Podcast
Questions and Answers
What is the term for drugs that produce their primary therapeutic effect by mimicking or altering the functions of the Autonomic Nervous System (ANS)?
What is the term for drugs that produce their primary therapeutic effect by mimicking or altering the functions of the Autonomic Nervous System (ANS)?
Autonomic drugs
Which receptor type are the postsynaptic nicotinic receptors in skeletal muscle cells?
Which receptor type are the postsynaptic nicotinic receptors in skeletal muscle cells?
- Adrenergic receptors
- Metabotropic receptors
- Muscarinic receptors
- Ion channels (correct)
______ is the neurotransmitter at the adrenal medulla.
______ is the neurotransmitter at the adrenal medulla.
Epinephrine
ACh is a neurotransmitter of parasympathetic and somatic nerves.
ACh is a neurotransmitter of parasympathetic and somatic nerves.
Match the following categories of drugs affecting ANS with their definitions:
Match the following categories of drugs affecting ANS with their definitions:
Dry-powder inhalers (DPIs) include ____________ & ____________.
Dry-powder inhalers (DPIs) include ____________ & ____________.
When 2 or more puffs are needed, inform the patient that at least _____________ should be allowed between puffs.
When 2 or more puffs are needed, inform the patient that at least _____________ should be allowed between puffs.
Inform the patient that salmeterol and formoterol, and oral β-2 agonists should be taken on a _________________, not on a prn basis.
Inform the patient that salmeterol and formoterol, and oral β-2 agonists should be taken on a _________________, not on a prn basis.
What is one of the adverse effects of Bronchodilators?
What is one of the adverse effects of Bronchodilators?
Leukotriene receptor antagonists help prevent acute asthma attacks induced by allergens.
Leukotriene receptor antagonists help prevent acute asthma attacks induced by allergens.
What is a nursing alert regarding the use of topical nasal decongestants?
What is a nursing alert regarding the use of topical nasal decongestants?
What is the recommended maximum duration for the use of topical nasal decongestants?
What is the recommended maximum duration for the use of topical nasal decongestants?
Intranasal corticosteroids are most effective for the treatment of ______________ and ______________ rhinitis.
Intranasal corticosteroids are most effective for the treatment of ______________ and ______________ rhinitis.
Match the following drugs with their formulations and dosages:
Match the following drugs with their formulations and dosages:
Bronchodilator medications are crucial for symptom management in asthma and COPD.
Bronchodilator medications are crucial for symptom management in asthma and COPD.
Flashcards are hidden until you start studying
Study Notes
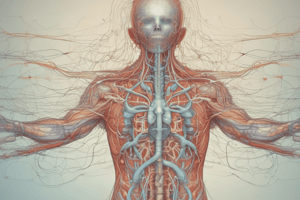
Autonomic Nervous System (ANS)
- ANS transmits signals from CNS to effector organs through two types of efferent neurons
- Divided into sympathetic and parasympathetic nervous systems
- Regulates bodily functions without conscious participation of the mind
Sympathetic Nervous System
- Prepares the body for "fight or flight" response
- Increases heart rate, blood pressure, and energy levels
- Releases epinephrine (adrenaline) and norepinephrine into the bloodstream
Parasympathetic Nervous System
- Regulates involuntary actions, such as digestion and heart rate
- Releases acetylcholine, which slows down heart rate and promotes digestion
Neurotransmitters
- Acetylcholine: released by parasympathetic nerves, slows down heart rate, and promotes digestion
- Norepinephrine: released by sympathetic nerves, increases heart rate and blood pressure
- Epinephrine (adrenaline): released by sympathetic nerves, prepares the body for "fight or flight" response
Cholinergic and Adrenergic Receptors
- Cholinergic receptors:
- Muscarinic receptors: found in smooth muscle, glands, and the CNS
- Nicotinic receptors: found in the CNS and the autonomic ganglia
- Adrenergic receptors:
- Alpha receptors: found in smooth muscle, increase blood pressure
- Beta receptors: found in the heart, increase heart rate and contraction force
ANS Drugs
- Cholinergic agonists: mimic the action of acetylcholine, used to treat glaucoma and urinary retention
- Cholinergic antagonists: block the action of acetylcholine, used to treat glaucoma and urinary retention
- Adrenergic agonists: mimic the action of epinephrine and norepinephrine, used to treat hypotension and asthma
- Adrenergic antagonists: block the action of epinephrine and norepinephrine, used to treat hypertension and anxiety
Cardiovascular System
- Blood pressure regulation:
- Short-term regulation: mediated by the autonomic nervous system
- Long-term regulation: mediated by the kidneys and renin-angiotensin-aldosterone system
- Hypertension:
- Defined as a sustained systolic blood pressure of >140 mmHg or diastolic blood pressure of >90 mmHg
- Causes: genetics, obesity, lack of physical activity, high-sodium diet, stress
- Heart failure:
- Defined as the inability of the heart to pump enough blood to meet the body's needs
- Causes: hypertension, coronary artery disease, cardiomyopathy
Diuretic Agents
- Diuretics:
- Increase urine production and excretion of sodium and water
- Used to treat hypertension, heart failure, and edema
- Types of diuretics:
- Thiazide diuretics: inhibit sodium reabsorption in the distal tubule
- Loop diuretics: inhibit sodium reabsorption in the loop of Henle
- Potassium-sparing diuretics: inhibit aldosterone production
- Carbonic anhydrase inhibitors: inhibit the production of bicarbonate and hydrogen ions
Respiratory System
- Asthma:
- Defined as a chronic inflammatory disorder of the airways
- Characterized by recurring episodes of wheezing, coughing, and shortness of breath
- Treatment of asthma:
- Bronchodilators: relieve bronchospasm and improve lung function
- Corticosteroids: reduce inflammation and airway constriction
- Mast cell stabilizers: prevent mast cell degranulation and allergic reactions
- Leukotriene modifiers: inhibit the production of leukotrienes and reduce airway constriction
Antihistamines
-
Used to treat allergic reactions, including itching, hives, and nasal congestion
-
Classified into two generations:
- First-generation antihistamines: sedating and have anticholinergic effects
- Second-generation antihistamines: non-sedating and selective for peripheral H1 receptors### Cough Preparations
-
There are three classes of cough preparations: Antitussives, Expectorants, and Mucolytics
-
Antitussives suppress coughs, some acting within the CNS and some peripherally, indicated for dry, hacking, nonproductive coughs that interfere with rest and sleep
-
Examples of antitussives include codeine phosphate, pholcodine, dextromethorphan, and diphenhydramine
-
Adverse effects of antitussives include drowsiness, respiratory depression, and constipation
-
Preparations containing codeine or similar analgesics are not recommended in children and should be avoided altogether in those under 1 year of age
Expectorants
- Expectorants render the cough more productive by stimulating the flow of respiratory tract secretions
- Guaifenesin is commonly used alone and as an ingredient in many combination cough and cold remedies
- Dosage of guaifenesin includes 10-20ml three to four times daily PO
Mucolytics
- Mucolytics react directly with mucus to make it more watery, making the cough more productive
- Examples of mucolytics include acetylcysteine, bromhexine, and carbocisteine
Nasal Decongestants
- Sympathomimetics are used to reduce nasal congestion by stimulating alpha1-adrenergic receptors on nasal blood vessels, causing vasoconstriction and shrinkage of swollen membranes
- Topical administration results in rapid and intense response, while oral administration results in delayed, moderate, and prolonged response
- Examples of nasal decongestants include oxymetazoline, phenylephrine, and xylometazoline
- Adverse effects of nasal decongestants include rebound congestion, CNS stimulation, and vasoconstriction
Intranasal Corticosteroids
- Intranasal corticosteroids are effective for treating seasonal and perennial rhinitis, with anti-inflammatory actions that can prevent or suppress all major symptoms of allergic rhinitis
- Examples of intranasal corticosteroids include beclomethasone dipropionate
Asthma and COPD
- Asthma is characterized by eosinophilic inflammation, while COPD is characterized by neutrophilic inflammation
- COPD can coexist with asthma, and distinguishing between the two can be difficult
- Goals of COPD management include relieving symptoms, preventing disease progression, improving exercise tolerance, and improving health status
Pharmacotherapy for COPD
- Bronchodilators are central to symptom management in COPD, with inhaled therapy preferred
- The choice of bronchodilator depends on availability, individual response, and side effects
- Combining bronchodilators may improve efficacy and decrease side effects
Corticosteroids in COPD Management
- Oral and inhaled corticosteroids have limited roles in COPD management, with oral corticosteroids used to identify patients who may benefit from long-term treatment
- Inhaled corticosteroids are effective in reducing exacerbations and improving health status when combined with a long-acting beta agonist
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.