Podcast
Questions and Answers
A client on ECMO suddenly exhibits decreased urine output, elevated potassium levels, and fluid retention. Which of the following complications is MOST likely indicated by these findings?
A client on ECMO suddenly exhibits decreased urine output, elevated potassium levels, and fluid retention. Which of the following complications is MOST likely indicated by these findings?
- Gastrointestinal bleeding
- Pulmonary edema
- Renal failure (correct)
- Sepsis
A patient on ECMO is receiving a neuromuscular blocker. What is the MOST important nursing intervention prior to and during the administration of this medication?
A patient on ECMO is receiving a neuromuscular blocker. What is the MOST important nursing intervention prior to and during the administration of this medication?
- Monitoring blood glucose levels
- Providing deep sedation (correct)
- Ensuring adequate pain management
- Administering a prophylactic antibiotic
After noticing a sudden drop in hemoglobin levels to 7.5 g/dL in an ECMO patient, what should be the nurse's priority intervention based on the provided information?
After noticing a sudden drop in hemoglobin levels to 7.5 g/dL in an ECMO patient, what should be the nurse's priority intervention based on the provided information?
- Ordering a chest X-ray
- Initiating a blood transfusion (correct)
- Increasing the rate of total parenteral nutrition
- Administering a dose of enoxaparin
Which combination of medications would MOST appropriately address both sedation and prevention of peptic ulcers in a patient receiving ECMO?
Which combination of medications would MOST appropriately address both sedation and prevention of peptic ulcers in a patient receiving ECMO?
A patient on ECMO is being monitored for early signs of sepsis. Which assessment finding would be MOST indicative of a developing septic process?
A patient on ECMO is being monitored for early signs of sepsis. Which assessment finding would be MOST indicative of a developing septic process?
Which of the following is a critical requirement for a patient to be considered a suitable candidate for CPAP therapy?
Which of the following is a critical requirement for a patient to be considered a suitable candidate for CPAP therapy?
A patient with which condition would be least suitable for BiPAP therapy due to the increased risk of complications?
A patient with which condition would be least suitable for BiPAP therapy due to the increased risk of complications?
What is the primary physiological effect of CPAP that makes it beneficial for treating conditions like obstructive sleep apnea?
What is the primary physiological effect of CPAP that makes it beneficial for treating conditions like obstructive sleep apnea?
A key difference between CPAP and BiPAP is that BiPAP:
A key difference between CPAP and BiPAP is that BiPAP:
Which of the following is true regarding both CPAP and BiPAP?
Which of the following is true regarding both CPAP and BiPAP?
A patient on CPAP is experiencing increased work of breathing. What is the physiological reason for this?
A patient on CPAP is experiencing increased work of breathing. What is the physiological reason for this?
Which of the following best explains how BiPAP assists in removing CO2 for clients who need ventilation support?
Which of the following best explains how BiPAP assists in removing CO2 for clients who need ventilation support?
When using BiPAP, the programmed rate determines:
When using BiPAP, the programmed rate determines:
What is the immediate concern when a high respiratory rate alarm sounds on a mechanically ventilated patient?
What is the immediate concern when a high respiratory rate alarm sounds on a mechanically ventilated patient?
Which of the following situations would most likely trigger an apnea alarm on a mechanical ventilator?
Which of the following situations would most likely trigger an apnea alarm on a mechanical ventilator?
A low tidal volume alarm is sounding on a patient's ventilator. What is the priority nursing intervention?
A low tidal volume alarm is sounding on a patient's ventilator. What is the priority nursing intervention?
How does increased intrathoracic pressure from mechanical ventilation affect cardiovascular function?
How does increased intrathoracic pressure from mechanical ventilation affect cardiovascular function?
What strategy is most effective in minimizing the risk of ventilator-associated pneumonia (VAP)?
What strategy is most effective in minimizing the risk of ventilator-associated pneumonia (VAP)?
A patient on mechanical ventilation has been on an FiO2 of 60% for 36 hours. Which assessment finding would suggest potential oxygen toxicity?
A patient on mechanical ventilation has been on an FiO2 of 60% for 36 hours. Which assessment finding would suggest potential oxygen toxicity?
Which nursing intervention is essential for preventing VAP in a mechanically ventilated patient?
Which nursing intervention is essential for preventing VAP in a mechanically ventilated patient?
What are the key components of assessing a patient's readiness for weaning from mechanical ventilation?
What are the key components of assessing a patient's readiness for weaning from mechanical ventilation?
A patient is on ECMO. Which coagulation lab value requires immediate notification to the provider?
A patient is on ECMO. Which coagulation lab value requires immediate notification to the provider?
How does ECMO support a patient with severe respiratory failure?
How does ECMO support a patient with severe respiratory failure?
A patient on mechanical ventilation is at risk for barotrauma. What physiological effect causes this condition?
A patient on mechanical ventilation is at risk for barotrauma. What physiological effect causes this condition?
When should a nurse consider the possibility of volutrauma in a patient on mechanical ventilation?
When should a nurse consider the possibility of volutrauma in a patient on mechanical ventilation?
Which of the following interventions is aimed at improving venous return when a patient is receiving mechanical ventilation?
Which of the following interventions is aimed at improving venous return when a patient is receiving mechanical ventilation?
A patient receiving ECMO is ordered to receive a continuous heparin infusion. What is the primary reason for this order?
A patient receiving ECMO is ordered to receive a continuous heparin infusion. What is the primary reason for this order?
In caring for a patient on ECMO, which of the following findings indicates a potential complication requiring immediate intervention?
In caring for a patient on ECMO, which of the following findings indicates a potential complication requiring immediate intervention?
Which condition necessitates invasive mechanical ventilation?
Which condition necessitates invasive mechanical ventilation?
What is the primary purpose of inflating the cuff of an endotracheal tube (ETT) immediately after placement?
What is the primary purpose of inflating the cuff of an endotracheal tube (ETT) immediately after placement?
What does a color change in an end-tidal CO2 detector indicate after ETT placement?
What does a color change in an end-tidal CO2 detector indicate after ETT placement?
What is the purpose of the obturator in a tracheostomy tube?
What is the purpose of the obturator in a tracheostomy tube?
What is the most appropriate initial response to a high-pressure alarm on a mechanical ventilator?
What is the most appropriate initial response to a high-pressure alarm on a mechanical ventilator?
In Assist Control (A/C) ventilation mode, what happens if the patient's respiratory rate falls below the set minimum?
In Assist Control (A/C) ventilation mode, what happens if the patient's respiratory rate falls below the set minimum?
How does Synchronized Intermittent Mandatory Ventilation (SIMV) differ from Assist Control (A/C)?
How does Synchronized Intermittent Mandatory Ventilation (SIMV) differ from Assist Control (A/C)?
What is the primary function of Positive End-Expiratory Pressure (PEEP) in mechanical ventilation?
What is the primary function of Positive End-Expiratory Pressure (PEEP) in mechanical ventilation?
What is the significance of noting the ETT marking at the teeth?
What is the significance of noting the ETT marking at the teeth?
A low-pressure alarm is sounding on a patient's ventilator. Which of the following is the most likely cause?
A low-pressure alarm is sounding on a patient's ventilator. Which of the following is the most likely cause?
In Pressure Support Ventilation, which parameters are determined by the patient's effort?
In Pressure Support Ventilation, which parameters are determined by the patient's effort?
Following the insertion of a tracheostomy tube, what steps should be taken to confirm correct placement?
Following the insertion of a tracheostomy tube, what steps should be taken to confirm correct placement?
What does the FiO2 setting on a mechanical ventilator represent?
What does the FiO2 setting on a mechanical ventilator represent?
Which of the following conditions might cause a high-pressure alarm in a mechanically ventilated patient?
Which of the following conditions might cause a high-pressure alarm in a mechanically ventilated patient?
What should be done with the obturator after a tracheostomy tube is successfully inserted?
What should be done with the obturator after a tracheostomy tube is successfully inserted?
Flashcards
Noninvasive Ventilation
Noninvasive Ventilation
Breathing assistance without an artificial airway (like a tube).
CPAP
CPAP
Continuous pressure during spontaneous breathing, increasing alveoli function.
CPAP Candidate Requirement
CPAP Candidate Requirement
Client's ability to remove the mask independently due to aspiration risk.
BiPAP
BiPAP
Signup and view all the flashcards
Common BiPAP Uses
Common BiPAP Uses
Signup and view all the flashcards
BiPAP Contraindications
BiPAP Contraindications
Signup and view all the flashcards
Benefit of BiPAP
Benefit of BiPAP
Signup and view all the flashcards
Pressure Relief (CPAP)
Pressure Relief (CPAP)
Signup and view all the flashcards
Internal Hemorrhage Signs
Internal Hemorrhage Signs
Signup and view all the flashcards
ECMO: Renal Failure Monitoring
ECMO: Renal Failure Monitoring
Signup and view all the flashcards
ECMO: Sepsis Monitoring
ECMO: Sepsis Monitoring
Signup and view all the flashcards
Neuromuscular Blockers
Neuromuscular Blockers
Signup and view all the flashcards
Propofol/Dexmedetomidine
Propofol/Dexmedetomidine
Signup and view all the flashcards
Endotracheal Tube (ETT)
Endotracheal Tube (ETT)
Signup and view all the flashcards
Laryngoscope
Laryngoscope
Signup and view all the flashcards
End-tidal CO2 detector
End-tidal CO2 detector
Signup and view all the flashcards
Tracheostomy Tube
Tracheostomy Tube
Signup and view all the flashcards
Obturator
Obturator
Signup and view all the flashcards
Assist Control (A/C) Ventilation
Assist Control (A/C) Ventilation
Signup and view all the flashcards
Synchronized Intermittent Mandatory Ventilation (SIMV)
Synchronized Intermittent Mandatory Ventilation (SIMV)
Signup and view all the flashcards
Pressure Support Ventilation/CPAP
Pressure Support Ventilation/CPAP
Signup and view all the flashcards
FiO2
FiO2
Signup and view all the flashcards
Positive End-Expiratory Pressure (PEEP)
Positive End-Expiratory Pressure (PEEP)
Signup and view all the flashcards
Pressure Support (PS)
Pressure Support (PS)
Signup and view all the flashcards
Ventilator Rate
Ventilator Rate
Signup and view all the flashcards
Tidal Volume
Tidal Volume
Signup and view all the flashcards
Ventilator Alarm Response
Ventilator Alarm Response
Signup and view all the flashcards
Causes of High-Pressure Alarm
Causes of High-Pressure Alarm
Signup and view all the flashcards
Apnea Alarm
Apnea Alarm
Signup and view all the flashcards
High Vt or RR Alarm
High Vt or RR Alarm
Signup and view all the flashcards
Low Vt Alarm
Low Vt Alarm
Signup and view all the flashcards
Barotrauma
Barotrauma
Signup and view all the flashcards
Volutrauma
Volutrauma
Signup and view all the flashcards
Atelectasis
Atelectasis
Signup and view all the flashcards
Oxygen Toxicity
Oxygen Toxicity
Signup and view all the flashcards
Spontaneous Breathing Trial (SBT)
Spontaneous Breathing Trial (SBT)
Signup and view all the flashcards
Sedation Vacation
Sedation Vacation
Signup and view all the flashcards
Weaning
Weaning
Signup and view all the flashcards
ECMO
ECMO
Signup and view all the flashcards
Bleeding
Bleeding
Signup and view all the flashcards
Heparin-Induced Thrombocytopenia (HIT)
Heparin-Induced Thrombocytopenia (HIT)
Signup and view all the flashcards
Minimize Sedation
Minimize Sedation
Signup and view all the flashcards
Study Notes
Noninvasive Ventilation
- Breathing assistance is provided without artificial airways like endotracheal tubes or tracheostomy through a mask, such as a full-face mask, nasal mask, or nasal prongs (pillows).
Continuous Positive Airway Pressure (CPAP)
- CPAP delivers continuous pressure during spontaneous breathing, enhancing alveoli capacity and function.
- Primary use is for treating obstructive sleep apnea.
- CPAP increases the work of breathing, as the client must forcibly exhale against the pressure.
- Clients must independently remove the CPAP mask to avoid aspiration from vomiting.
- Clients must be able to maintain their airway.
- CPAP is not suitable for those with excessive secretions.
- It delivers a set pressure to increase oxygen levels, reduce work of breathing, and decrease cardiac workload.
- CPAP helps to prevent airway collapse.
- Pressure relief settings aid user tolerance during exhalation by reducing pressure.
Bilevel Positive Airway Pressure (BiPAP)
- BiPAP delivers positive pressure at two levels: a higher pressure during inspiration and a lower pressure during expiration.
- It is used for clients with COPD, heart failure, respiratory failure and sleep apnea.
- Clients must be able to spontaneously breathe and comply with ventilation.
- Not suitable for those with increased secretions due to risk of aspiration.
- Clients with decreased mental status are not candidates due to their inability to remove the mask if needed.
- BiPAP is beneficial for removing CO2.
- Makes breathing easier and results in lower average airway pressure
- Delivers different pressure during inhalation and exhalation.
- A specific rate is programmed into the device.
- This ensures programmed pressure delivery at the programmed rate, regardless of the client's breathing.
CPAP and BiPAP Similarities
- Both are noninvasive ventilation modes.
- Therapy involves wearing a snug-fitting face mask.
Invasive Mechanical Ventilation
- Required for clients unable to protect their airway or provide adequate respiratory effort.
- Uses an endotracheal tube (ETT), which is inserted by a provider.
- Supplies needed include:
- Laryngoscope with Macintosh or Miller blades
- ETT (size to be determined by provider)
- 10 mL syringe
- Sedation medications
- The team involved includes a respiratory therapist and possibly a CRNA.
- Immediately after placement, the cuff is inflated to allow breaths to enter the lungs without leakage.
- Ventilate with an ambu-bag.
Confirming ETT Placement
- Placement confirmed with an end-tidal CO2 detector.
- Color change indicates the presence of CO2.
- Auscultate breath sounds for equal bilateral air movement.
- Auscultate the epigastrium for the absence of air movement in the stomach.
- Observe the chest for equal and symmetrical wall movement.
- Note the SpO2, which should improve and stabilize.
- CXR (chest x-ray) is the final confirmation of correct ETT placement.
- Note the depth of the ETT using markings on the tube.
- Assess the ETT size and insertion depth relative to the client’s anatomy.
- The pilot balloon is where air is inserted to inflate the cuff.
- The cuff is at the end of the tube inside the trachea.
Tracheostomy Tubes
- The obturator is a smooth guide used for tube insertion.
- Once inserted, the obturator is removed and kept in case of dislodgement.
- Inserted into the neck, bypassing the mouth and nose.
- Similarities to ETT: pilot balloon and cuff to occlude the airway
- Tracheostomy tubes are shorter, with size selected by the provider.
- After insertion, inflate the cuff and auscultate breath sounds.
- Use end-tidal CO2 capnography to confirm placement via color change.
- Pass a suction tube through the trach, then remove the ETT.
- Secure the tube to prevent dislodgement, and obtain a chest x-ray.
Modes of Ventilation
- Full Support Mode: Assist Control (A/C)
- Assists with each breath by providing volume or pressure.
- If respiratory rates fall below a setting, the ventilator will control ventilation.
- Partial Support Mode: Synchronized Intermittent Mandatory Ventilation (SIMV)
- Administers ventilation with the client’s inspiratory efforts.
- A preset rate ensures delivery of a fixed number of breaths at a fixed tidal volume.
- A patient can trigger a spontaneous breath with the volume determined by patient effort.
- Spontaneous Modes: Pressure Support Ventilation or CPAP
- Respiratory rate, tidal volume, and inspiratory times are determined by the patient.
- Requires that the patient can spontaneously initiate breaths.
Ventilator Settings
- FiO2: Percentage of oxygen in the air provided to the client.
- PEEP: Positive end-expiratory pressure is the amount of pressure remaining in the lungs upon expiration.
- PS (Pressure Support): Preset pressure to ease breathing when the client initiates a breath.
- Rate: Minimum respiratory rate before ventilation support begins.
- Tidal Volume: Amount of air moved into or out of the lungs with each breath.
Positive End-Expiratory Pressure (PEEP)
- Pressure is applied to the airways at the end of expiration to prevent atelectasis by keeping alveoli open.
Ventilator Alarms
- When an alarm sounds, immediately check the client and the equipment.
- If the issue is unclear, disconnect the client from the ventilator.
- Provide manual breaths with an ambu bag and call for help.
- High Pressure:
- Caused by increased circuit pressure.
- Causes include coughing, asynchronous breathing, condensation in tubing, kinked tubing, bronchospasms, or decreased lung compliance like pulmonary edema, ARDS, atelectasis, or tension pneumothorax.
- Low Pressure:
- Caused by decreased circuit pressure.
- Causes include disconnection of tubing or accidental extubation.
- Ensure tubing connections are tight.
- Apnea:
- Sounds when no breathing is sensed.
- Can occur in modes without a set rate.
- May indicate respiratory arrest or over-sedation.
- May require changing the ventilator setting or titrating sedation.
- High Vt or RR:
- Generally indicates the client is breathing too fast.
- Can be caused by pain, anxiety, infection, fever, hypoxia, or hypercapnia.
- Treat the underlying condition; verbal coaching can help with anxiety.
- Low Vt:
- Similar to low pressure but senses volume.
- Caused by disconnected tubing, leaks in the circuit, or cuff leaks in the ETT or tracheostomy tube.
- Reconnect tubing or consult with respiratory therapist to resolve air leaks.
Alarm Fatigue
- Tuning out frequent alarms can endanger clients.
Mechanical Ventilation Complications
- Cardiovascular:
- Increased intrathoracic pressure can decrease cardiac output and venous return.
- Pulmonary:
- Barotrauma: Rupture of the lungs due to added pressure.
- Volutrauma: Lung rupture due to high air volume.
- Atelectasis: Can result from insufficient volume or PEEP.
- Ventilator-Associated Pneumonia (VAP): Risk for all ventilated clients.
- Oxygen Toxicity: Can occur with FiO2 over 50% for more than 24-48 hours, causing fatigue, restlessness, nausea, vomiting, coughing, dyspnea, and hypoxia.
- Avoid this by using the lowest amount of oxygen to keep SpO2 > 90%.
- Never compromise oxygenation due to risk of oxygen toxicity.
Preventing Ventilator-Associated Pneumonia (VAP)
- The most effective way to prevent its is to remove the ventilator.
- Minimize sedation based on CPOT and RASS assessments.
- Nursing Interventions:
- Elevate the head of the bed.
- Perform range of motion exercises.
- Provide oral care.
- Assess and clean the skin frequently.
- Administer medications for peptic ulcer prophylaxis.
- Ensure nutritional needs are met via tube feeds or TPN.
- Daily spontaneous breathing trials and sedation vacations are implemented to assess readiness for ETT removal.
- A weaning process is used and determined by meeting pre-established criteria.
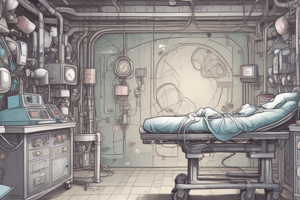
Extracorporeal Membrane Oxygenation (ECMO)
- Cardiopulmonary support delivered in the ICU.
- Blood is removed from the body, oxygenated and has carbon dioxide removed mechanically, then reinfused.
- Nurses Role: assessment, preventive care, and timely communication.
- Monitor for:
- Bleeding
- Thrombus formation
- Heparin-induced thrombocytopenia (HIT)
- Internal hemorrhaging
- Neurological changes
- Renal failure, oliguria
- Sepsis
- Prophylactic care:
- Suction secretions every 4 to 6 hr.
- Perform frequent position changes.
- Manage blood transfusions if hemoglobin levels drop below 8 g/dL.
- Provide total parenteral nutrition (TPN) to assist with maintaining nutrition, as well as fluid and electrolyte levels.
Medications used in Ventilation
| Medication | Class | Purpose | Nursing Considerations |
|---|---|---|---|
| Cisatracurium, Rocuronium | Neuromuscular Blocker (Paralytic) | Paralysis of muscles | Administer with sedation medication. |
| Midazolam, Lorazepam | Benzodiazepine | Sedation | Monitor LOC; client should be heavily sedated before giving a neuromuscular blocker. |
| Propofol, Dexmedetomidine | Anesthesia/Sedation | Provides sedation while on mechanical ventilation | Titrate to appropriate RASS. |
| Pantoprazole | Proton Pump Inhibitor | Prevention of peptic ulcers | Part of VAP prevention. |
| Enoxaparin | LMWH | Anticoagulation – DVT prevention | Part of VAP prevention. |
| Albuterol | Beta2 Agonist | Bronchodilation | Monitor lung sounds and HR. |
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.