Podcast
Questions and Answers
What is the primary goal of asthma treatment?
What is the primary goal of asthma treatment?
- Increase mucus production
- Reduce overall lung capacity
- Narrow the airways
- Improve airflow (correct)
Which medication is typically used in Step 1 for quick relief during an asthma attack?
Which medication is typically used in Step 1 for quick relief during an asthma attack?
- Long-acting muscarinic antagonist
- Low-dose corticosteroid inhaler
- Leukotriene receptor antagonist
- Short-acting B2 agonist (correct)
What is the purpose of adding a leukotriene receptor antagonist in asthma treatment?
What is the purpose of adding a leukotriene receptor antagonist in asthma treatment?
- To enhance mucus production
- To reduce inflammation (correct)
- To replace corticosteroids
- To increase airway tightening
What role does theophylline play in asthma treatment?
What role does theophylline play in asthma treatment?
Which receptors does adrenaline primarily activate to achieve bronchodilation?
Which receptors does adrenaline primarily activate to achieve bronchodilation?
What characterizes Step 5 in the management of severe asthma?
What characterizes Step 5 in the management of severe asthma?
What is the function of long-acting muscarinic antagonists in asthma therapy?
What is the function of long-acting muscarinic antagonists in asthma therapy?
What is the primary mechanism by which ACE inhibitors lower blood pressure?
What is the primary mechanism by which ACE inhibitors lower blood pressure?
Which of the following medications is considered a thiazide diuretic?
Which of the following medications is considered a thiazide diuretic?
What differentiates Angiotensin Receptor Blockers (ARBs) from ACE inhibitors in terms of side effects?
What differentiates Angiotensin Receptor Blockers (ARBs) from ACE inhibitors in terms of side effects?
What is the role of beta blockers in the treatment of hypertension?
What is the role of beta blockers in the treatment of hypertension?
Which of the following statements about potassium-sparing diuretics is true?
Which of the following statements about potassium-sparing diuretics is true?
What primarily causes the inside of the cardiac myocyte to become more negative during repolarization?
What primarily causes the inside of the cardiac myocyte to become more negative during repolarization?
Which phase of the cardiac nodal action potential is characterized by pacemaker depolarization occurring without a stable resting state?
Which phase of the cardiac nodal action potential is characterized by pacemaker depolarization occurring without a stable resting state?
Which receptor type is involved in increasing the heart rate through sympathetic stimulation?
Which receptor type is involved in increasing the heart rate through sympathetic stimulation?
What term describes the property of heart cells to generate spontaneous action potentials?
What term describes the property of heart cells to generate spontaneous action potentials?
What causes tachycardias according to the information provided?
What causes tachycardias according to the information provided?
During which phase does potassium leave the cell, helping to prepare the cell for the next action potential?
During which phase does potassium leave the cell, helping to prepare the cell for the next action potential?
Which of the following mechanisms slows down the pacemaker potential, leading to a slower heart rate?
Which of the following mechanisms slows down the pacemaker potential, leading to a slower heart rate?
What is the mechanism by which re-entry tachycardia occurs?
What is the mechanism by which re-entry tachycardia occurs?
What defines the resting phase of a cardiac myocyte?
What defines the resting phase of a cardiac myocyte?
What is the primary function of angiotensin converting enzyme (ACE)?
What is the primary function of angiotensin converting enzyme (ACE)?
How does angiotensin 2 primarily increase blood pressure?
How does angiotensin 2 primarily increase blood pressure?
What role do AT1 receptors play in fluid balance?
What role do AT1 receptors play in fluid balance?
What effect does the activation of AT1 receptors have on the sympathetic nervous system?
What effect does the activation of AT1 receptors have on the sympathetic nervous system?
What is a key feedback mechanism involved in regulating renin secretion?
What is a key feedback mechanism involved in regulating renin secretion?
What physiological action does aldosterone have following its release?
What physiological action does aldosterone have following its release?
In which part of the body does the angiotensin converting enzyme primarily act?
In which part of the body does the angiotensin converting enzyme primarily act?
What hormone is promoted by the activation of angiotensin 2 in the hypothalamus?
What hormone is promoted by the activation of angiotensin 2 in the hypothalamus?
Which of the following is NOT a result of angiotensin 2 action?
Which of the following is NOT a result of angiotensin 2 action?
What effect do calcium channel blockers have on heart rhythms?
What effect do calcium channel blockers have on heart rhythms?
Which type of β-blockers primarily targets the heart?
Which type of β-blockers primarily targets the heart?
What is a common side effect of β-blockers on blood pressure?
What is a common side effect of β-blockers on blood pressure?
Which of the following drugs has class III effects on heart repolarization?
Which of the following drugs has class III effects on heart repolarization?
How do non-selective β-blockers affect asthma symptoms?
How do non-selective β-blockers affect asthma symptoms?
What is one of the main uses of β-blockers after a heart attack?
What is one of the main uses of β-blockers after a heart attack?
What impact do β-blockers have on action potentials in nodal tissues?
What impact do β-blockers have on action potentials in nodal tissues?
Which condition can β-blockers help control in patients?
Which condition can β-blockers help control in patients?
What condition is Sotalol used cautiously for due to the risk of Torsades de Pointes?
What condition is Sotalol used cautiously for due to the risk of Torsades de Pointes?
What negative effect do β-blockers have on heart contractions?
What negative effect do β-blockers have on heart contractions?
Flashcards
Asthma Treatment Goal
Asthma Treatment Goal
Improve airflow, measured by PEF (Peak Expiratory Flow).
Bronchodilation
Bronchodilation
Relaxation of smooth muscles around bronchioles, widening airways and improving airflow.
Anti-inflammatory Therapy
Anti-inflammatory Therapy
Reduces inflammation causing airway thickening, edema, and mucus production, preventing narrowing.
Step 1 Asthma Treatment
Step 1 Asthma Treatment
Signup and view all the flashcards
Step 2 Asthma Treatment
Step 2 Asthma Treatment
Signup and view all the flashcards
Step 3 Asthma Treatment
Step 3 Asthma Treatment
Signup and view all the flashcards
Adrenaline's effect on bronchioles
Adrenaline's effect on bronchioles
Signup and view all the flashcards
Repolarization
Repolarization
Signup and view all the flashcards
Sodium-Potassium Pump
Sodium-Potassium Pump
Signup and view all the flashcards
Cardiac Nodal Action Potential
Cardiac Nodal Action Potential
Signup and view all the flashcards
Depolarization (Cardiac Nodal Cells)
Depolarization (Cardiac Nodal Cells)
Signup and view all the flashcards
Sympathetic Stimulation
Sympathetic Stimulation
Signup and view all the flashcards
Vagal (Parasympathetic) Stimulation
Vagal (Parasympathetic) Stimulation
Signup and view all the flashcards
Chronotropic Effect
Chronotropic Effect
Signup and view all the flashcards
Inotropic Effect
Inotropic Effect
Signup and view all the flashcards
Automaticity (Heart Cells)
Automaticity (Heart Cells)
Signup and view all the flashcards
Angiotensin 1 Conversion
Angiotensin 1 Conversion
Signup and view all the flashcards
Angiotensin 2's Role
Angiotensin 2's Role
Signup and view all the flashcards
AT1 Receptors
AT1 Receptors
Signup and view all the flashcards
Vasoconstriction (Angiotensin 2)
Vasoconstriction (Angiotensin 2)
Signup and view all the flashcards
Aldosterone Secretion (Angiotensin 2)
Aldosterone Secretion (Angiotensin 2)
Signup and view all the flashcards
Sympathetic Nervous System Activation (Angiotensin 2)
Sympathetic Nervous System Activation (Angiotensin 2)
Signup and view all the flashcards
Antidiuretic Hormone (ADH) Release (Angiotensin 2)
Antidiuretic Hormone (ADH) Release (Angiotensin 2)
Signup and view all the flashcards
Negative Feedback Regulation (Angiotensin)
Negative Feedback Regulation (Angiotensin)
Signup and view all the flashcards
Class IV Antiarrhythmics
Class IV Antiarrhythmics
Signup and view all the flashcards
β-blockers effect on heart rate
β-blockers effect on heart rate
Signup and view all the flashcards
β1-selective β-blockers
β1-selective β-blockers
Signup and view all the flashcards
Non-selective β-blockers
Non-selective β-blockers
Signup and view all the flashcards
Sotalol's special effect
Sotalol's special effect
Signup and view all the flashcards
β-blockers and action potentials
β-blockers and action potentials
Signup and view all the flashcards
β-blockers' effect on heart contractions
β-blockers' effect on heart contractions
Signup and view all the flashcards
β-blockers' effect on blood vessels
β-blockers' effect on blood vessels
Signup and view all the flashcards
β-blockers and asthma
β-blockers and asthma
Signup and view all the flashcards
Sotalol's potential risk
Sotalol's potential risk
Signup and view all the flashcards
ACE Inhibitors: How they work
ACE Inhibitors: How they work
Signup and view all the flashcards
ACE Inhibitors: Side Effects
ACE Inhibitors: Side Effects
Signup and view all the flashcards
Beta Blockers: Action in the Heart
Beta Blockers: Action in the Heart
Signup and view all the flashcards
Diuretics: Types and Actions
Diuretics: Types and Actions
Signup and view all the flashcards
Thiazide Diuretics: Mechanism
Thiazide Diuretics: Mechanism
Signup and view all the flashcards
Study Notes
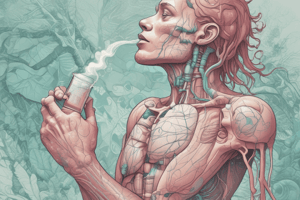
Drugs and Asthma
- Asthma treatment focuses on bronchioles to improve airflow, measured by peak expiratory flow (PEF).
- Treatment aims at bronchodilation (relaxing airway muscles) and anti-inflammation (reducing airway thickening, edema, and mucus).
Drug Treatment of Asthma
- Step 1: Intermittent Reliever Therapy: Short-acting beta-2 agonists (SABAs) like salbutamol are used to quickly relax airway muscles during asthma attacks.
- Step 2: Regular Preventer Therapy: Low-dose corticosteroids via inhaler are used daily to prevent future asthma symptoms by reducing inflammation.
- Step 3: Initial Add-In Therapy: Oral leukotriene receptor antagonists like montelukast are added if symptoms persist to reduce inflammation further.
- Step 4: Additional Controller Therapy: Long-acting beta-2 agonists (LABAs) and/or long-acting muscarinic antagonists (LAMAs) are used with or instead of inhaled corticosteroids to provide sustained bronchodilation and prevent airway tightening. Theophylline is another option.
- Step 5: Continuous Oral Corticosteroids: Used for severe, uncontrolled asthma for long-term control. Monoclonal antibodies (targeting anti-IgE or anti-IL5) are sometimes used for severe asthma.
SABA Drugs (Salbutamol, Terbutaline)
- Modified from adrenaline, targeting beta-2 receptors solely for bronchodilation, avoiding cardiac side effects.
- They last longer than adrenaline due to improved chemical structure, providing better relief.
- They activate G proteins, boosting cAMP levels, leading to smooth muscle relaxation and reduced intracellular calcium for bronchodilation.
Adverse Effects of Salbutamol
- Tachycardia (fast heart rate)
- Muscle tremors
- Hypokalemia (low potassium)
- Tolerance (decreased effectiveness over time due to downregulation of beta-2 receptors).
- Tolerance can be affected by genetic polymorphisms (variations in Beta-2 receptor genes).
Regular Preventer Therapy
- Corticosteroids, similar to cortisol, used via inhaler to reduce inflammation and suppress the immune system.
- Examples: Beclometasone, Fluticasone, Budesonide.
- Low-dose administration minimizes the risk of fungal infections (oral thrush).
Initial Add-In Therapy
- Leukotriene Receptor Antagonists (e.g., montelukast) block inflammatory chemicals and reduce inflammation.
- These are oral medications.
Additional Controller Therapy
- Long-acting beta-2 agonists (LABAs) and long-acting muscarinic antagonists (LAMAs) are used for ongoing bronchial relaxation.
- Theophylline can also be taken for airway relaxation.
Continuous Steroid Therapies
- Oral corticosteroids like prednisolone are used when asthma remains uncontrolled.
- They reduce inflammation and control the immune response. Can cause adrenal suppression, which needs to be managed carefully.
- There are monoclonal antibodies which target immune cells, used in severe cases to control inflammation.
Arrhythmias
- Cardiac synctium: network of interconnected cells with gap junctions facilitating rapid action potential spreading.
- Cardiac myocyte action potential has 4 phases (depolarization, partial repolarization, plateau, repolarization, rest) triggered by sodium, potassium, and calcium ions.
- Pacemaker cells (e.g., sinoatrial (SA) and atrioventricular (AV) nodes) continuously depolarize, initiating action potentials.
- Sympathetic stimulation (β1/β2 adrenergic receptors) increases heart rate, while parasympathetic stimulation (muscarinic acetylcholine receptors) slows it down.
- Common causes of tachycardias include rapid action potentials, re-entry (looping signals), or ectopic pacemaker activity.
- There are many types and classifications of arrhythmias that can be treated with different medicines.
Adverse Effects of Drugs
- Potential side effects like tachycardia, hypokalemia, and tremor.
- Important considerations for patients with cardiovascular issues to avoid potential adverse effects.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.