Podcast
Questions and Answers
What are the primary components broken down during digestion?
What are the primary components broken down during digestion?
- Proteins, carbohydrates, and triacylglycerols (correct)
- Carbohydrates, vitamins, and fiber
- Proteins, minerals, and sugars
- Fats, sugars, and carbohydrates
Which type of saliva is primarily secreted by the submaxillary glands?
Which type of saliva is primarily secreted by the submaxillary glands?
- High in protein and acidic
- Low in potassium and isotonic
- Rich in electrolytes and hypotonic (correct)
- Rich in mucin and hypertonic
What is the role of parasympathetic stimulation in salivary secretion?
What is the role of parasympathetic stimulation in salivary secretion?
- Promotes the secretion of mucin-rich saliva
- Increases the release of watery saliva (correct)
- Inhibits the function of acinar cells
- Decreases the viscosity of saliva
What enzymes are found in saliva that aid in digestion?
What enzymes are found in saliva that aid in digestion?
What is one of the minor roles of saliva in the digestive process?
What is one of the minor roles of saliva in the digestive process?
Which enzyme is primarily responsible for the hydrolysis of triacylglycerols at positions 1 and 3?
Which enzyme is primarily responsible for the hydrolysis of triacylglycerols at positions 1 and 3?
Which amylase has a cleavage site at the last α-1,4 glycosidic bond?
Which amylase has a cleavage site at the last α-1,4 glycosidic bond?
What is the optimum pH range for β-amylase activity?
What is the optimum pH range for β-amylase activity?
Lactase activity in most mammals tends to decrease after which life stage?
Lactase activity in most mammals tends to decrease after which life stage?
What role do bile salts play in lipid digestion?
What role do bile salts play in lipid digestion?
What is the primary role of co-lipase in the digestion of lipids?
What is the primary role of co-lipase in the digestion of lipids?
Which statement accurately describes the action of phospholipase A2?
Which statement accurately describes the action of phospholipase A2?
What is one of the functions of bile in lipid digestion?
What is one of the functions of bile in lipid digestion?
How does bile acid contribute to cholesterol homeostasis?
How does bile acid contribute to cholesterol homeostasis?
What characteristic of bile acids allows them to function as detergents?
What characteristic of bile acids allows them to function as detergents?
What mechanism is primarily responsible for the secretion of gastric acid by gastrin?
What mechanism is primarily responsible for the secretion of gastric acid by gastrin?
Which of the following statements about pepsin is correct?
Which of the following statements about pepsin is correct?
What is the role of rennin in the stomach?
What is the role of rennin in the stomach?
What is unique about the intrinsic factor produced by parietal cells?
What is unique about the intrinsic factor produced by parietal cells?
Which statement about gastric lipase is accurate?
Which statement about gastric lipase is accurate?
What effect does carbonic anhydrase have in the gastric secretions process?
What effect does carbonic anhydrase have in the gastric secretions process?
What is the physiological consequence of the alkaline tide after a meal?
What is the physiological consequence of the alkaline tide after a meal?
Which type of digestion occurs primarily in the stomach?
Which type of digestion occurs primarily in the stomach?
What is the primary rate-limiting enzyme in the synthesis of bile acids?
What is the primary rate-limiting enzyme in the synthesis of bile acids?
Which bile acid undergoes bacterial modification in the intestine resulting in secondary bile acids?
Which bile acid undergoes bacterial modification in the intestine resulting in secondary bile acids?
What percentage of secreted bile acids is efficiently reabsorbed in the enterohepatic circulation?
What percentage of secreted bile acids is efficiently reabsorbed in the enterohepatic circulation?
Which two bile acids are classified as primary bile acids?
Which two bile acids are classified as primary bile acids?
Which bile acid is primarily eliminated in the feces and is not reabsorbed due to its solubility?
Which bile acid is primarily eliminated in the feces and is not reabsorbed due to its solubility?
What is the primary effect of conjugation on bile acids?
What is the primary effect of conjugation on bile acids?
Which bile acid is produced in greater quantity from bacterial transformation compared to others?
Which bile acid is produced in greater quantity from bacterial transformation compared to others?
Which of the following statements is true regarding the typical ratio of glycine and taurine conjugates in bile salts?
Which of the following statements is true regarding the typical ratio of glycine and taurine conjugates in bile salts?
What regulates the activity of 7--hydroxylase?
What regulates the activity of 7--hydroxylase?
Which of the following secretions are produced by the Brush border of the small intestine?
Which of the following secretions are produced by the Brush border of the small intestine?
Which nutrient absorption occurs through tight junctions between epithelial cells?
Which nutrient absorption occurs through tight junctions between epithelial cells?
What distinguishes L- and D-amino acids in their transport process?
What distinguishes L- and D-amino acids in their transport process?
What is the end product of sucrase activity?
What is the end product of sucrase activity?
Which statement about cholesterol's role in bile acid synthesis is accurate?
Which statement about cholesterol's role in bile acid synthesis is accurate?
How are fatty acids and monoglycerides processed after absorption?
How are fatty acids and monoglycerides processed after absorption?
What is the mechanism for glucose transport in the small intestine?
What is the mechanism for glucose transport in the small intestine?
Flashcards
Digestion process
Digestion process
Breakdown of food into absorbable forms
Digestion phases
Digestion phases
Neurogenic, gastric, intestinal
Saliva composition
Saliva composition
Rich in K+, HCO3-, hypotonic, has enzymes and mucus
Saliva role
Saliva role
Signup and view all the flashcards
Salivary glands
Salivary glands
Signup and view all the flashcards
α-amylase
α-amylase
Signup and view all the flashcards
β-amylase
β-amylase
Signup and view all the flashcards
γ-amylase
γ-amylase
Signup and view all the flashcards
Lactase
Lactase
Signup and view all the flashcards
Lipase
Lipase
Signup and view all the flashcards
Gastric Acid Secretion
Gastric Acid Secretion
Signup and view all the flashcards
HCI Secretion by Parietal Cell
HCI Secretion by Parietal Cell
Signup and view all the flashcards
Pepsinogen
Pepsinogen
Signup and view all the flashcards
Pepsin Function
Pepsin Function
Signup and view all the flashcards
Rennin Function (Infants)
Rennin Function (Infants)
Signup and view all the flashcards
Intrinsic Factor
Intrinsic Factor
Signup and view all the flashcards
Gastric Lipase
Gastric Lipase
Signup and view all the flashcards
Fat Digestion Steps
Fat Digestion Steps
Signup and view all the flashcards
Co-lipase's Role
Co-lipase's Role
Signup and view all the flashcards
Lipase's Action on Triglycerides
Lipase's Action on Triglycerides
Signup and view all the flashcards
What are Lysophospholipids?
What are Lysophospholipids?
Signup and view all the flashcards
Bile's Functions
Bile's Functions
Signup and view all the flashcards
Bile Acids' Role
Bile Acids' Role
Signup and view all the flashcards
Bile acid synthesis
Bile acid synthesis
Signup and view all the flashcards
7-α-hydroxylase
7-α-hydroxylase
Signup and view all the flashcards
Conjugation of bile acids
Conjugation of bile acids
Signup and view all the flashcards
Primary bile acids
Primary bile acids
Signup and view all the flashcards
Secondary bile acids
Secondary bile acids
Signup and view all the flashcards
Enterohepatic circulation
Enterohepatic circulation
Signup and view all the flashcards
Bile salt reabsorption
Bile salt reabsorption
Signup and view all the flashcards
Lithocholic acid excretion
Lithocholic acid excretion
Signup and view all the flashcards
Bile Acid Synthesis Regulation
Bile Acid Synthesis Regulation
Signup and view all the flashcards
Brunner's Glands
Brunner's Glands
Signup and view all the flashcards
Crypts of Lieberkuhn
Crypts of Lieberkuhn
Signup and view all the flashcards
Brush Border
Brush Border
Signup and view all the flashcards
Aminopeptidase Function
Aminopeptidase Function
Signup and view all the flashcards
Dipeptidase Function
Dipeptidase Function
Signup and view all the flashcards
What are Chylomicrons?
What are Chylomicrons?
Signup and view all the flashcards
Monosaccharide Absorption
Monosaccharide Absorption
Signup and view all the flashcards
Study Notes
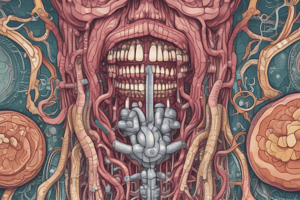
Digestion, Transport and Absorption of Nutrients
- Digestion breaks down naturally occurring food into assimilable forms.
- Proteins are broken down into amino acids.
- Carbohydrates are broken down into monosaccharides.
- Triacylglycerols are broken down into fatty acids and glycerol.
- Minerals and vitamins also become assimilable.
- Digestion has three phases: neurogenic, gastric, and intestinal.
Digestion in the Oral Cavity
- Salivary glands (parotid, sublingual, submaxillary) produce most saliva.
- Acinar cells create saliva similar to plasma composition (Na+, K+, Cl-, HCO3-).
- Duct cells alter the ionic content of saliva.
- Saliva is rich in K+, HCO3-, hypotonic, and contains amylase, lingual lipase, and lysozyme.
- Parasympathetic stimulation increases watery saliva release.
- Saliva helps with mastication, swallowing, and dissolving food molecules.
- Saliva is a medium for hydrolases to act on food.
- Aids in excretion of some drugs.
- Lingual lipase is not significant in humans.
Digestion in the Stomach
- Sight, smell, and taste of food stimulate cerebral cortex and vagal nuclei.
- These stimulate gastric parietal and chief cells.
- Gastric secretions include gastrin, HCl, and H2O.
- Other secretions include pepsin, rennin, and gastric lipase.
- Mucin and inorganic salts are also secreted.
- HCl secretion is controlled by neurocrine (vagus/local reflexes), endocrine (gastrin), and paracrine (histamine) mechanisms.
- Mucus forms a physical barrier between the lumen and epithelium.
- Bicarbonate buffers stomach acid to prevent damage.
- Pepsinogen is an inactive precursor to pepsin which is activated by HCl.
- Pepsin is an endopeptidase that breaks down proteins.
- Rennin is important in infants.
- Gastric lipase is produced by chief cells.
- It's important during the neonatal period.
Digestion in the Intestines
- Chyme moves to the duodenum.
- Pancreatic and biliary secretions neutralize pH and inactivate pepsin.
- Bile acids emulsify fats & enable fat-soluble vitamin absorption.
- Bile acids neutralize chyme and excrete cholesterol, bile pigments, and drugs.
Pancreatic Secretions
- Pancreatic secretions include various zymogens (inactive enzymes).
- These activate into active enzymes.
- Different enzymes digest different substrates (peptides, phospholipids, triglycerides, starch, glycogen, RNA, DNA).
- Zymogens are activated by enteropeptidase.
Carbohydrate Digestion
- Starch and glycogen are broken down into glucose.
- Amylase breaks down starch/glycogen.
- Maltase, sucrase, and lactase further break down disaccharides into monosaccharides.
- Monosaccharides are absorbed in the intestines.
Disaccharidases
- Brush border enzymes (maltase, sucrase-isomaltase, lactase, trehalase) act on disaccharides.
- Lactase activity usually declines after weaning in most mammals.
Fat Digestion
- Lipids are emulsified by bile salts.
- Pancreatic lipase hydrolyzes triglycerides.
- Bile salts, colipase, and phospholipids are required for lipase action.
- Short- and medium-chain fatty acids can be absorbed directly, while longer chains dissolve in lipid droplets.
Intestinal Secretions
- Intestinal secretions contain various enzymes for breaking down peptides, and disaccharides, organic and nucleic acids.
- Enzymes are found in the brush border
Absorption in Small Intestine
- All nutrients pass through epithelial cells.
- Tight junctions prevent movement between cells
- Amino acids, monosaccharides, and fatty acids are transported through membranes and into blood capillaries.
- Fatty acids and monoglycerides are reassembled into triglycerides and coated with proteins to form chylomicrons.
- Chylomicrons are transported to lymphatic capillaries (lacteal).
Lipid Absorption
- Intestinal epithelial cells synthesize triacylglycerols, cholesterol esters, phospholipids, and apoproteins.
- These are packaged into chylomicrons.
- Free fatty acids (<10 carbons) are transported unesterified in the portal vein.
- Chylomicrons are too large to pass through capillary beds.
- They are secreted into the lymph and enter the bloodstream via the thoracic duct.
Colon
- No digestion occurs in the colon.
- The colon absorbs water and ions.
- It contains bacteria that synthesize vitamin K.
- Bacterial fermentation produces gases and various acids.
- Ammonia (NH3) is absorbed and removed by the liver.
Bacteria in the Intestine
- Bacteria produce various gases (CO2, methane, H2S) and organic acids.
- Bacterial activity generates considerable amounts of ammonia (NH3).
- The liver removes ammonia.
- Bacteria synthesize vitamin K and biotin.
Defects in Digestion and Absorption
- Lactose intolerance, sucrase deficiency, and monosaccharide deficiency can result in issues with carbohydrate absorption.
- Chyluria, chylothorax, and co-lipase deficiency affect lipid digestion/absorption.
- Deficiencies in protein digestion may result from incomplete digestion of polypeptides or issues with mucosal permeability.
Diseases Resulting From Defects in Digestion and Malabsorption
- Anemia (iron, vitamin B12, folic acid deficiency), edema (protein digestion/absorption), and tetany (Ca2+, Mg2+, vitamin D deficiency) may arise.
- Osteoporosis (Ca2+, vitamin D deficiency), lactose intolerance, bleeding/bruising (vitamin K deficiency), steatorrhea (lipid digestion/absorption issues), and Hartnup disease (neutral amino acid carrier defect) are other possible illnesses.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.