Podcast
Questions and Answers
[Blank] are commonly called water pills and promote diuresis, leading to increased urine production.
[Blank] are commonly called water pills and promote diuresis, leading to increased urine production.
Diuretics
[Blank] characterized by increased intraocular pressure (IOP), which is the pressure inside the eyes.
[Blank] characterized by increased intraocular pressure (IOP), which is the pressure inside the eyes.
Glaucoma
[Blank] diuretics act on the thick ascending loop of Henle to inhibit chloride transport of sodium into the circulation and inhibit passive reabsorption of sodium
[Blank] diuretics act on the thick ascending loop of Henle to inhibit chloride transport of sodium into the circulation and inhibit passive reabsorption of sodium
Loop
The carbonic anhydrase inhibitors acetazolamide and methazolamide block the action of the enzyme ______, which is needed to maintain the body's acid-base balance.
The carbonic anhydrase inhibitors acetazolamide and methazolamide block the action of the enzyme ______, which is needed to maintain the body's acid-base balance.
[Blank] diuretics are weaker than thiazides and loop diuretics, or in combination with another diuretic such as hydrochlorothiazide or an antihypertensive drug.
[Blank] diuretics are weaker than thiazides and loop diuretics, or in combination with another diuretic such as hydrochlorothiazide or an antihypertensive drug.
[Blank] is a mineralocorticoid hormone that promotes sodium retention and potassium excretion.
[Blank] is a mineralocorticoid hormone that promotes sodium retention and potassium excretion.
[Blank] is the stop of natural blood loss when an injury occurs.
[Blank] is the stop of natural blood loss when an injury occurs.
[Blank] is a substance that inactivates thrombin, is synthesized in the liver, and circulates in plasma.
[Blank] is a substance that inactivates thrombin, is synthesized in the liver, and circulates in plasma.
[Blank] laboratory tests used to detect deficiencies of certain clotting factors & these tests are used to monitor heparin therapy
[Blank] laboratory tests used to detect deficiencies of certain clotting factors & these tests are used to monitor heparin therapy
[Blank] is the process or a form of treatment with a primary goal of the dissolving blood clots that cause obstruction
[Blank] is the process or a form of treatment with a primary goal of the dissolving blood clots that cause obstruction
Flashcards
Diuretics
Diuretics
Drugs that promote diuresis, which results in increased urine production.
Hypertension
Hypertension
Persistent higher-than-normal blood pressure. Diuretics are used to reduce blood pressure.
Glaucoma
Glaucoma
An eye disease characterized by increased pressure inside the eyes.
Loop diuretics
Loop diuretics
Signup and view all the flashcards
Osmotic diuretics
Osmotic diuretics
Signup and view all the flashcards
Hemostasis
Hemostasis
Signup and view all the flashcards
Anticoagulation
Anticoagulation
Signup and view all the flashcards
Antithrombin III
Antithrombin III
Signup and view all the flashcards
International Normalized Ratio (INR)
International Normalized Ratio (INR)
Signup and view all the flashcards
Thrombolysis
Thrombolysis
Signup and view all the flashcards
Study Notes
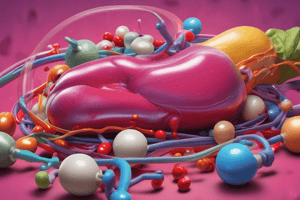
Module 7: Diuretics
- Diuretics, commonly known as water pills, are drugs that increase urine production.
Disease Spotlight
- Edema is the accumulation of fluid in the interstitial spaces.
- Typically seen in patients with heart failure, cirrhosis, other liver diseases, and renal diseases
- Hypertension is persistently high blood pressure, often with no known cause (idiopathic).
- Diuretics manage hypertension by reducing blood volume and sodium.
- Glaucoma is an eye disease characterized by increased intraocular pressure (IOP).
5 Categories of Diuretics
Thiazide and Thiazide-Like Diuretics
- Used to treat hypertension and peripheral edema.
- Not effective for immediate diuresis.
- Primarily for patients with normal renal function.
- Cause loss of sodium, potassium, and magnesium, but promote calcium reabsorption.
Benzothiadiazides
- Commonly called thiazides, they have been a useful class of diuretics and antihypertensive agents since the 1960s.
Chlorothiazide
- The first thiazide, marketed in 1957.
- Hydrochlorothiazide followed a year later.
Loop or High-Ceiling Diuretics
- Act on the thick ascending loop of Henle.
- Inhibit chloride transport of sodium into the circulation.
- Inhibit passive reabsorption of sodium.
- Resulting in the loss of sodium and water, along with potassium, calcium, and magnesium.
- Ethacrynic Acid was the first marketed loop diuretic.
- Followed by furosemide and then bumetanide (more potent than furosemide).
- Their high diuretic potential earns them the name "high ceiling diuretics" or "potassium-wasting diuretics."
- Bumetanide, furosemide, and torsemide are used for edema from heart failure, liver cirrhosis, renal disease, and nephrotic syndrome.
- The primary outcome of sulfonamide loop diuretic therapy is diuresis.
Osmotic Diuretics
- Increase osmolality (concentration) and sodium reabsorption in the proximal tubule and loop of Henle.
- Used to prevent kidney failure, decrease intracranial pressure (ICP), and decrease intraocular pressure (IOP).
Mannitol
- Most frequently prescribed osmotic diuretic, followed by urea.
- Used with cisplatin and carboplatin in cancer chemotherapy to induce diuresis and decrease side effects.
- Mannitol is a sugar that is not well absorbed by the tubules and acts to increase urine production.
Carbonic Anhydrase Inhibitors
- Acetazolamide and methazolamide block carbonic anhydrase.
- Carbonic anhydrase is an enzyme needed to maintain the body's acid-base balance.
Acetazolamide
- A weak diuretic that inhibits carbonic anhydrase in the kidneys, brain, and eyes.
Potassium-Sparing Diuretics
- Weaker than thiazides and loop diuretics.
- Can be used in combination with hydrochlorothiazide or an antihypertensive drug.
Spironolactone
- Aldosterone antagonist discovered in 1958.
- It was the first potassium-sparing diuretic.
Aldosterone
- It is a mineralocorticoid hormone.
- Promotes sodium retention and potassium excretion.
Module 8: Hemostasis
- Hemostasis is the process that stops blood loss when an injury occurs and involves 3 steps.
Vascular Spasm
- Smooth muscle in blood vessel walls contracts immediately when injured, reducing blood loss.
Platelet Plug Formation
- Platelets that encounter damaged blood vessels form a "platelet plug" to close the gap.
- Key stages include platelet adhesion, platelet release reaction, and platelet aggregation.
Blood Clotting (Coagulation)
- Blood remains liquid inside vessels but thickens and coagulates (gel-like) when injury occurs.
- Anticoagulation slows down the blood clotting to prevent the formation of blood clots.
- Anticoagulant agents slow down or prevent formation of blood clots.
Anticoagulants
- Prevent blood clotting in patients with thrombophlebitis, pulmonary embolism, & embolism.
- Heparin & warfarin prevent thrombosis in the veins
Types of Heparin
- Regular or Unfractionated Heparin
- LMWHS (low molecular weight heparin)/fractionated
Antithrombin III
- Is a substance that inactivates thrombin.
- synthesized in the liver and circulates in plasma
Heparin Antagonist
- Suspends the effect of heparin.
- Protamine sulfate (10mg for 1000 unit of heparin)
Partial Thromboplastin Time -PTT/Activated Partial Thromboplastin Time - aPTT
- Laboratory tests detect deficiencies of certain clotting factors.
- Tests used to monitor heparin therapy.
Thrombocytopenia/Bleeding Complications
- Excessive bleeding managed by administering protamine sulfate to reverse heparin.
Warfarin (Coumadin)
- Warfarin is absorbed rapidly and almost completely when taken orally.
- Dicoumarol and Anisindone are also anticoagulants.
International Normalized Ratio (INR)
- Is the laboratory test frequently used to report PT results
Antidote for Warfarin
- Vitamin K or phytonadione
- Direct thrombin inhibitors are a new class of anticoagulants that bind directly to thrombin and block its interaction with its substrates.
Antiplatelet Drugs
- Used to prevent thrombosis in the arteries that suppresses platelet aggregation
- These drugs decrease the formation of the platelet plug by decreasing the responsiveness of the platelets
COX Inhibitors: Aspirin
- Inhibits cyclooxygenase, the enzyme platelets need to synthesize thromboxane.
- Has prolonged antiplatelet activity.
Adenosine Diphosphate (ADP) Antagonists
- Clopidogrel
- Dipyridamole
Thrombolytics
- Thrombolysis is a treatment with the goal of dissolving blood clots that cause obstruction.
- Thrombolytics are used to dissolve clots, improve blood flow, and prevent damage to tissues and organs.
- Thrombolytics activate the natural anti-clotting fibrinolytic mechanism to convert plasminogen to plasmin.
- Destroys and breaks down the fibrin threads in the blood clot (FIBRINOLYSIS)
- Thromboembolism is the occlusion of an artery or vein caused by thrombus or embolus, resulting in ischemia (deficient blood flow) that causes necrosis
Common Thrombolytics
- Tissue plasminogen activator (t-PA) or alteplase, Steptokinase, Urokinase, Anistreplase, Reteplase, and Tenecteplase
Alteplase
- Also known as tissue plasminogen activator (tPA) & tenecteplase (TNK tPA)
Streptokinase
- Obtained from B haemolytic streptococci group C
- Non-intrinsic enzyme activity
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.