Podcast
Questions and Answers
Which mechanism primarily leads to osmotic diarrhea?
Which mechanism primarily leads to osmotic diarrhea?
- Inflammation-induced damage to the intestinal mucosa reducing absorption.
- Malabsorption of nutrients causing increased osmolality in the intestinal lumen. (correct)
- Increased secretion of electrolytes into the intestinal lumen.
- Increased intestinal motility reducing the time available for fluid absorption.
What is the main difference between secretory and exudative diarrhea?
What is the main difference between secretory and exudative diarrhea?
- Secretory diarrhea involves inflammation, whereas exudative diarrhea does not.
- Secretory diarrhea stops with fasting, whereas exudative diarrhea does not.
- Secretory diarrhea involves increased electrolyte secretion, whereas exudative diarrhea involves the leakage of blood and mucus. (correct)
- Secretory diarrhea is caused by bacterial toxins, whereas exudative diarrhea is caused by viruses.
Which of the following is a key characteristic of diarrhea caused by altered intestinal motility?
Which of the following is a key characteristic of diarrhea caused by altered intestinal motility?
- Increased absorption of electrolytes and water.
- Normal transit time allowing for adequate fluid absorption.
- Decreased intestinal contractions promoting stasis and bacterial overgrowth.
- Reduced contact time between the intestinal contents and mucosa. (correct)
A patient presents with chronic diarrhea and laboratory tests reveal decreased levels of serum albumin and the presence of fecal leukocytes. What type of diarrhea is most likely?
A patient presents with chronic diarrhea and laboratory tests reveal decreased levels of serum albumin and the presence of fecal leukocytes. What type of diarrhea is most likely?
How does bacterial overgrowth in the small intestine typically lead to diarrhea?
How does bacterial overgrowth in the small intestine typically lead to diarrhea?
Which of the following mechanisms contributes to diarrhea by directly altering the osmotic gradient in the intestinal lumen?
Which of the following mechanisms contributes to diarrhea by directly altering the osmotic gradient in the intestinal lumen?
In cases of diarrhea caused by Salmonella enterica, which of the following mechanisms is NOT directly associated with its pathogenesis?
In cases of diarrhea caused by Salmonella enterica, which of the following mechanisms is NOT directly associated with its pathogenesis?
How does increased cyclic adenosine monophosphate (cAMP) contribute to secretory diarrhea?
How does increased cyclic adenosine monophosphate (cAMP) contribute to secretory diarrhea?
Which characteristic is least likely to be observed in the intestines of a piglet infected with Enterotoxigenic Escherichia coli (ETEC)?
Which characteristic is least likely to be observed in the intestines of a piglet infected with Enterotoxigenic Escherichia coli (ETEC)?
Enterotoxigenic Escherichia coli (ETEC) primarily affects which animal group the most?
Enterotoxigenic Escherichia coli (ETEC) primarily affects which animal group the most?
What role do fimbriae play in the pathogenesis of diarrhea caused by Enterotoxigenic Escherichia coli (ETEC)?
What role do fimbriae play in the pathogenesis of diarrhea caused by Enterotoxigenic Escherichia coli (ETEC)?
What is the primary effect of enterotoxins produced by Enterotoxigenic Escherichia coli (ETEC) on intestinal cells?
What is the primary effect of enterotoxins produced by Enterotoxigenic Escherichia coli (ETEC) on intestinal cells?
Vasoactive intestinal polypeptide secretion from pancreatic islet cell tumors can lead to diarrhea via what mechanism?
Vasoactive intestinal polypeptide secretion from pancreatic islet cell tumors can lead to diarrhea via what mechanism?
Which of the following is NOT a general mechanism of diarrhea?
Which of the following is NOT a general mechanism of diarrhea?
How does inflammation contribute to secretory diarrhea?
How does inflammation contribute to secretory diarrhea?
In a dog presenting with acute diarrhea and systemic signs, which of the following is the MOST appropriate initial diagnostic step to differentiate between potential causes?
In a dog presenting with acute diarrhea and systemic signs, which of the following is the MOST appropriate initial diagnostic step to differentiate between potential causes?
According to the European guidelines for treating acute diarrhea, when is antibiotic use MOST clearly indicated?
According to the European guidelines for treating acute diarrhea, when is antibiotic use MOST clearly indicated?
A dog presents with chronic diarrhea that has not responded to initial treatments. Following the sequential treatment protocol, what is the MOST appropriate next step if an elimination diet proves ineffective?
A dog presents with chronic diarrhea that has not responded to initial treatments. Following the sequential treatment protocol, what is the MOST appropriate next step if an elimination diet proves ineffective?
Which dietary characteristic is MOST important when selecting a diet for managing acute diarrhea?
Which dietary characteristic is MOST important when selecting a diet for managing acute diarrhea?
A cat is diagnosed with IBD and has not responded adequately to an elimination diet and prednisolone. Which medication should be considered NEXT?
A cat is diagnosed with IBD and has not responded adequately to an elimination diet and prednisolone. Which medication should be considered NEXT?
What is the initial recommended dosage of prednisolone for treating IBD in dogs, according to the provided guidelines?
What is the initial recommended dosage of prednisolone for treating IBD in dogs, according to the provided guidelines?
When should abdominal radiographs be considered as part of the diagnostic workup for acute diarrhea?
When should abdominal radiographs be considered as part of the diagnostic workup for acute diarrhea?
Why is cobalamin supplementation often recommended in the treatment of IBD in cats?
Why is cobalamin supplementation often recommended in the treatment of IBD in cats?
Which of the following mechanisms directly contributes to malabsorptive diarrhea by reducing the surface area available for nutrient absorption?
Which of the following mechanisms directly contributes to malabsorptive diarrhea by reducing the surface area available for nutrient absorption?
Protein-losing enteropathies are often associated with damage to lymphatic vessels. What is a common clinicopathological finding in animals with this condition?
Protein-losing enteropathies are often associated with damage to lymphatic vessels. What is a common clinicopathological finding in animals with this condition?
Which of the following infectious agents is most likely to cause non-protein losing enteropathy by directly targeting and damaging villous enterocytes?
Which of the following infectious agents is most likely to cause non-protein losing enteropathy by directly targeting and damaging villous enterocytes?
Lymphangiectasia leads to protein-losing enteropathy through which primary mechanism?
Lymphangiectasia leads to protein-losing enteropathy through which primary mechanism?
What is the primary characteristic differentiating non-protein losing enteropathies from protein-losing enteropathies?
What is the primary characteristic differentiating non-protein losing enteropathies from protein-losing enteropathies?
In cases of malabsorptive diarrhea, an increased thickness of the lamina propria can contribute to the condition. Which of the following is a plausible cause for this increased thickness?
In cases of malabsorptive diarrhea, an increased thickness of the lamina propria can contribute to the condition. Which of the following is a plausible cause for this increased thickness?
How does rotavirus contribute to malabsorptive diarrhea in affected animals?
How does rotavirus contribute to malabsorptive diarrhea in affected animals?
Which of the following mechanisms best describes how large, undigested solutes typically lead to osmotic diarrhea in non-protein losing enteropathies?
Which of the following mechanisms best describes how large, undigested solutes typically lead to osmotic diarrhea in non-protein losing enteropathies?
Increased intestinal permeability can contribute to protein-losing enteropathy. What alteration to the intestinal barrier is most directly responsible for this increased permeability?
Increased intestinal permeability can contribute to protein-losing enteropathy. What alteration to the intestinal barrier is most directly responsible for this increased permeability?
Which factor can influence the permeability of junctional complexes in the intestinal mucosa, potentially leading to protein loss?
Which factor can influence the permeability of junctional complexes in the intestinal mucosa, potentially leading to protein loss?
Which of the following mechanisms accurately describes how Clostridium perfringens type C disrupts blood vessels, leading to diarrhea?
Which of the following mechanisms accurately describes how Clostridium perfringens type C disrupts blood vessels, leading to diarrhea?
Why is trypsin sensitivity a significant characteristic of the beta toxin (CPB) produced by Clostridium perfringens type C?
Why is trypsin sensitivity a significant characteristic of the beta toxin (CPB) produced by Clostridium perfringens type C?
What is the most likely consequence of a drug-induced hypomotility in the gastrointestinal tract?
What is the most likely consequence of a drug-induced hypomotility in the gastrointestinal tract?
When evaluating a gastrointestinal sample, which observation would suggest a possible neoplastic process rather than an inflammatory lesion?
When evaluating a gastrointestinal sample, which observation would suggest a possible neoplastic process rather than an inflammatory lesion?
Which term describes a lesion that extends throughout all layers of the intestinal wall?
Which term describes a lesion that extends throughout all layers of the intestinal wall?
When examining a cross-section of the intestine, a pathologist notes a distinct mucoid appearance. Which of the following is the most likely underlying cause?
When examining a cross-section of the intestine, a pathologist notes a distinct mucoid appearance. Which of the following is the most likely underlying cause?
Which of the following accurately describes how hypermotility affects water and nutrient absorption in the gastrointestinal tract?
Which of the following accurately describes how hypermotility affects water and nutrient absorption in the gastrointestinal tract?
A veterinarian notes 'ground glass' serosa during a canine necropsy. Which disease is most aligned with this observation?
A veterinarian notes 'ground glass' serosa during a canine necropsy. Which disease is most aligned with this observation?
Distinguishing between serosal and mucosal location of a lesion helps determine what aspect of the disease process?
Distinguishing between serosal and mucosal location of a lesion helps determine what aspect of the disease process?
A veterinarian discovers a mass on the cut surface of an intestinal sample that appears friable. What is the MOST likely cause?
A veterinarian discovers a mass on the cut surface of an intestinal sample that appears friable. What is the MOST likely cause?
What is the primary characteristic of protein-losing enteropathy (PLE)?
What is the primary characteristic of protein-losing enteropathy (PLE)?
Which of the following is NOT typically associated with the clinical presentation of protein-losing enteropathy (PLE)?
Which of the following is NOT typically associated with the clinical presentation of protein-losing enteropathy (PLE)?
In a patient with chronic small intestinal diarrhea, what is the recommended first step in the diagnostic process?
In a patient with chronic small intestinal diarrhea, what is the recommended first step in the diagnostic process?
When is antibiotic (AB) therapy most appropriate for acute diarrhea cases?
When is antibiotic (AB) therapy most appropriate for acute diarrhea cases?
An 8-year-old dog presents with lethargy, inappetence, and chronic (2 months) waxing and waning diarrhea. On physical exam, the dog appears normal. What is the MOST appropriate next step in refining the problem of diarrhea?
An 8-year-old dog presents with lethargy, inappetence, and chronic (2 months) waxing and waning diarrhea. On physical exam, the dog appears normal. What is the MOST appropriate next step in refining the problem of diarrhea?
An 8-year-old dog presents with chronic small intestinal diarrhea. After ruling out extra-intestinal causes, which of the following is the MOST likely differential diagnosis category?
An 8-year-old dog presents with chronic small intestinal diarrhea. After ruling out extra-intestinal causes, which of the following is the MOST likely differential diagnosis category?
Which of the following is an extra-intestinal cause of chronic small intestinal diarrhea?
Which of the following is an extra-intestinal cause of chronic small intestinal diarrhea?
Which of the following is a GI cause of chronic small intestinal diarrhea?
Which of the following is a GI cause of chronic small intestinal diarrhea?
Flashcards
Pathophysiology
Pathophysiology
The study of how diseases or injuries disrupt normal physiological processes.
Diarrhea
Diarrhea
Abnormally liquid or frequent bowel movements, leading to increased fluid loss.
DVM, Dipl.
DVM, Dipl.
A veterinarian who has completed additional training and passed a board certification exam in a specific area of veterinary medicine.
Sources of Intestinal Fluid
Sources of Intestinal Fluid
Signup and view all the flashcards
Intestinal Fluid Absorption
Intestinal Fluid Absorption
Signup and view all the flashcards
Diarrhea Mechanisms
Diarrhea Mechanisms
Signup and view all the flashcards
Secretory Diarrhea
Secretory Diarrhea
Signup and view all the flashcards
cAMP role in Secretory Diarrhea
cAMP role in Secretory Diarrhea
Signup and view all the flashcards
Infectious Causes of Secretory Diarrhea
Infectious Causes of Secretory Diarrhea
Signup and view all the flashcards
Non-Infectious Causes of Secretory Diarrhea
Non-Infectious Causes of Secretory Diarrhea
Signup and view all the flashcards
ETEC Common Hosts
ETEC Common Hosts
Signup and view all the flashcards
ETEC Mechanism
ETEC Mechanism
Signup and view all the flashcards
Malabsorptive Diarrhea
Malabsorptive Diarrhea
Signup and view all the flashcards
Protein-Losing Enteropathy
Protein-Losing Enteropathy
Signup and view all the flashcards
Lymphangiectasia
Lymphangiectasia
Signup and view all the flashcards
Non-Protein Losing Enteropathy
Non-Protein Losing Enteropathy
Signup and view all the flashcards
Rotavirus
Rotavirus
Signup and view all the flashcards
Increased Intestinal Permeability
Increased Intestinal Permeability
Signup and view all the flashcards
E. coli-Associated Diarrhea
E. coli-Associated Diarrhea
Signup and view all the flashcards
Clinical signs of Protein Losing Enteropathy
Clinical signs of Protein Losing Enteropathy
Signup and view all the flashcards
Malabsorptive Diarrhea Mechanisms
Malabsorptive Diarrhea Mechanisms
Signup and view all the flashcards
Increased Permeability Causes
Increased Permeability Causes
Signup and view all the flashcards
Clostridium perfringens type C
Clostridium perfringens type C
Signup and view all the flashcards
Hypomotility
Hypomotility
Signup and view all the flashcards
Hypermotility
Hypermotility
Signup and view all the flashcards
GI Tract Evaluation
GI Tract Evaluation
Signup and view all the flashcards
"Added" in GI disease
"Added" in GI disease
Signup and view all the flashcards
"Subtracted" in GI disease
"Subtracted" in GI disease
Signup and view all the flashcards
Lesion distribution
Lesion distribution
Signup and view all the flashcards
Friable cut surface appearance
Friable cut surface appearance
Signup and view all the flashcards
Hemorrhagic cut surface appearance
Hemorrhagic cut surface appearance
Signup and view all the flashcards
Mucoid cut surface appearance
Mucoid cut surface appearance
Signup and view all the flashcards
Helminths
Helminths
Signup and view all the flashcards
Giardia
Giardia
Signup and view all the flashcards
Iatrogenic
Iatrogenic
Signup and view all the flashcards
Parvovirus
Parvovirus
Signup and view all the flashcards
Acute Diarrhea Treatment (Europe)
Acute Diarrhea Treatment (Europe)
Signup and view all the flashcards
Highly Digestible Diets
Highly Digestible Diets
Signup and view all the flashcards
IBD
IBD
Signup and view all the flashcards
When to perform biopsies for Chronic Enteropathy/IBD
When to perform biopsies for Chronic Enteropathy/IBD
Signup and view all the flashcards
Protein Losing Enteropathy (PLE)
Protein Losing Enteropathy (PLE)
Signup and view all the flashcards
PLE Clinical Signs
PLE Clinical Signs
Signup and view all the flashcards
Diarrhea Case Workup
Diarrhea Case Workup
Signup and view all the flashcards
Victor's Diarrhea
Victor's Diarrhea
Signup and view all the flashcards
Extra-GI Causes of Chronic Small Intestinal Diarrhea
Extra-GI Causes of Chronic Small Intestinal Diarrhea
Signup and view all the flashcards
GI Causes of Chronic Small Intestinal Diarrhea
GI Causes of Chronic Small Intestinal Diarrhea
Signup and view all the flashcards
DDx Chronic Small Intestinal Diarrhea
DDx Chronic Small Intestinal Diarrhea
Signup and view all the flashcards
Study Notes
Pathophysiology of Diarrhea Study Notes
- Diarrhea is characterized by excess water in feces, resulting from excessive secretions and/or decreased absorption.
- Diarrhea leads to severe electrolyte depletion, acid-base imbalance, and dehydration.
- A thorough history and physical examination are crucial for classifying the type of diarrhea.
Normal Intestine Function
- Fluid for normal intestine function is derived from ingested material and normal secretions from such organs as the stomach, intestine, pancreas, and gallbladder.
- Most fluid is absorbed in the small intestine, which has a limited capacity.
- Tight junctions in the small intestine allow small molecules and water to pass through.
- The cecum and colon absorb most of the water in horses.
- The normal function for intestines is when absoprtion exceeds secretion, so they can function as expected.
Mechanisms of Diarrhea
- Understanding the pathophysiology is important for categorizing diarrhea and guiding diagnoses and therapy.
- General mechanisms include secretory, malabsorptive, increased permeability, and abnormal motility processes.
- Multiple diarrhea forms can simultaneously occur with the same disease or etiologic agent.
- Salmonella enterica is one such example; it leads to secretory diarrhea by blocking chloride channels (due to effector proteins) and inducing hypersecretion of chloride via prostaglandin upregulation.
- Salmonella enterica also causes malabsorptive diarrhea as apoptosis of infiltrated enterocytes reduces mucosal surface area.
- A further mechanism of Salmonella enterica is to promote increased permeability when cytotoxins alter vascular permeability.
Secretory Diarrhea
- Secretory diarrhea is increased secretion of chloride, sodium, and other electrolytes.
- Exudation of fluid from inflammation can contribute to secretory diarrhea through prostaglandins and cytokines.
- Shifting the osmotic gradient via luminal contents can cause secondary secretory diarrhea.
- This process can lead to osmotic diarrhea and non-protein losing enteropathy.
Increased Chloride Secretion
- Cyclic adenosine monophosphate (cAMP) mediates increased chloride secretion.
- Chloride secretion can be due to reduced passive absorption of water and the promotion of chloride secretion.
- Infectious causes include Escherichia coli and Salmonella enterica.
- Non-infectious causes include vasoactive intestinal polypeptides from pancreatic islet cell tumors and histamine from mast cell tumors.
Enterotoxigenic Escherichia coli (ETEC)
- ETEC primarily affects calves, piglets, and lambs.
- ETEC uses fimbriae to adhere to microvilli; these fimbriae adhesins are age-dependent.
- Its enterotoxins bind to guanylate cyclase c receptor Gsa protein, which causes increased levels of cGMP and cAMP.
- This process causes secretion of chloride, blocks sodium absorption, and results in osmotic gradient leading to secretory diarrhea.
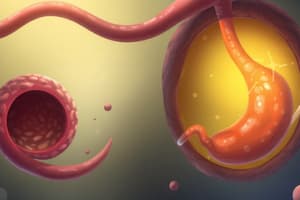
Malabsorptive Diarrhea
- Malabsorptive diarrhea is an impaired ability to absorb nutrients from villous damage, atrophy, or maldigested digesta.
- It is important to distinguish between protein-losing and non-protein-losing enteropathy since clinicopathologic findings can suggest prognosis and influence treatment decisions.
- This is often associated with severe hypoproteinemia and hypoalbuminemia.
Mechanisms of Malabsorptive Diarrhea
-
Loss of protein due to damaged mucosa is a common mechanism; ruptured lymphatic vessels typically cause it.
-
Loss of surface area for solute absorption occurs in the following ways
- Loss of microvilli/villous enterocytes.
- Overall villous atrophy.
-
Increased thickness of lamina propria occurs through inflammatory cells, fibrosis, and neoplastic cells.
-
Loss of digestive enzymes to break down food includes exocrine pancreas insufficiency (maldigestion) and loss of villous enterocytes.
Protein-Losing Enteropathies
- These are often associated with damage to lymphatic vessels
- severe hypoproteinemia.
- Infections: parasites (Cooperia, Nematodirus, Strongyloides, Trichostrongylus, cyathostomes), Johne's .
- Non-infectious causes include: lymphangiectasia, lymphoma, and inflammatory bowel disease.
- Lymphangiectasia, common in dogs, is a dilation, obstruction, and/or dysfunction of lymphatic vessels leading to their rupture, resulting in lymphatic fluid (rich in protein) leak into the intestinal lumen ultimately leading to malabsorptive diarrhea (protein loss).
Non-Protein Losing Enteropathies
- Non-protein enteropathies feature impaired absorption of electrolytes/nutrients.
- Patient's can still have hypoproteinemia.
- These include mucosa or digesta problems, where large, undigested solutes lead to osmotic diarrhea.
- Infectious etiologies to consider are rotavirus, Johne's, cryptosporidium, and coccidia.
- Non-infectious causes include laxatives, grain overload, and dietary, or antibiotic imbalances.
- Rotavirus targets villous enterocytes, thus impairing absorption of small solutes and production of enzymes.
- Rotavirus causes villous atrophy which results in malabsorptive diarrhea (a non-protein losing enteropathy).
- Rotavirus' secretory enterotoxin also increases chloride secretion, leading to secretory diarrhea
Increased Intestinal Permeability
- This can happen when there is inflammation or destruction of the mucosal barrier or vasculature; leaky tight junctions then permit macromolecules to pass through.
- Junctional complexes are sensitive to Starling forces.
- Potential infectious triggers are Clostridium perfringens, E. coli, Lawsonia intracellularis, parvovirus, and parasites.
- Non-infectious causes include amyloidosis, lymphoma, congestive heart failure, and portal hypertension.
Clostridium perfringens Type C
- This form of Clostridium particularly affects piglets, foals, lambs, kids, and calves.
- It is known for it's alpha toxin (CPA) and beta toxin (CPB), the latter of which is trypsin labile. Beta2 toxin, perfringolysin, and large clostridial toxin Tpel are also seen with the disease
- There is bacterial overgrowth, and CPB, the previously mentioned beta toxin, is produced.
- It forms pores in endothelial cells, influx of Ca, Na, and Cl causes swelling; this can kill the cell.
- Increased permeability diarrhea and ischemic necrosis of mucosa can greatly contribute to the effects.
Abnormal Motility
- Abnormal motility is a minor cause/contributor to diarrhea.
- Hypermotility leads to less efficient water and nutrient absorption (the primary disease is uncharacterized in veterinary medicine).
- Hypomotility promotes bacterial overgrowth.
- Potential causes include: parasites (cyathostomes, Oesophagostomum spp.), peritonitis, drugs, dysautonomia, and behavioral related effects.
Evaluating the Gastrointestinal Tract
- Consider normal parameters for the species, such as orientation, symmetry, size, number, color, and consistency.
- Most disease comes from something "added" (inflammation, hyperplasia, metaplasia, neoplasia) or "subtracted" (atrophy, hypoplasia).
- The cecum typically has one constituent in dogs and horses and two in chickens.
- Evaluate location (serosa vs. mucosa vs. transmural, mesenteric vs. anti-mesenteric), distribution (focal, multifocal, locally extensive, diffuse)
- Further consider measurement, shape, and consistency (soft, firm, hard).
Additional Considerations
- Assess characteristics of digesta (amount, color, consistency).
- Evaluate how thick the wall of a hollow viscus is (mucosa, submucosa, muscularis, serosa).
- Consider cut surface: solid, friable, hemorrhagic, mucoid or cystic.
Case Study Points
- Veterinarians used the cases of Victor and Liesl to show how to apply the principles from this presentation.
- Victor, an 8 year old cross breed dog had clinical signs for 2 months, showing waxing and waning vomiting with diarrhea as a common presenting clinical sign. Analysis also showed hyponatremia and hyperkalemia. Ultimately was diagnosed wth Addison's.
- Siamese, 8mo, female- Chronic diarrhea, fresh blood, muscus, Clinically WNL were the presenting signs of another case named Kitty! After further testing, PCR tested ositive for Tritrichomonas fetus.
- Then in another practice case study, a 7 year old female labrador named Liesl had clinical signs for 3 months including liquid diarrhea, 4-5 times a day, showing weightloss and ascites; the clinical sign of the other cases in contrast to their previous case. Ultimately, the dog was having the clinical issue because of a protein lose issue involving the animals lymphatic system.
Diarrhea Overview for Cats and Dogs
- Differentiate between acute vs chronic small animal diarrhea cases and with or without systemic signs.
- Determine if the diarrhea is small intestinal, large intestinal, or mixed.
- Develop logical approaches to your small animal workup, using know treatments and diagnoses.
- Diarrhea signs are: increased frequency, volume or fluidity.
- Melena signs can include tarry feces and flatulance from gas.
- In some cases, Dyschezia can be difficult or bring pain to the patient when defecating.
- Hematochezia will cause fresh blood in stool and Tenesmus will cause straining.
- Chronic cases can have intermittant signs greater than or equal to 3 weeks old.
- Acute signs may be self resolving, symptomatic with a need for some treatment, whereas chronic signs may lead the practice to determine more diagnostic investigations.
- For treating acute cases, highly digestible foods with lower residue count and moderate fat are important.
- With chronic, the patient history is very important at determining the overall outcome and diagnosis, alongside the workup results.
Antibiotics for Diarrhea
- Metronidazole creates a significant shift in the normal microbiome; illustrated by dysbiosis index.
- C. Hiranonis is a key species important for converting primary to secondary bile acids.
- Dysbiosis from Antibiotic overuse could lead to problems down the line.
- In cases where secondary bile acids cannot survive due to presence of Dysbiosis bacteria- this pro inflammatory with chronic inflammation changes and permiability increase
Protein Losing Enteropathy Definition
- Syndrome of intestinal diseases with non-selective protein losses via albumin and globulins reduction.
- Some causes of this clinical issue can stem from IBD (inflammatory bowel disease), Neoplasia (Lymphoma)- and Lymphangiectasia. These often present as Clinical issues.
Cased Studies
- The lecture uses various case studies to show how a new practitioner can approach each unique set of symptoms.
- Two major diseases are commonly tested for, Inflammatory Bowel Disease vs Chronic Inflammatory Enteropathy.
- Long term outcomes are found to vary based on long term clinical signs.
- Some examples of common drugs prescribed include: Metronidazole, Tylosin and prednisolone.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.