Podcast
Questions and Answers
What is the primary therapeutic use of acetazolamide in the context of glaucoma?
What is the primary therapeutic use of acetazolamide in the context of glaucoma?
- Decreases intraocular pressure (correct)
- Increases aqueous humor production
- Enhances systemic circulation
- Promotes sodium retention
What condition can acetazolamide help prevent symptoms of?
What condition can acetazolamide help prevent symptoms of?
- Altitude sickness (correct)
- Circulatory shock
- Acute renal failure
- Chronic kidney disease
Which pharmacokinetic property is NOT true for mannitol?
Which pharmacokinetic property is NOT true for mannitol?
- It undergoes little or no reabsorption.
- It should be administered intravenously.
- It is absorbed when given orally. (correct)
- It has osmotic effects in the systemic circulation.
Which adverse effect is associated with carbonic anhydrase inhibitors like acetazolamide?
Which adverse effect is associated with carbonic anhydrase inhibitors like acetazolamide?
What is the main mechanism of action of mannitol as an osmotic diuretic?
What is the main mechanism of action of mannitol as an osmotic diuretic?
What is the primary action of diuretics in the kidneys?
What is the primary action of diuretics in the kidneys?
Which type of diuretic is commonly used for managing hypertension?
Which type of diuretic is commonly used for managing hypertension?
What percentage of filtered Na+ and water is reabsorbed in the proximal convoluted tubule?
What percentage of filtered Na+ and water is reabsorbed in the proximal convoluted tubule?
Why do diuretics that act in the proximal convoluted tubule exhibit weak diuretic properties?
Why do diuretics that act in the proximal convoluted tubule exhibit weak diuretic properties?
What phenomenon occurs in the descending loop of Henle that causes an increase in osmolarity?
What phenomenon occurs in the descending loop of Henle that causes an increase in osmolarity?
Which ions are actively reabsorbed in the ascending loop of Henle?
Which ions are actively reabsorbed in the ascending loop of Henle?
How do osmotic diuretics exert part of their action in the kidney?
How do osmotic diuretics exert part of their action in the kidney?
Which effect do diuretics commonly have on urine composition?
Which effect do diuretics commonly have on urine composition?
What is the primary function of thiazide diuretics in the distal convoluted tubule?
What is the primary function of thiazide diuretics in the distal convoluted tubule?
Which statement about loop diuretics is correct?
Which statement about loop diuretics is correct?
What percentage of filtered sodium chloride is reabsorbed in the distal convoluted tubule?
What percentage of filtered sodium chloride is reabsorbed in the distal convoluted tubule?
How do thiazides affect urinary calcium excretion?
How do thiazides affect urinary calcium excretion?
What mediates calcium reabsorption in the distal convoluted tubule?
What mediates calcium reabsorption in the distal convoluted tubule?
What impact does renal function have on the effectiveness of thiazide diuretics?
What impact does renal function have on the effectiveness of thiazide diuretics?
What hormones influence sodium reabsorption in the collecting tubule?
What hormones influence sodium reabsorption in the collecting tubule?
What is one of the primary uses of thiazides in clinical settings?
What is one of the primary uses of thiazides in clinical settings?
Which condition is primarily treated with high doses of spironolactone due to secondary hyperaldosteronism?
Which condition is primarily treated with high doses of spironolactone due to secondary hyperaldosteronism?
What is the primary function of administering potassium-sparing diuretics in conjunction with thiazide or loop diuretics?
What is the primary function of administering potassium-sparing diuretics in conjunction with thiazide or loop diuretics?
Which adverse effect is commonly associated with spironolactone but not with eplerenone?
Which adverse effect is commonly associated with spironolactone but not with eplerenone?
What mechanism do triamterene and amiloride utilize to achieve potassium-sparing effects?
What mechanism do triamterene and amiloride utilize to achieve potassium-sparing effects?
Which diuretic class is less efficacious and mainly used for their pharmacologic actions, rather than diuretic effect?
Which diuretic class is less efficacious and mainly used for their pharmacologic actions, rather than diuretic effect?
What occurs as a direct effect of acetazolamide inhibiting carbonic anhydrase?
What occurs as a direct effect of acetazolamide inhibiting carbonic anhydrase?
What is a notable consequence of the loss of bicarbonate (HCO3-) in patients treated with acetazolamide?
What is a notable consequence of the loss of bicarbonate (HCO3-) in patients treated with acetazolamide?
Which condition can be treated with lower doses of spironolactone to prevent myocardial remodeling?
Which condition can be treated with lower doses of spironolactone to prevent myocardial remodeling?
What is the primary mechanism by which loop diuretics produce diuresis?
What is the primary mechanism by which loop diuretics produce diuresis?
Which adverse effect is commonly associated with thiazide diuretics?
Which adverse effect is commonly associated with thiazide diuretics?
Loop diuretics do NOT typically cause which of the following?
Loop diuretics do NOT typically cause which of the following?
Which therapeutic use is NOT indicated for loop diuretics?
Which therapeutic use is NOT indicated for loop diuretics?
What is a significant impact of loop diuretics on potassium levels?
What is a significant impact of loop diuretics on potassium levels?
Which of the following statements about thiazide diuretics is incorrect?
Which of the following statements about thiazide diuretics is incorrect?
What effect does loop diuretics have on renal hemodynamics?
What effect does loop diuretics have on renal hemodynamics?
In patients with poor renal function, what is a characteristic of loop diuretics?
In patients with poor renal function, what is a characteristic of loop diuretics?
Flashcards are hidden until you start studying
Study Notes
Diuretics Overview
- Diuretics are medications that increase urine production by preventing sodium (Na+) reabsorption in the kidneys.
- Diuretics are utilized for managing conditions like edema, hypertension, glaucoma, and heart failure.
- They can alter the urine's pH and ionic composition, as well as that of blood.
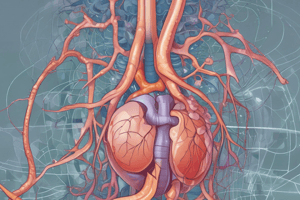
Nephron Structure and Function
- Proximal Convoluted Tubule: Reabsorbs 65% of filtered Na+ and about 60% of water; diuretics here have limited effectiveness due to subsequent reabsorption in the Loop of Henle.
- Descending Loop of Henle: Water is reabsorbed, increasing the osmolarity of tubular fluid; osmotic diuretics exert effects in this area.
- Ascending Loop of Henle: Impermeable to water; reabsorbs approximately 25% to 30% of filtered Na+, K+, and Cl-; loop diuretics are particularly effective here.
- Distal Convoluted Tubule: Reabsorbs 5% to 10% of NaCl; target for thiazide diuretics.
- Collecting Tubule and Duct: Involves Na+ reabsorption affected by aldosterone and antidiuretic hormone (ADH).
Diuretic Classes
-
Thiazides
- Common diuretics used for hypertension and fluid retention.
- Mechanism: Inhibit Na+/Cl- cotransporter in the distal convoluted tubule.
- Actions include increased Na+ and Cl- excretion, reduced urinary calcium, and lowered peripheral vascular resistance.
- Adverse effects: Hypokalemia, hyponatremia, hyperuricemia, and hypovolemia.
-
Loop Diuretics
- Examples: Bumetanide, Furosemide, Torsemide, Ethacrynic Acid.
- Most potent diuretics, effective in renal impairment situations.
- Mechanism: Block Na+/K+/2Cl- cotransporter in the ascending loop.
- Indications: Edema, heart failure, resistant hypertension, polycystic ovary syndrome.
-
Potassium-Sparing Diuretics
- Includes spironolactone and eplerenone.
- Mechanism: Inhibit aldosterone, leading to reduced Na+ reabsorption and K+ secretion.
- Adverse effects: Hyperkalemia and gynecomastia (primarily with spironolactone).
-
Carbonic Anhydrase Inhibitors
- Example: Acetazolamide.
- Mechanism: Inhibits carbonic anhydrase leading to mild diuresis and increased urinary pH.
- Therapeutic uses: Glaucoma management and altitude sickness prevention.
- Adverse effects: Mild metabolic acidosis and potential renal complications.
-
Osmotic Diuretics
- Example: Mannitol.
- Mechanism: Increases osmolarity of tubular fluid, preventing water reabsorption, but not Na+.
- Indications: Maintenance of urine flow post-acute renal failure and for increased intracranial pressure treatment.
- Pharmacokinetics: Non-absorbed orally; administered intravenously.
Pharmacology Notes
- Diuretics function primarily through their targeted action at specific nephron sites.
- The renal function status critically influences the effectiveness of diuretics, especially thiazides.
- Careful monitoring for electrolyte imbalances and other potential adverse effects is essential in patients on diuretics.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.