOT a typical cause of pulmonary edema?
- Lymphatic obstruction (correct)
- Acute lung injury
- Renal failure
- Left ventricular failure
What is a key morphological feature of brain edema?
What is a key morphological feature of brain edema?
In congestive heart failure, what leads to increased hydrostatic pressure, contributing to edema?
In congestive heart failure, what leads to increased hydrostatic pressure, contributing to edema?
What factor is associated with reduced plasma osmotic pressure?
What factor is associated with reduced plasma osmotic pressure?
Which condition is characterized by the fibrosis of lymphatics due to filariasis?
Which condition is characterized by the fibrosis of lymphatics due to filariasis?
Which of the following best describes the primary function of hemostasis?
Which of the following best describes the primary function of hemostasis?
What is a common feature of subcutaneous edema?
What is a common feature of subcutaneous edema?
What is the main cause of the appearance of bright red color in tissues during hyperemia?
What is the main cause of the appearance of bright red color in tissues during hyperemia?
A patient presents with significant swelling in the lower extremities after prolonged standing, but minimal impact in other areas. Which of these is the most likely explanation?
A patient presents with significant swelling in the lower extremities after prolonged standing, but minimal impact in other areas. Which of these is the most likely explanation?
Which of the following is the most likely consequence of inadequate hemostasis?
Which of the following is the most likely consequence of inadequate hemostasis?
What is the fundamental difference between hyperemia and congestion with respect to circulatory mechanisms?
What is the fundamental difference between hyperemia and congestion with respect to circulatory mechanisms?
Which of the following is most likely to result from a thromboembolism?
Which of the following is most likely to result from a thromboembolism?
In an acute scenario, what would be the direct consequence of impaired venous drainage?
In an acute scenario, what would be the direct consequence of impaired venous drainage?
What would be the most direct impact of decreased plasma protein content on capillary dynamics?
What would be the most direct impact of decreased plasma protein content on capillary dynamics?
What is the primary defect in Glanzmann Thrombasthenia?
What is the primary defect in Glanzmann Thrombasthenia?
Which enzyme is directly responsible for converting fibrinogen into fibrin?
Which enzyme is directly responsible for converting fibrinogen into fibrin?
Which of the following pathways is tested by the Prothrombin Time (PT) assay?
Which of the following pathways is tested by the Prothrombin Time (PT) assay?
In the in vivo coagulation process, what is the key activator of Factor IX?
In the in vivo coagulation process, what is the key activator of Factor IX?
Which laboratory assay is used to evaluate the intrinsic pathway of coagulation?
Which laboratory assay is used to evaluate the intrinsic pathway of coagulation?
What is the role of Factor XIII in hemostasis?
What is the role of Factor XIII in hemostasis?
Which vitamin is crucial for the gamma-carboxylation of certain coagulation factors?
Which vitamin is crucial for the gamma-carboxylation of certain coagulation factors?
What complex directly converts prothrombin to thrombin in the coagulation cascade?
What complex directly converts prothrombin to thrombin in the coagulation cascade?
Why does a deficiency in Factor XII not typically result in a severe bleeding disorder?
Why does a deficiency in Factor XII not typically result in a severe bleeding disorder?
Which of the following is NOT a key mechanism that limits coagulation from spreading beyond the injury site?
Which of the following is NOT a key mechanism that limits coagulation from spreading beyond the injury site?
Which of the following is NOT a direct effect of thrombin?
Which of the following is NOT a direct effect of thrombin?
What is the primary role of plasmin in the fibrinolytic cascade?
What is the primary role of plasmin in the fibrinolytic cascade?
Which molecule acts to rapidly inactivate free plasmin in circulation?
Which molecule acts to rapidly inactivate free plasmin in circulation?
Which of the following is synthesized by the endothelium and is most active when bound to fibrin, leading to localized fibrinolysis?
Which of the following is synthesized by the endothelium and is most active when bound to fibrin, leading to localized fibrinolysis?
In its anticoagulant role, what effect does thrombin have on intact endothelium?
In its anticoagulant role, what effect does thrombin have on intact endothelium?
Elevated levels of which clinical marker signal active thrombosis or fibrinolysis?
Elevated levels of which clinical marker signal active thrombosis or fibrinolysis?
Which component of Virchow's triad primarily contributes to the formation of arterial thrombi?
Which component of Virchow's triad primarily contributes to the formation of arterial thrombi?
What is a direct effect of stasis on the formation of a thrombus?
What is a direct effect of stasis on the formation of a thrombus?
Which of the following alterations in endothelial function promotes a prothrombotic environment?
Which of the following alterations in endothelial function promotes a prothrombotic environment?
A mutation in Factor V Leiden causes which alteration, increasing the risk of venous thrombosis?
A mutation in Factor V Leiden causes which alteration, increasing the risk of venous thrombosis?
How does turbulence contribute to thrombus formation?
How does turbulence contribute to thrombus formation?
Which condition exemplifies a state of combined stasis and turbulence, increasing the risk of thrombosis?
Which condition exemplifies a state of combined stasis and turbulence, increasing the risk of thrombosis?
What is the primary mechanism behind Heparin-Induced Thrombocytopenia (HIT)?
What is the primary mechanism behind Heparin-Induced Thrombocytopenia (HIT)?
Which of these is considered a high risk state for secondary (acquired) hypercoagulability?
Which of these is considered a high risk state for secondary (acquired) hypercoagulability?
Which of the following best describes the role of tissue plasminogen activator (t-PA) in hemostasis?
Which of the following best describes the role of tissue plasminogen activator (t-PA) in hemostasis?
How does thrombomodulin contribute to the anticoagulant properties of endothelial cells?
How does thrombomodulin contribute to the anticoagulant properties of endothelial cells?
Which of these is NOT an antithrombotic function of the endothelium?
Which of these is NOT an antithrombotic function of the endothelium?
How do heparin-like molecules on the endothelial cell surface contribute to anticoagulation?
How do heparin-like molecules on the endothelial cell surface contribute to anticoagulation?
What is the role of Tissue Factor Pathway Inhibitor (TFPI)?
What is the role of Tissue Factor Pathway Inhibitor (TFPI)?
According to Virchow’s Triad, which of the following is the most critical factor related to thrombosis?
According to Virchow’s Triad, which of the following is the most critical factor related to thrombosis?
Which substance is responsible for degrading ADP, thereby preventing further platelet activation?
Which substance is responsible for degrading ADP, thereby preventing further platelet activation?
Which of the following therapeutic agents enhances antithrombin activity?
Which of the following therapeutic agents enhances antithrombin activity?
Flashcards
Edema
Edema
Accumulation of fluid in tissues due to water movement into extravascular spaces.
Effects of Mild Edema
Effects of Mild Edema
Swelling in lower extremities after prolonged inactivity.
Severe Edema Impact
Severe Edema Impact
Pulmonary edema causes alveolar fluid accumulation, leading to life-threatening hypoxia.
Role of Hemostasis
Role of Hemostasis
Signup and view all the flashcards
Consequences of Inadequate Hemostasis
Consequences of Inadequate Hemostasis
Signup and view all the flashcards
Thromboembolism Outcomes
Thromboembolism Outcomes
Signup and view all the flashcards
Hyperemia
Hyperemia
Signup and view all the flashcards
Congestion
Congestion
Signup and view all the flashcards
Glanzmann Thrombasthenia
Glanzmann Thrombasthenia
Signup and view all the flashcards
Aspirin
Aspirin
Signup and view all the flashcards
Coagulation Factors
Coagulation Factors
Signup and view all the flashcards
Extrinsic Pathway
Extrinsic Pathway
Signup and view all the flashcards
Intrinsic Pathway
Intrinsic Pathway
Signup and view all the flashcards
Thrombin
Thrombin
Signup and view all the flashcards
Vitamin K Dependency
Vitamin K Dependency
Signup and view all the flashcards
Warfarin Therapy
Warfarin Therapy
Signup and view all the flashcards
Lymphatic Obstruction
Lymphatic Obstruction
Signup and view all the flashcards
Fluid Movement Regulation
Fluid Movement Regulation
Signup and view all the flashcards
Types of Edema Fluid
Types of Edema Fluid
Signup and view all the flashcards
Pulmonary Edema
Pulmonary Edema
Signup and view all the flashcards
Brain Edema
Brain Edema
Signup and view all the flashcards
Congestive Heart Failure
Congestive Heart Failure
Signup and view all the flashcards
Reduced Plasma Osmotic Pressure
Reduced Plasma Osmotic Pressure
Signup and view all the flashcards
Pitting Edema
Pitting Edema
Signup and view all the flashcards
PT Test
PT Test
Signup and view all the flashcards
PTT Test
PTT Test
Signup and view all the flashcards
Coagulation Cascade
Coagulation Cascade
Signup and view all the flashcards
Role of Plasmin
Role of Plasmin
Signup and view all the flashcards
D-dimers
D-dimers
Signup and view all the flashcards
t-PA Function
t-PA Function
Signup and view all the flashcards
Endothelial Regulation
Endothelial Regulation
Signup and view all the flashcards
α2-Plasmin Inhibitor
α2-Plasmin Inhibitor
Signup and view all the flashcards
t-PA
t-PA
Signup and view all the flashcards
Endothelial Function
Endothelial Function
Signup and view all the flashcards
Antithrombotic Activities
Antithrombotic Activities
Signup and view all the flashcards
Prostacyclin (PGI2)
Prostacyclin (PGI2)
Signup and view all the flashcards
Thrombomodulin
Thrombomodulin
Signup and view all the flashcards
Endothelial Protein C Receptor
Endothelial Protein C Receptor
Signup and view all the flashcards
Heparin
Heparin
Signup and view all the flashcards
Virchow’s Triad
Virchow’s Triad
Signup and view all the flashcards
Thrombosis
Thrombosis
Signup and view all the flashcards
Endothelial Injury
Endothelial Injury
Signup and view all the flashcards
Hypercoagulability
Hypercoagulability
Signup and view all the flashcards
Abnormal Blood Flow
Abnormal Blood Flow
Signup and view all the flashcards
Turbulence
Turbulence
Signup and view all the flashcards
Stasis
Stasis
Signup and view all the flashcards
Heparin-Induced Thrombocytopenia (HIT)
Heparin-Induced Thrombocytopenia (HIT)
Signup and view all the flashcards
Study Notes
Hemodynamic Disorders: Morphological Indicators
- Thromboembolic disease, shock, and disseminated intravascular coagulation (DIC) are morphological indicators of hemodynamic disorders.
Introduction to Circulatory Health: Key Functions of Circulation
- Delivers oxygen and nutrients.
- Removes metabolic waste products.
Normal Capillary Dynamics
- Minimal net movement of water/electrolytes into tissues.
Pathologic Disruptions
- Altered endothelial function.
- Increased vascular hydrostatic pressure.
- Decreased plasma protein content.
Edema - Definition and Implications
- Accumulation of fluid in tissues
- Caused by water movement into extravascular spaces.
- Mild: Swelling in lower extremities after prolonged inactivity.
- Severe: Pulmonary edema causing alveolar fluid accumulation → Life-threatening hypoxia.
Hemostasis and Vascular Integrity: Role of Hemostasis
- Blood clotting process after vascular damage.
Consequences of Inadequate Hemostasis: Hemorrhage (Excessive Bleeding)
- Tissue perfusion compromise.
- Potential for hypotension, shock, and death.
Thrombosis (Inappropriate Clotting)
- Formation of obstructive clots in blood vessels and, if the clot migrates, potential for ischemic cell death (infarction)
Clinical Relevance of Thromboembolism
-
Major Outcomes: Myocardial infarction, pulmonary embolism, cerebrovascular accident (stroke)
-
Significance: Leading causes of morbidity and mortality worldwide.
Hemodynamic Disorders Overview: Focus Areas
- Conditions increasing blood volumes.
- Impact on local and systemic circulatory systems.
Hyperemia and Congestion - Overview: Definitions
- Increased blood volume in tissue
- Hyperemia (Active Process): Caused by arteriolar dilation → increased blood inflow. Common during inflammation or in exercising skeletal muscle. Appearance: Bright red due to oxygenated blood..
- Congestion (Passive Process): Caused by impaired venous outflow. Common in systemic cardiac failure or localized venous obstruction. Appearance: Blue-red (cyanotic) due to deoxygenated hemoglobin.
Clinical Consequences of Congestion: Acute vs. Chronic Congestion
- Acute: Impaired venous drainage → capillary rupture and edema.
- Chronic: Persistent hypoxia → parenchymal cell death, fibrosis. Elevated pressures → capillary rupture → focal hemorrhages.
Morphology of Hyperemia and Congestion: General Characteristics
- Wet cut surfaces, oozing blood.
- Variable edema and hemorrhage.
Acute Pulmonary Congestion
- Blood-engorged alveolar capillaries.
- Alveolar septal edema and intraalveolar hemorrhage.
Chronic Pulmonary Congestion
- Thickened and fibrotic alveolar septa.
- Presence of "heart failure cells" (macrophages with hemosiderin).
Chronic Hepatic Congestion: Acute Hepatic Congestion
- Distension of central vein and sinusoids.
- Central hepatocyte necrosis; fatty changes in periportal hepatocytes.
Chronic Passive Liver Congestion: "Nutmeg Liver"
- Central regions: Red-brown and depressed (necrosis, cell loss).
- Periportal regions: Tan, may exhibit fatty changes.
Key Histological Features: "Heart Failure Cells"
- Hemosiderin-laden macrophages in alveolar spaces.
- Derived from phagocytosed red cells leaking from congested capillaries.
Liver Morphology
- Red-brown congested zones vs. tan periportal hepatocytes.
- Reflects chronic venous congestion and ischemia.
Overview of Edema: Definitions
- Accumulation of interstitial fluid within tissues.
Distribution: Interstitial fluid
- Hydrothorax: Pleural cavity.
- Hydropericardium: Pericardial cavity.
- Ascites (Hydroperitoneum): Peritoneal cavity.
Severe Cases: Anasarca
- Generalized edema with profound swelling and fluid accumulation.
Causes of Edema - Increased Hydrostatic Pressure
- Impaired venous return
- Systemic: Congestive heart failure, constrictive pericarditis, liver cirrhosis.
- Localized: Venous obstruction (thrombosis, external pressure).
Reduced Plasma Osmotic Pressure (Hypoproteinemia)
- Protein loss (nephrotic syndrome, gastroenteropathy).
- Reduced synthesis (liver disease, malnutrition).
Lymphatic Obstruction
- Inflammation, neoplasia, postsurgical/irradiation effects..
Sodium and Water Retention
- Renal hypoperfusion, increased renin-angiotensin-aldosterone activation.
Inflammation
- Acute, chronic, or due to angiogenesis.
Overview of Edema - Fluid Movement Regulation
- Hydrostatic Pressure: Drives fluid out of capillaries.
- Colloid Osmotic Pressure: Pulls fluid into capillaries.
- Normal balance → Minimal interstitial fluid.
Edema Formation
- Increased hydrostatic pressure or reduced osmotic pressure.
- Lymphatic drainage overwhelmed → Fluid accumulates.
- Types of Edema Fluid: - Transudate: Protein-poor (from hydrostatic imbalance) - Exudate: Protein-rich (from inflammation)
Clinical Types of Edema: Subcutaneous
- Most pronounced in dependent areas (legs/sacrum).
- Pitting edema: Finger pressure leaves a depression, indicates underlying cardiac/renal disease.
- Pulmonary Edema: Causes: left ventricular failure, renal failure, acute lung injury; Morphology: Frothy, blood-tinged fluid; Clinical Effects: Impaired ventilation, increased risk of infection.
- Brain Edema: Causes: localized (abscess/tumor) or generalized injury; Morphology: Narrowed sulci, flattened gyri; Clinical Effects: Increased intracranial pressure, risk of herniation, and brain stem vascular compromise.
Pathophysiology in Specific Conditions: Congestive Heart Failure
- Reduced cardiac output → Venous pooling → Increased hydrostatic pressure.
- Key management strategies: Salt Restriction, Diuretics, Aldosterone antagonists
Reduced Plasma Osmotic Pressure: Causes and Consequences
- Albumin loss (nephrotic syndrome).
- Decreased synthesis (liver cirrhosis, malnutrition).
- Edema, hypoperfusion, secondary hyperaldosteronism
Lymphatic Obstruction: Examples
- Elephantiasis (fibrosis of lymphatics from filariasis).
- Peau d'orange (breast cancer obstruction).
Morphological Features of Edema
- Subcutaneous swelling, dependent regions; Frothy fluid in lungs; narrowed sulci in brain.
Clinical Implications of Edema
- Subcutaneous Edema: Indicator of systemic diseases (cardiac, renal), Impaired wound healing; Pulmonary Edema: Life-threatening, predisposes to infections; Brain Edema: Risk of herniation, vital function compromise, death
Overview of Hemorrhage: Definition and Causes
- Extravasation of blood from blood vessels.
- Trauma, Atherosclerosis, Chronic capillary bleeding in congested tissues, Inflammatory or neoplastic vessel wall erosion.
Exacerbating Factors of Hemorrhage
- Hemorrhagic diatheses: Defects in vessel walls, platelets, or coagulation factors.
Forms of Hemorrhage: External Bleeding vs. Internal Accumulation
- Hematoma: Trivial (bruises), Fatal (retroperitoneal hematoma - e.g., aortic aneurysm rupture); Large Cavity Hg: Hemothorax, hemopericardium, hemoperitoneum, hamarthrosis.
- Jaundice: Large hemorrhages → Hemoglobin breakdown → Bilirubin accumulation.
Types of Hemorrhages
- Petechiae: Minute, Thrombocytopenia, Defective platelet function, Vitamin C deficiency (scurvy).
- Purpura: Slightly larger, trauma, vasculitis, and vascular fragility.
- Ecchymoses: Large, subcutaneous hematomas (bruises). Hemoglobin (red-blue) → Bilirubin (blue-green) →Hemosiderin (golden-brown).
Clinical Impact of Hemorrhage
- Factors Affecting Severity: Volume and rate of blood loss; Bleed location; Individual health status; Tolerated Loss: Healthy adults: Up to 20% blood volume; Greater losses: Risk of hemorrhagic (hypovolemic) shock. Location-Specific Effects: Subcutaneous: Often trivial; Brain: Potentially fatal (e.g., intracerebral hemorrhage)
Chronic vs. Acute Blood Loss
- Chronic/Recurrent Blood Loss: Examples: Peptic ulcers, menstrual bleeding, Consequence: Iron deficiency anemia (loss of hemoglobin iron); Internal Bleeding: Example: Hematomas, No iron deficiency: Efficient iron recycling from phagocytosed red cells.
Morphological Examples
- Petechial Hemorrhages: Example: Colonic mucosa in thrombocytopenia (Fig. 3.4A); Intracerebral Hemorrhage: Fatal outcomes due to pressure on vital brain structures (Fig. 3.4B).
Overview of Hemostasis and Thrombosis
- Hemostasis: Normal process to prevent blood loss after vascular injury, Involves platelets, clotting factors, and endothelium; Thrombosis: Pathologic formation of a clot (thrombus) within vessels, Occurs in vessels damaged by disease processes
Steps in Hemostasis: Arteriolar Vasoconstriction
- Immediate response to vascular injury, Neurogenic reflexes, Local release of endothelin (vasoconstrictor), Reduces blood flow transiently
Primary Hemostasis: Platelet Plug Formation
- Endothelial disruption → Exposure of subendothelial collagen, von Willebrand factor (vWF) binds collagen and promotes platelet adhesion, Platelet Activation: Shape change (flat plates with spiky protrusions), Granule release (e.g., ADP, thromboxane A2). Aggregation: Platelets recruited and adhere via fibrinogen and Gpllb-Illa receptors. Formation of a primary hemostatic plug
Secondary Hemostasis: Fibrin Deposition
- Tissue Factor Activation: Exposed at injury site (on smooth muscle cells and fibroblasts), Activates Factor VII → Initiates coagulation cascade, Thrombin Generation: Cleaves fibrinogen → Insoluble fibrin, Promotes further platelet aggregation, Result: Formation of a fibrin meshwork, Consolidates the platelet plug into a stable structure
Clot Stabilization
- Fibrin Crosslinking: Covalent bonds formed by Factor XIII, Platelet Contraction: Solidifies the clot structure. Outcome: Formation of a permanent hemostatic plug, Prevents further bleeding. Regulation: Counterregulatory mechanisms, Restrict clotting to injury site, Promote clot resorption and tissue repair.
Role of Endothelium in Hemostasis: Anticoagulant Functions (Healthy Endothelium)
-
Inhibits platelet aggregation, Prevents coagulation, Promotes fibrinolysis. Procoagulant Functions: Injury/Activation, Shifts balance to favor clot formation, Triggers for Activation
-
Microbial pathogens, Hemodynamic forces, Proinflammatory mediators
Clinical Relevance: Hemostasis and Thrombosis
- Essential to prevent excessive bleeding after injury; Common in conditions with endothelial dysfunction (e.g., inflammation, atherosclerosis); Risk of obstruction, ischemia, and tissue damage.
Overview of Platelets in Hemostasis: Role of Platelets
- Form primary plug sealing vascular defects, Provide a surface for activated coagulation factors.
- Origin: Anucleate cell fragments derived from megakaryocytes.
- Key Components: Glycoprotein receptors, Contractile cytoskeleton, a-Granules: Adhesion molecules (e.g., P-selectin, coagulation factors, wound healing proteins), Dense Granules: ADP, ATP, calcium, serotonin, epinephrine.
Platelet Activation Sequence: Platelet Adhesion
- Mediated by vWF acting as a bridge between: Exposed collagen in subendothelial connective tissue, Genetic Defects: Deficiency of vWF, Deficiency of Gplb receptor. Shape Change: Platelets become spiky, increasing surface area, Gpllb/llla receptors increase affinity for fibrinogen, Negatively charged phospholipids (e.g., phosphatidylserine) translocate to the surface: Bind calcium, Nucleation sites for coagulation factor complexes.
Platelet Activation: Triggered by and Granule Secretion
- Thrombin, Activates via protease-activated receptor (PAR); ADP: Released from dense granules, recruits more platelets; Granule Secretion: Release of ADP, calcium, and thromboxane A2 (TxA2); Aspirin Mechanism: Inhibits cyclooxygenase → Prevents TxA2 synthesis → Reduces aggregation; Growth Factor Contribution: PDGF promotes vessel wall repair
Platelet Aggregation: Mechanism and Stabilization
- Activated Gpllb/llla binds fibrinogen, Forms bridges between platelets; Initial aggregation is reversible; Thrombin: Promotes irreversible aggregation, Converts fibrinogen → Insoluble fibrin, Fibrin crosslinking consolidates the plug; Cytoskeleton: Platelet contraction strengthens aggregated platelets.
Hemostatic Plug
- Components: Platelets, Fibrin mesh, Entrapped red cells and leukocytes (Leukocytes adhere to P-selectin on activated platelets); Result: Definitive secondary hemostatic plug
Clinical Correlations
- Disorders of Platelet Function; Von Willebrand Disease: Impaired adhesion, Bernard-Soulier Syndrome: Defective Gplb receptor; Glanzmann Thrombasthenia: Deficiency of GpIIb/Illa receptor → Aggregation failure; Therapeutic Interventions: Aspirin, Platelet-related therapies in bleeding disorders
Overview of Coagulation Factors
- Role in Hemostasis: Series of enzymatic reactions leading to fibrin clot deposition, Components of Each Reaction: Enzyme: Activated coagulation factor, Substrate: Inactive proenzyme, Cofactor: Reaction accelerator, Assembly: On negatively charged phospholipid surfaces (platelets), Requires calcium and y-carboxylated glutamic acid (Vitamin K-dependent).
Coagulation Pathways: Extrinsic and Intrinsic Pathways
- Extrinsic Pathway: Test: Prothrombin Time (PT); Factors Assessed: X, VII, V, II (prothrombin), fibrinogen; Initiation: Tissue factor, phospholipids, and calcium; Intrinsic Pathway: Test: Partial Thromboplastin Time (PTT); Factors Assessed: XII, XI, IX, VIII, X, V, II, fibrinogen; Initiation: Negatively charged particles (e.g., glass), phospholipids, and calcium
In Vivo vs. In Vitro Coagulation
-
In Vitro: Cascade driven by either intrinsic or extrinsic factors, Tissue Factor-Factor VIla Complex: Key activator of Factor IX, Factor IXa/VIlla Complex: Activates Factor X; Thrombin Feedback
-
Amplifies cascade by activating Factors V, VIII, XI, Converts fibrinogen into fibrin.
Key Coagulation Factor - Thrombin
- Central Role in Hemostasis; Fibrin Formation: Converts fibrinogen to crosslinked fibrin, Platelet Activation: Induces activation, aggregation, and contraction via PARs, Cascade Amplification: Activates Factors V, VIII, XI, Fibrin Stabilization: Activates Factor XIII for fibrin crosslinking; Broader Effects: Inflammation and Repair, Anticoagulant Effects.
Clinical Implications of Coagulation Factor Deficiencies
- Severe Bleeding: Deficiency in Factors V, VII, VIII, IX, X, or prothrombin, Mild Bleeding, Factor XI deficiency; No Bleeding Disorder, Factor XII deficiency; Vitamin K Dependency: Factors II, VII, IX, X depend on y-carboxylation (Vitamin K); Warfarin Therapy: Antagonizes Vitamin K → Reduces clotting; Laboratory Assays: PT: Evaluates extrinsic pathway, PTT: Evaluates intrinsic pathway.
Coagulation Cascade Summary
- Sequential Activation: Factor IXa/Factor VIIla Complex: Activates Factor X; Factor Xa/Factor Va Complex: Converts prothrombin to thrombin; Essential Components: Phospholipid surfaces, calcium, and cofactors
Factors That Limit Coagulation
- Importance of Regulation: Prevent coagulation from spreading beyond the injury site; Dilution: Blood flow washes away activated coagulation factors, Factors removed by the liver, Requirement for Phospholipids: Provided by activated platelets only at the injury site; Endothelial Counterregulation: Intact endothelial cells adjacent to the injury inhibit coagulation.
Fibrinolytic Cascade
- Role: Limits clot size and facilitates clot dissolution; Key Enzyme: Plasmin, Breaks down fibrin, Prevents fibrin polymerization; Clinical Marker: D-dimers, Breakdown products of fibrin; indicate thrombotic activity.
Activation and Control of Plasmin : Plasminogen Activation
- Plasminogen: Inactive precursor circulating in blood, Activators: Tissue Plasminogen Activator (t-PA), Synthesized by endothelium, Most active when bound to fibrin → Localized fibrinolysis, Urokinase, Control of Plasmin: a2-Plasmin Inhibitor, Rapidly inactivates free plasmin in circulation.
Endothelial Regulation of Fibrinolysis: Endothelial-Derived Regulators
- Plasminogen Activator Inhibitors (PAIs); Negative regulators of plasmin activity, Prevent excessive fibrinolysis. Therapeutic Applications: t-PA as a Drug, Targets clots due to fibrin specificity; Used for thrombolytic therapy
Thrombin's Role in Regulation: Procoagulant Effects
- Cleaves fibrinogen → Fibrin, Activates Factor XIII → Fibrin crosslinking, Cellular Activation via PARs: Platelets: TxA2 secretion, aggregation, and degranulation, Endothelium: Generates adhesion molecules, Leukocytes: Enhances adhesion to endothelium, Anticoagulant Effects: On intact endothelium, thrombin prevents clot extension.
Clinical Significance of Thrombosis and D-dimer Testing
- Diagnostic Marker: Elevated levels signal active thrombosis or fibrinolysis; Therapeutic Implications: t-PA and Fibrinolytics, Effective for localized thrombus dissolution, Plasmin Control: Balance between clot stability and dissolution.
Overview of Endothelium in Hemostasis
- Balance between anticoagulant and procoagulant activities; Antithrombotic Activities: Directed toward (Platelets: Inhibition of activation and aggregation), (Coagulation Factors: Prevention of clotting), and Fibrinolysis: Promotion of clot dissolution
Platelet Inhibitory Effects
- Physical Barrier: Shields platelets from subendothelial vWF and collagen, Key Inhibitors: Prostacyclin (PGI2) and Nitric Oxide (NO), Inhibits platelet activation and aggregation; Promote vasodilation and washout of coagulation factors, Adenosine Diphosphatase: Degrades ADP, preventing platelet activation, Thrombin Binding: Endothelial cells inhibit thrombin's platelet-activating ability.
Anticoagulant Effects: Protection Against Coagulation and Key Molecules
- Shields coagulation factors
- Thrombomodulin: binds thrombin → converts thrombin to anticoagulant enzyme; Activates protein C → inhibits factors Va and VIIIa (requires Protein S); Endothelial Protein C Receptor, Enhances activation of Protein C; Heparin-Like Molecules, Activate antithrombin III → inhibits thrombin and factors IXa, Xa, Xla, Xlla; Tissue Factor Pathway Inhibitor (TFPI), Inhibits Tissue Factor/Factor VIla complexes.
Fibrinolytic Effects: Key Enzyme and Local Fibrinolysis
- Tissue Plasminogen Activator (t-PA), Synthesized by endothelial cells, Activates plasminogen → Plasmin, Localized fibrinolysis at the clot site.
Antithrombotic Effects
- Thrombomodulin: Binds thrombin → converts thrombin to an anticoagulant enzyme; Activates protein C → inhibits factors Va and VIIla (requires Protein S); Endothelial Protein C Receptor: Enhances activation of Protein C; Heparin-Like Molecules: Activate antithrombin III → inhibits thrombin and factors IXa, Xa, Xla, Xlla; Tissue Factor Pathway Inhibitor (TFPI): Inhibits Tissue Factor/Factor VIla complexes.
Clinical Relevance
- Therapeutic Implications: Heparin, Enhances antithrombin activity, t-PA, Fibrinolytic agent targeting clots.
- Pathological Considerations: Loss of endothelial antithrombotic properties → Increased risk of thrombosis
Virchow's Triad and Endothelial Integrity
- Endothelial Integrity: Most critical factor in thrombosis; Abnormal Blood Flow: Stasis or turbulence → Endothelial dysfunction, Hypercoagulability: Induced by procoagulant shifts; Key Takeaway: Endothelial health is pivotal in preventing thrombosis
Overview of Thrombosis: Definition and Key Underlying Abnormalities
- Formation of a blood clot, Endothelial injury; Abnormal blood flow (stasis or turbulence), Hypercoagulability of the blood.
Endothelial Injury and Thrombosis Role of Endothelial Injury
- Triggers platelet activation and thrombus formation, Particularly important in arterial and cardiac thrombi; Mechanisms: Severe injury, Exposure of vWF and tissue factor, Endothelial activation/dysfunction from, Physical injury, Infections, Cytokines and inflammatory mediators, Metabolic abnormalities, Toxins. Prothrombotic Changes; Downregulation of thrombomodulin, endothelial protein C receptor, tissue factor pathway inhibitor, Increased secretion of plasminogen activator inhibitors (PAIs)
Abnormal Blood Flow: Turbulence
- Causes endothelial injury and dysfunction, Forms countercurrents and pockets of stasis; Stasis, Slows washout of clotting factors, Allows platelet-endothelium interaction. Examples: Atherosclerotic plaques: Expose ECM and cause turbulence; Aneurysms: Local stasis promotes thrombosis; Atrial fibrillation: Combines stasis and turbulence; Hyperviscosity (e.g., polycythemia vera): Increases resistance and stasis
Hypercoagulability: Definition and Types
- Increased tendency; Primary (Genetic): Factor V Leiden, Prothrombin G20210A mutation, Protein C, S, or antithrombin deficiencies, Secondary (Acquired): High-risk states, Moderate-risk states.
Clinical Syndromes of Hypercoagulability
- Heparin-Induced Thrombocytopenia (HIT), Mechanism: Antibodies against heparin-PF4 complexes activate platelets., Paradoxical prothrombotic state despite low platelet count,Associated with: Unfractionated heparin > Low molecular weight heparins; Antiphospholipid Antibody Syndrome, Clinical Features, Recurrent thrombosis, pregnancy loss, cardiac valve vegetations; Renal microangiopathy → Renal failure, Mechanism, Antibodies target β2-glycoprotein I or other proteins bound to phospholipids; Types: Primary: Hypercoagulable state without autoimmune disease; Secondary: Associated with systemic lupus erythematosus; Therapy: Anticoagulation and immunosuppression
Genetic Testing and Thrombosis: Factor V Leiden and Prothrombin Mutation Testing
- Indicated in, Young patients (<50 years) with unprovoked DVT; Strong family history of thrombosis; Clinical Implications: Heterozygotes: Risk amplified by acquired factors (e.g., pregnancy), Homozygotes: Higher risk → Often lifelong anticoagulation
Therapeutic Implications of Thrombosis
- Anticoagulation Strategies: Factor V Leiden and Prothrombin Mutations, Lifelong anticoagulation for high-risk patients, HIT, Switch to non-heparin anticoagulants; Antiphospholipid Syndrome: Combine anticoagulation with immunosuppression. Lifestyle Modifications: Address risk factors (e.g., smoking cessation, weight management).
Conclusion: Thrombosis and Key Takeaways
- Thrombosis arises from a delicate imbalance of, Endothelial integrity; Blood flow dynamics; Coagulation system regulation; Early recognition and targeted intervention are critical in managing thrombotic risk.
Morphology of Thrombi: Sites of Formation, Attachment and Growth, and Fragmentation Risk
- Arterial/Cardiac Thrombi: Form at sites of endothelial injury or turbulence; Venous Thrombi: Form at sites of stasis, Attached to vascular surfaces; Growth direction: Arterial thrombi: Retrograde (against blood flow), Venous thrombi: Toward the heart (with blood flow), Fragmentation Risk: Propagating portions prone to embolization.
Lines of Zahn
- Laminations with alternating layers, Pale platelet and fibrin layers, Dark red cell-rich layers, Found in thrombi formed in flowing blood., Distinguishes antemortem thrombi from postmortem clots.
Types of Thrombi: Arterial and Venous Thrombi
- Arterial Thrombi: Characteristics, Rich in platelets; Often occlusive; Common Causes, Ruptured atherosclerotic plaques, Vascular injuries, Common Locations, Coronary arteries, cerebral arteries, femoral arteries; Venous Thrombi (Phlebothrombosis): Characteristics, Contain enmeshed red cells; Red or stasis thrombi; Almost invariably occlusive; Common Locations, Lower extremity veins (90%), upper extremity veins, periprostatic plexus, periuterine veins, Special cases: Dural sinuses, portal vein, hepatic vein.
Special Types of Thrombi: Mural Thrombi and Valve Thrombi (Vegetations)
- Mural Thrombi: Location, Heart chambers or aortic lumen; Causes, Abnormal myocardial contraction (e.g., arrhythmias, infarction), Endomyocardial injury (e.g., myocarditis, catheter trauma), Aortic thrombosis (e.g., from ulcerated atherosclerotic plaques, aneurysmal dilation); Valve Thrombi (Vegetations): Infective Endocarditis, Bacterial or fungal infections → Large thrombotic masses, Nonbacterial Thrombotic Endocarditis, Sterile vegetations in hypercoagulable states, Libman-Sacks Endocarditis, Sterile, verrucous vegetations in systemic lupus erythematosus.
Postmortem Clots vs. Venous Thrombi
- Postmortem Clots: Appearance: Gelatinous, Settled red cells - Dark red portion; Yellow "chicken fat" portion; Attachment: Not attached to vessel walls; Venous Thrombi: Appearance: Firm, focally attached, Contains gray fibrin strands; Distinction, Presence of attachment and laminations (lines of Zahn)..
Clinical Implications of Thrombi: Fragmentation and Embolization
- Propagation ,Increased risk of vascular occlusion and embolization, Occlusion Risks: Arterial thrombi → ischemia, Venous thrombi → pulmonary embolism; Diagnostic Importance: Distinction between antemortem and postmortem clots aids in determining cause of death.
Fates of Thrombi
- Propagation: Thrombus enlarges, Increases risk of vascular occlusion and embolization; Embolization: Part or all of the thrombus dislodges, Dissolution: Fibrinolysis leads to rapid shrinkage, Organization and Recanalization; Endothelial cells, smooth muscle, and fibroblasts grow; Capillary channels restore partial blood flow; May form a vascularized connective tissue mass
Morphological Features of Thrombi: Lines of Zahn, Postmortem Clots, and Organized Thrombus
- Lines of Zahn: Alternating pale platelet-fibrin layers and darker red cell-rich layers; Found in flowing blood, distinguishing antemortem thrombi from postmortem clots; Postmortem Clots: Gelatinous with red lower portion and yellow "chicken fat" upper portion, Non-adherent to vessel walls; Organized Thrombus: Endothelialization and capillary formation, May be incorporated into the vessel wall.
Clinical Significance of Thrombi: Venous and Arterial Thrombi
- Venous Thrombi: Complications, Congestion, edema, and embolization (e.g., pulmonary embolism), Superficial Venous Thrombi, Common in saphenous veins with varicosities, Deep Vein Thrombosis (DVT), Common in popliteal, femoral, and iliac veins, Often asymptomatic, Risk factors: Stasis, hypercoagulability, immobilization, trauma, pregnancy; Arterial Thrombi: Complications, Vessel occlusion → Infarction, Embolization, Common Causes, Atherosclerosis, myocardial infarction, atrial fibrillation.
Special Types of Thrombi: Mural Thrombi and Trousseau Syndrome
- Mural Thrombi: Located in heart chambers or aortic lumen; Associated with myocardial infarction, myocarditis, or aortic aneurysms; Trousseau Syndrome: Migratory thrombophlebitis linked to malignancy, Tumor-released procoagulants predispose to transient venous thrombi.
Risk Factors for Thrombosis: Venous and Arterial Thrombosis
- Venous Thrombosis: Primary (Inherited), Factor V Leiden mutation, prothrombin G20210A mutation, Protein C, S, or antithrombin deficiencies, Secondary (Acquired), Prolonged immobilization, surgery, cancer, pregnancy; Arterial Thrombosis, Endothelial damage due to atherosclerosis or trauma, Hypercoagulability
Clinical Management of Thrombosis: Diagnosis and Treatment
- Diagnosis: Imaging for DVT or emboli, D-dimer for fibrinolysis activity; Treatment, Anticoagulants: Heparin, warfarin, direct oral anticoagulants, Fibrinolytics: t-PA for newly formed thrombi, Compression Therapy: superficial venous thrombi; Prevention: Early mobilization, compression stockings, and anticoagulation in high-risk patients.
Overview of Embolism: Definitions and Types
- Definition: A detached intravascular solid, liquid, or gas mass transported by blood to a distant site, Types: Thromboembolism (most common); Fat, air, nitrogen bubbles, atherosclerotic debris, tumor fragments, bone marrow, or amniotic fluid.
Primary Effects of Embolism: Systemic and Pulmonary Embolisms
- Systemic Embolism, Ischemic necrosis (infarction), Pulmonary Embolism (PE), Hypoxia, hypotension, and right-sided heart failure.
Pulmonary Thromboembolism: Sources, Pathophysiology, Recorrent Emboli, and Paradoxical Embolism
-
Source: Deep venous thrombi (DVT), often from leg veins proximal to the popliteal fossa, Pathophysiology: Fragments travel to the pulmonary vasculature; Outcomes depend on embolus size and location, Small emboli, Large emboli, Medium emboli (dual circulation prevents infarction unless bronchial perfusion is compromised), Recurrent emboli (lead to pulmonary hypertension); Paradoxical embolism
-
Venous embolus enters systemic circulation through an atrial or ventricular defect
Systemic Thromboembolism: Sources, Destinations, Types, and Outcome
- Source: 80% from intracardiac mural thrombi, 66% from left ventricular infarcts, 25% from dilated left atria (e.g., mitral valve disease), Aortic aneurysms, atherosclerotic plaques, valvular vegetations, or paradoxical emboli; Destinations: Common sites: Lower extremities (75%), central nervous system (10%), Less common: Intestines, kidneys, spleen; Outcome, Depends on vessel caliber, collateral circulation, and tissue vulnerability. Often causes infarction in end-artery systems.
Fat Embolism Syndrome
- Causes: Long bone fractures, soft tissue crush injuries, Symptoms: Pulmonary insufficiency, neurological symptoms , onset: 1-3 days post injury, pathogenesis, Mechanical: Obstruction; Biochemical: Free fatty acids damage endothelium, Mortality Rate: ~10%
Amniotic Fluid Embolism
- Incidence and Mortality rate (Rare, 1 in 40,000 deliveries, ~80% mortality rate); Mechanism, Amniotic fluid enters maternal circulation, Activation of coagulation and innate immune systems; Clinical Features, Sudden dyspnea, cyanosis, shock, Seizures, coma, Pulmonary edema and DIC in survivors; Histology observations include fetal squamous cells
Air Embolism
- Causes, Iatrogenic, Surgery, obstetrics, chest trauma; Decompression Sickness, Rapid atmospheric pressure changes; Pathophysiology, Gas bubbles obstruct microvasculature; Acute Symptoms: bends (joint pain); respiratory distress, memory loss, coma., Chronic: Caisson disease → Ischemic necrosis in bones; Treatment: High-pressure chamber → Gradual decompression.
Clinical Management of Embolism: Pulmonary, Systemic, Fat, and Amniotic Fluid Embolisms
- Pulmonary embolism: Diagnosis (D-dimer, CT pulmonary angiography), Treatments, Anticoagulation, thrombolysis, IVC filters, recurrence prevention; Systemic embolism, Treatment (Anticoagulants, surgical removal if necessary) Fat embolism syndrome Supportive care (oxygen, fluids); Amniotic fluid embolism, Intensive care for respiratory and coagulation support; Air embolism High-pressure therapy (hyperbaric oxygen).
Overview of Disseminated Intravascular Coagulation (DIC)
- Definition, Systemic activation of coagulation pathways leading to widespread microthrombi, Consequences, Thrombosis: Tissue hypoxia, microinfarcts; Bleeding: Consumptive coagulopathy, pathologic fibrinolysis; Common triggers, Sepsis, obstetric complications, malignancy, trauma
Pathogenesis of DIC: Release of Procoagulants, Endothelial Damage
- Release of Procoagulants: Tissue factor from massive tissue injury, cancer cells, microbial endotoxins; Endothelial Damage: Causes, placenta, cancer cells, infections, complexes, Effects, tissue factor expression, downregulation of thrombomodulin.
Microvascular Thrombosis, Consumption, and Pathophysiology
- Widespread thrombin generation, Microthrombi, Consumption of platelets and clotting factors; Pathologic fibrinolysis, Fibrin degradation products, Inhibited hemostasis
Major Disorders Associated with DIC
- Obstetric Complications: Abruptio placentae, septic abortion, amniotic fluid embolism, eclampsia; Infections: Sepsis (gram-positive, gram-negative), meningococcemia, malaria; Neoplasms: Adenocarcinomas of pancreas, lung, stomach; acute promyelocytic leukemia; Massive Tissue Injury: Trauma, burns, extensive surgery, Miscellaneous: Acute hemolysis, snakebite, vasculitis, aortic aneurysm, liver disease.
Morphology of DIC: Commonly Affected Organs
- Kidneys: Fibrin thrombi, cortical necrosis; Adrenal Glands: Waterhouse-Friderichsen syndrome; Brain: Microinfarcts, hemorrhage; Heart and Pituitary: Infarcts, hemorrhages, Manifestations: Petechiae, ecchymoses, serosal hemorrhages, Diffuse microvascular thrombi.
Clinical Features of DIC: Acute and Chronic DIC
- Acute DIC, Rapid onset, Bleeding dominant (e.g., obstetric complications); Petechiae, ecchymoses, Severe hemorrhage (gut, urinary tract), Shock, renal failure, cyanosis, dyspnea; Chronic DIC, Insidious onset; Thrombosis-dominant (e.g., adenocarcinomas); Minimal bleeding; Laboratory abnormalities
Laboratory Findings of DIC
- Thrombocytopenia, Prolonged PT and PTT, Elevated fibrin degradation products (e.g., D-dimers), Reduced fibrinogen levels, Microangiopathic hemolytic anemia (schistocytes).
Management of DIC: Acute and Chronic DIC
- Acute DIC, Stabilize, Immediate Treatment: IV hydrocortisone, IV fluids, Correction: Antibiotics for sepsis; Treat underlying DIC or infections; Supportive Care: Monitor electrolytes, glucose, hemodynamic status; Chronic DIC: Address underlying malignancy or chronic condition; Supportive management for thrombotic complications
Summary of DIC: Simultaneous Clotting and Bleeding, Microthrombi and Common Causes, and Treatment
- DIC = Simultaneous clotting and bleeding, Microthrombi → Tissue hypoxia and infarction, Consumptive coagulopathy → Bleeding diathesis; Common Causes: Sepsis, obstetric complications, malignancy, trauma, Treatment: Treat underlying cause, Balance anticoagulation and bleeding control.
Overview of Acute Adrenocortical Insufficiency
- Definition, A life-threatening condition, Failure of the adrenal cortex to produce, Glucocorticoids, Mineralocorticoids; Key Causes, Massive Adrenal Hemorrhage, Acute Crisis in Chronic Insufficiency, Rapid Withdrawal of Exogenous Steroids
Causes of Acute Adrenocortical Insufficiency
- Massive Adrenal Hemorrhage: Conditions associated, Postoperative state, Disseminated intravascular coagulation (DIC), Overwhelming sepsis; Waterhouse-Friderichsen Syndrome, Classically linked to Neisseria meningitidis septicemia, Common in children but can occur at any age., Pathogenesis: Sepsis, endothelial injury, DIC, Adrenal hemorrhage; Acute Crisis in Chronic Insufficiency, Triggers: Acute stress, insufficient glucocorticoids; Rapid Withdrawal of Exogenous Steroids, Suppression of hypothalamic-pituitary-adrenal (HPA) axis, Adrenal glands atrophied, insufficient hormone production during stress
Waterhouse-Friderichsen Syndrome: Definitions, Clinical Presentation, Pathology
- Definition, Acute adrenal insufficiency due to bilateral adrenal hemorrhage during severe bacterial sepsis, Clinical Presentation: Rapid onset hypotension (shock), Fever, Disseminated intravascular coagulation (DIC) - Petechiae, purpura, Adrenal failure: Pathology; Extensive cortical destruction by hemorrhage.
Clinical Manifestations of Acute Adrenocortical Insufficiency: Symptoms and Signs
- Symptoms: Weakness, fatigue, Nausea, vomiting,abdominal pain, Hypotension, shock, Confusion, coma in severe cases; Signs of Adrenal Crisis: Dehydration, Hypoglycemia, Hyperkalemia, Hyponatremia
Diagnosis of Acute Adrenocortical Insufficiency: Clinical Suspicion, Laboratory Findings, and Imaging
- Clinical Suspicion: History of sepsis, anticoagulation, or steroid use, Acute presentation with shock and DIC, Laboratory Findings: Hypoglycemia, Hyperkalemia, Hyponatremia; Increased ACTH levels with low cortisol in primary insufficiency; Imaging: Adrenal hemorrhage on CT/MRI
Management of Acute Adrenocortical Insufficiency: Immediate Treatment, Correction Steps, and Supportive Care
- Immediate Treatment: IV hydrocortisone or dexamethasone, IV fluids for hypotension and electrolyte imbalances, Correction of Precipitating Cause: Antibiotics for sepsis, Treat underlying DIC or infections; Supportive Care: Monitor electrolytes, glucose, and hemodynamic status
Summary of Acute Adrenocortical Insufficiency
- Acute adrenocortical insufficiency is a life-threatening condition, Adrenal hemorrhage (Waterhouse-Friderichsen syndrome), Acute stress in chronic insufficiency, Rapid steroid withdrawal, Treatment: Rapid glucocorticoid replacement, Management of underlying triggers, Prevention of recurrence through careful steroid management.
Overview of Ischemic Necrosis of the Anterior Pituitary: Definitions, Most Common Causes, and Key Risk Factors
- Ischemic necrosis of the anterior pituitary caused by inadequate blood supply, Sheehan Syndrome: Postpartum necrosis of the anterior pituitary, Obstetric hemorrhage, Severe hypotension.
Pathophysiology of Sheehan Syndrome
- Pregnancy Changes: Anterior pituitary enlarges, Blood supply (from low-pressure hypophyseal portal venous system) does not increase proportionally; Obstetric Hemorrhage or Hypotension, Reduced blood flow → ischemia and necrosis; Posterior Pituitary Protection, Blood supply from direct arterial branches – Less vulnerable to ischemic injury.
Other Causes of Anterior Pituitary Necrosis
- Disseminated Intravascular Coagulation (DIC), Sickle Cell Anemia, Elevated Intracranial Pressure, Traumatic Injury, Shock of Any Origin, Checkpoint Blockade Therapy for Cancer.
Clinical Features of Sheehan Syndrome: Symptoms and Acute Presentation
- Symptoms of Anterior Pituitary Hormone Deficiency: Prolactin Deficiency, failure to lactate postpartum, Adrenocorticotropic Hormone (ACTH) Deficiency: Fatigue, hypotension, hypoglycemia, Thyroid-Stimulating Hormone (TSH) Deficiency, Hypothyroidism; Gonadotropin Deficiency: Amenorrhea, loss of pubic and axillary hair, Growth Hormone Deficiency: Weakness, poor wound healing; Acute Presentation: Severe hypotension and hypoglycemia in the postpartum period
Diagnosis of Sheehan Syndrome: History and Clinical Signs, Laboratory Findings, and Imaging
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.