Podcast
Questions and Answers
What primary condition leads to mitral stenosis?
What primary condition leads to mitral stenosis?
- Myocardial infarction
- Infective endocarditis
- Rheumatic fever (correct)
- Congenital abnormalities
What is the normal area range of the mitral valve orifice?
What is the normal area range of the mitral valve orifice?
- 1 to 3 cm²
- 2 to 4 cm²
- 4 to 6 cm² (correct)
- 6 to 8 cm²
What complication can arise from atrial fibrillation in mitral stenosis patients?
What complication can arise from atrial fibrillation in mitral stenosis patients?
- Systemic embolization risk (correct)
- Enhanced pulmonary venous return
- Increased left ventricular filling
- Decreased risk of thrombosis
What is the consequence of a mitral valve area below 2.0 cm²?
What is the consequence of a mitral valve area below 2.0 cm²?
What happens to the left atrial pressure in mitral stenosis?
What happens to the left atrial pressure in mitral stenosis?
Which of the following is NOT a complication associated with mitral stenosis?
Which of the following is NOT a complication associated with mitral stenosis?
What results from severe pulmonary hypertension in patients with mitral stenosis?
What results from severe pulmonary hypertension in patients with mitral stenosis?
Which condition is often worsened by tachycardia or atrial fibrillation in mitral stenosis patients?
Which condition is often worsened by tachycardia or atrial fibrillation in mitral stenosis patients?
Which structure is NOT part of the mitral valve apparatus?
Which structure is NOT part of the mitral valve apparatus?
What is a common cause of acute mitral regurgitation (MR)?
What is a common cause of acute mitral regurgitation (MR)?
Acute severe mitral regurgitation can lead to which of the following immediate consequences?
Acute severe mitral regurgitation can lead to which of the following immediate consequences?
Which condition is a potential chronic cause of mitral regurgitation?
Which condition is a potential chronic cause of mitral regurgitation?
What is the primary physiological impact of acute severe mitral regurgitation?
What is the primary physiological impact of acute severe mitral regurgitation?
Which of the following is NOT a contributing factor to chronic mitral regurgitation?
Which of the following is NOT a contributing factor to chronic mitral regurgitation?
What happens to the left atrium during acute severe MR?
What happens to the left atrium during acute severe MR?
Which symptom is most commonly associated with acute pulmonary edema caused by acute MR?
Which symptom is most commonly associated with acute pulmonary edema caused by acute MR?
Which peripheral sign is characterized by abrupt distension and quick collapse on palpation of the peripheral arterial pulse?
Which peripheral sign is characterized by abrupt distension and quick collapse on palpation of the peripheral arterial pulse?
What is the best imaging method to assess the severity and hemodynamic consequences of aortic regurgitation?
What is the best imaging method to assess the severity and hemodynamic consequences of aortic regurgitation?
Which sign is described as visible pulsations of the fingernail bed with light compression?
Which sign is described as visible pulsations of the fingernail bed with light compression?
What sound is described by booming systolic and diastolic sounds auscultated over the femoral artery?
What sound is described by booming systolic and diastolic sounds auscultated over the femoral artery?
What is indicated by a popliteal cuff systolic blood pressure being 40 mmHg higher than the brachial cuff systolic blood pressure?
What is indicated by a popliteal cuff systolic blood pressure being 40 mmHg higher than the brachial cuff systolic blood pressure?
Which of the following electrical changes on an ECG is indicative of aortic regurgitation?
Which of the following electrical changes on an ECG is indicative of aortic regurgitation?
Which clinical finding is NOT associated with chronic aortic valve regurgitation?
Which clinical finding is NOT associated with chronic aortic valve regurgitation?
Which sign reflects vigorous carotid pulsations and is indicative of aortic regurgitation?
Which sign reflects vigorous carotid pulsations and is indicative of aortic regurgitation?
What heart sound may be heard in cases of mitral regurgitation?
What heart sound may be heard in cases of mitral regurgitation?
What type of murmur is typically associated with severe mitral regurgitation?
What type of murmur is typically associated with severe mitral regurgitation?
What finding on an ECG can indicate left atrial enlargement?
What finding on an ECG can indicate left atrial enlargement?
What echocardiographic assessment is crucial in patients with mitral regurgitation?
What echocardiographic assessment is crucial in patients with mitral regurgitation?
Which of the following symptoms is NOT typically associated with chronic mitral regurgitation?
Which of the following symptoms is NOT typically associated with chronic mitral regurgitation?
What is a common first-line medical treatment for patients experiencing pulmonary congestion due to mitral regurgitation?
What is a common first-line medical treatment for patients experiencing pulmonary congestion due to mitral regurgitation?
For males over 40 or females over 50, what is the purpose of cardiac catheterization in the context of mitral regurgitation?
For males over 40 or females over 50, what is the purpose of cardiac catheterization in the context of mitral regurgitation?
What is the recommended long-term prophylaxis for patients with rheumatic heart disease?
What is the recommended long-term prophylaxis for patients with rheumatic heart disease?
What characteristic is NOT typically observed in the pulse of a patient with severe aortic stenosis?
What characteristic is NOT typically observed in the pulse of a patient with severe aortic stenosis?
Which of the following is a common feature noted during the cardiac examination of a patient with aortic stenosis?
Which of the following is a common feature noted during the cardiac examination of a patient with aortic stenosis?
Which diagnostic tool is considered the gold standard in assessing aortic stenosis?
Which diagnostic tool is considered the gold standard in assessing aortic stenosis?
What is the primary purpose of performing a cardiac catheterization in patients with suspected aortic stenosis?
What is the primary purpose of performing a cardiac catheterization in patients with suspected aortic stenosis?
Which of the following management strategies is appropriate for patients with aortic stenosis and existing comorbid conditions?
Which of the following management strategies is appropriate for patients with aortic stenosis and existing comorbid conditions?
Which statement regarding the impact of medical therapy on aortic stenosis is accurate?
Which statement regarding the impact of medical therapy on aortic stenosis is accurate?
Which auscultation finding is associated with aortic stenosis?
Which auscultation finding is associated with aortic stenosis?
What is a classic symptom of aortic stenosis that patients often experience during physical activity?
What is a classic symptom of aortic stenosis that patients often experience during physical activity?
Flashcards are hidden until you start studying
Study Notes
Disorders of the Cardiac Valves
Mitral Valve Disease
-
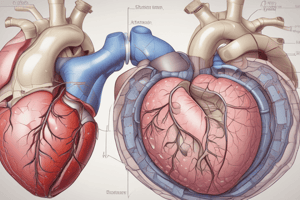
Mitral Valve Anatomy:
- Composed of the mitral annulus, anterior and posterior leaflets, chordae tendineae, and papillary muscles.
- Dysfunction arises from abnormalities in one or more of these structures.
-
Mitral Regurgitation (MR):
- Can be chronic (due to rheumatic fever, ischemic heart disease, cardiomyopathy, etc.) or acute (due to papillary muscle rupture or infective endocarditis).
-
Pathophysiology of Acute MR:
- Results in acute left ventricular (LV) volume overload, leading to increased LV diastolic pressure, pulmonary edema, and signs like S3 heart sound and harsh pan-systolic murmur.
-
Investigations:
- ECG: May show P mitrale or left ventricular hypertrophy.
- Chest X-ray: Reveals left atrial enlargement and possible LV enlargement.
- Echocardiography: Visualizes mitral leaflets, assesses regurgitation severity, LV dimensions, and pulmonary hypertension.
- Cardiac Catheterization: For coronary risk evaluation in older patients.
-
Treatment of MR:
- Acute MR: Requires afterload reduction with vasodilators and diuretics; assisted ventilation may be necessary.
- Chronic MR: Focus on timely surgery before irreversible LV dysfunction develops; medical treatment includes diuretics and anticoagulation for atrial fibrillation.
Aortic Valve Disease
-
Aortic Stenosis (AS):
- Normal mitral valve orifice area is 4-6 cm²; stenosis occurs when the area is below 2.0 cm², causing diastolic pressure gradients and LV filling issues.
-
Pathophysiology of AS:
- Results in increased left atrial pressure and pulmonary venous hypertension, leading to right ventricular dilation and tricuspid regurgitation.
- Tachycardia or atrial fibrillation significantly worsens symptoms due to loss of atrial contraction.
-
Complications of AS:
- Atrial fibrillation (AF) increases pulmonary congestion and embolic risk.
- May lead to pulmonary hypertension, recurrent pulmonary infections, and possible angina-like symptoms.
-
Signs of Aortic Regurgitation:
- Characterized by hyperdynamic pulses and wide pulse pressure.
- Peripheral signs include Water-Hammer pulse, Pistol-shot sign, and visible pulsations in the nail bed (Quincke's sign).
-
Diagnosis of Aortic Regurgitation:
- ECG: Shows signs of left ventricular hypertrophy and left atrial enlargement.
- Chest X-ray: May show cardiomegaly and aortic aneurysm.
- Echocardiography: Gold standard for assessing etiology and severity of aortic regurgitation.
-
Management of Aortic Stenosis:
- No proven medical therapies to modify AS; however, managing comorbidities (like hypertension) is recommended.
- Gradual dose increase of antihypertensive medications is crucial for patients with severe AS.
This summary provides essential insights into mitral and aortic valve diseases, emphasizing their anatomy, pathophysiology, signs, diagnosis, and management strategies.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.