Podcast
Questions and Answers
What condition is primarily caused by the failure of insulin-sensitive tissues to respond adequately to insulin?
What condition is primarily caused by the failure of insulin-sensitive tissues to respond adequately to insulin?
- Pancreatic beta-cell dysfunction
- Hypoglycemia
- Insulin resistance (correct)
- Lipid metabolism disorder
How does glucagon primarily raise blood glucose levels?
How does glucagon primarily raise blood glucose levels?
- By stimulating glycogenolysis and gluconeogenesis (correct)
- By inhibiting insulin secretion
- By increasing protein synthesis
- By promoting lipolysis
In individuals with diabetes, how might glucagon regulation be impaired?
In individuals with diabetes, how might glucagon regulation be impaired?
- Lower than normal glucagon levels during meals
- Inappropriately elevated glucagon levels during hyperglycemia (correct)
- Increased insulin activity on glucagon secretion
- Enhanced sensitivity of alpha cells to insulin
What is a key consequence of pancreatic beta-cell dysfunction?
What is a key consequence of pancreatic beta-cell dysfunction?
Which counterregulatory hormones may stimulate glucagon secretion during hypoglycemia?
Which counterregulatory hormones may stimulate glucagon secretion during hypoglycemia?
Which process is related to hyperglycemia and can be exacerbated by impaired insulin-glucagon balance?
Which process is related to hyperglycemia and can be exacerbated by impaired insulin-glucagon balance?
What is the primary effect of insulin resistance on glucose metabolism?
What is the primary effect of insulin resistance on glucose metabolism?
Which of the following lipid profiles is most characteristic of individuals with diabetes?
Which of the following lipid profiles is most characteristic of individuals with diabetes?
What is a common lifestyle modification strategy for managing insulin resistance?
What is a common lifestyle modification strategy for managing insulin resistance?
Which medication is commonly used to increase insulin sensitivity in individuals with insulin resistance?
Which medication is commonly used to increase insulin sensitivity in individuals with insulin resistance?
What is the primary benefit of using HbA1c testing in diabetes management?
What is the primary benefit of using HbA1c testing in diabetes management?
What is the primary purpose of monitoring HbA1c levels in individuals with diabetes?
What is the primary purpose of monitoring HbA1c levels in individuals with diabetes?
An HbA1c level of 8.0% would be considered:
An HbA1c level of 8.0% would be considered:
Which of the following factors can influence HbA1c levels?
Which of the following factors can influence HbA1c levels?
A patient with an HbA1c of 6.5% would likely be classified as:
A patient with an HbA1c of 6.5% would likely be classified as:
What is a potential consequence of consistently elevated HbA1c levels?
What is a potential consequence of consistently elevated HbA1c levels?
What is the most common method for diagnosing diabetic retinopathy?
What is the most common method for diagnosing diabetic retinopathy?
Which of the following laboratory tests is most helpful in evaluating kidney damage in patients with end-stage kidney disease?
Which of the following laboratory tests is most helpful in evaluating kidney damage in patients with end-stage kidney disease?
Which of the following is a risk factor for foot ulcers in patients with end-stage kidney disease?
Which of the following is a risk factor for foot ulcers in patients with end-stage kidney disease?
What is the target HbA1c level for most individuals with diabetes?
What is the target HbA1c level for most individuals with diabetes?
A patient with a moderately decreased estimated glomerular filtration rate (eGFR) would be classified as having which stage of chronic kidney disease?
A patient with a moderately decreased estimated glomerular filtration rate (eGFR) would be classified as having which stage of chronic kidney disease?
What is the primary purpose of glycated hemoglobin (HbA1c) testing in diabetes management?
What is the primary purpose of glycated hemoglobin (HbA1c) testing in diabetes management?
A patient's fasting plasma glucose (FPG) level is measured at 6.2 mmol/L. According to Canadian lab values, how would this result be classified?
A patient's fasting plasma glucose (FPG) level is measured at 6.2 mmol/L. According to Canadian lab values, how would this result be classified?
A patient's HbA1c level is determined to be 7.0%. Based on Canadian lab values, this result indicates:
A patient's HbA1c level is determined to be 7.0%. Based on Canadian lab values, this result indicates:
A patient has a 2-hour oral glucose tolerance test (OGTT) result of 9.5 mmol/L. According to Canadian lab values, this result would be classified as:
A patient has a 2-hour oral glucose tolerance test (OGTT) result of 9.5 mmol/L. According to Canadian lab values, this result would be classified as:
What is the target fasting blood glucose level for individuals with diabetes according to Canadian lab values?
What is the target fasting blood glucose level for individuals with diabetes according to Canadian lab values?
Which of the following blood glucose levels 2 hours after meals falls within the acceptable range for diabetes management?
Which of the following blood glucose levels 2 hours after meals falls within the acceptable range for diabetes management?
What is the target Hemoglobin A1c (HbA1c) level for individuals with diabetes?
What is the target Hemoglobin A1c (HbA1c) level for individuals with diabetes?
An individual with diabetes has a pre-meal blood glucose level of 3.5 mmol/L. How should this result be interpreted?
An individual with diabetes has a pre-meal blood glucose level of 3.5 mmol/L. How should this result be interpreted?
What is classified as impaired fasting glucose (IFG) according to Canadian lab values?
What is classified as impaired fasting glucose (IFG) according to Canadian lab values?
Which of the following values would indicate macroalbuminuria?
Which of the following values would indicate macroalbuminuria?
What fasting plasma glucose (FPG) level indicates diabetes according to Canadian lab values?
What fasting plasma glucose (FPG) level indicates diabetes according to Canadian lab values?
What is the desirable level of total cholesterol according to Canadian lab values?
What is the desirable level of total cholesterol according to Canadian lab values?
Which of the following lipoprotein cholesterol levels is considered optimal?
Which of the following lipoprotein cholesterol levels is considered optimal?
Which range indicates impaired glucose tolerance (IGT) based on the 2-hour oral glucose tolerance test (OGTT)?
Which range indicates impaired glucose tolerance (IGT) based on the 2-hour oral glucose tolerance test (OGTT)?
What characterizes Type 1 Diabetes?
What characterizes Type 1 Diabetes?
What is a common characteristic of Type 2 Diabetes?
What is a common characteristic of Type 2 Diabetes?
Which of the following is a risk factor for developing Type 2 Diabetes?
Which of the following is a risk factor for developing Type 2 Diabetes?
Which environmental factor is linked to an increased risk of diabetes?
Which environmental factor is linked to an increased risk of diabetes?
What is the recommended initial treatment for managing hypoglycemia in a conscious patient?
What is the recommended initial treatment for managing hypoglycemia in a conscious patient?
Which of the following is a significant barrier in nurse-patient communication for diabetic patients?
Which of the following is a significant barrier in nurse-patient communication for diabetic patients?
Which of the following factors can negatively influence medication adherence in diabetic patients?
Which of the following factors can negatively influence medication adherence in diabetic patients?
What should a nurse do if a patient becomes unconscious due to hypoglycemia?
What should a nurse do if a patient becomes unconscious due to hypoglycemia?
Which communication technique is essential for improving patient participation in their diabetes care?
Which communication technique is essential for improving patient participation in their diabetes care?
What is the main purpose of bacterial adhesins in the context of UTI?
What is the main purpose of bacterial adhesins in the context of UTI?
Which of the following factors can lead to bacterial colonization in the urinary tract?
Which of the following factors can lead to bacterial colonization in the urinary tract?
What is one effect of the innate immune response during a urinary tract infection?
What is one effect of the innate immune response during a urinary tract infection?
How does bacterial colonization contribute to UTI symptoms?
How does bacterial colonization contribute to UTI symptoms?
Which demographic factor increases susceptibility to urinary tract infections in females?
Which demographic factor increases susceptibility to urinary tract infections in females?
Which medical condition is associated with an increased risk of urinary tract infections?
Which medical condition is associated with an increased risk of urinary tract infections?
What role do Toll-like receptors (TLRs) play in the immune response to UTIs?
What role do Toll-like receptors (TLRs) play in the immune response to UTIs?
What is a consequence of biofilm formation by bacteria in the urinary tract?
What is a consequence of biofilm formation by bacteria in the urinary tract?
Which immune cells are primarily recruited during the inflammatory response in a UTI?
Which immune cells are primarily recruited during the inflammatory response in a UTI?
What is the primary reason older individuals are at greater risk for urinary tract infections?
What is the primary reason older individuals are at greater risk for urinary tract infections?
Study Notes
Diabetic Neuropathy Overview
- Caused by nerve ischemia from microvascular disease, hyperglycemia effects, and metabolic changes.
- Multiple forms exist, each with distinct characteristics and outcomes.
Types of Diabetic Neuropathy
-
Symmetric Polyneuropathy
- Most common form, affects distal parts of feet and hands (stocking-glove distribution).
- Symptoms include paresthesias, dysesthesias, and loss of touch, vibration, proprioception, or temperature.
- Can lead to foot trauma, ulcers, infections, and Charcot arthropathy due to abnormal weight distribution.
-
Small-Fiber Neuropathy
- Characterized by pain, numbness, and loss of temperature sensation, while vibration and position sense remain intact.
- Patients at high risk for foot ulcers and neuropathic joint degeneration.
-
Large-Fiber Neuropathy
- Symptoms include muscle weakness, loss of vibration and position sense, and absent deep tendon reflexes.
- May lead to foot intrinsic muscle atrophy and foot drop.
-
Autonomic Neuropathy
- Can cause a range of symptoms including orthostatic hypotension, resting tachycardia, dysphagia, gastroparesis, and bowel dysfunction.
- Other effects include urinary complications and sexual dysfunction.
-
Radiculopathies
- Commonly affect proximal lumbar (L2-L4) or thoracic (T4-T12) nerve roots.
- Outcomes include lower extremity pain and atrophy (diabetic amyotrophy) or abdominal pain (thoracic polyradiculopathy).
-
Cranial Neuropathies
- Affecting the 3rd cranial nerve can lead to diplopia, ptosis, and anisocoria; the 4th or 6th nerves can cause motor palsies.
-
Mononeuropathies
- Affect individual nerves, leading to conditions like median nerve weakness (carpal tunnel syndrome) and peroneal nerve foot drop.
- May occur simultaneously in multiple locations (mononeuritis multiplex).
Diagnosis
- Symmetric polyneuropathy diagnosed through detection of sensory deficits and decreased ankle reflexes.
- Loss of light touch sensation indicates high risk for foot ulceration.
- 128 Hz tuning fork used to assess vibratory sense on the first toe.
- Electromyography and nerve conduction studies aid in diagnosing various neuropathy forms and excluding other neuropathic causes.
Insulin Resistance
- A condition where insulin-sensitive tissues, like muscle and liver, don't respond well to insulin, causing impaired glucose uptake.
- Key causes include genetic factors, obesity, lack of physical activity, aging, and certain medications like glucocorticoids and beta-blockers.
- Leads to impaired glucose tolerance, hyperinsulinemia, and increases the risk of type 2 diabetes.
Glucagon Regulation
- A hormone from pancreatic alpha cells that elevates blood glucose by promoting glycogenolysis and gluconeogenesis.
- The relationship between insulin and glucagon is crucial; insulin inhibits glucagon, while glucagon can stimulate insulin release.
- Counterregulatory hormones (e.g., cortisol, growth hormone) enhance glucagon secretion during low blood sugar.
- In diabetes, elevated glucagon exacerbates hyperglycemia and disrupts glucose regulation.
Pancreatic Beta-cell Dysfunction
- Refers to the beta cells' inability to produce enough insulin to satisfy glucose needs.
- Potential causes include genetic defects (like maturity-onset diabetes of the young), autoimmune destruction (notably in type 1 diabetes), oxidative stress, and lipotoxicity.
- Results in impaired insulin secretion, leading to hyperglycemia and type 2 diabetes.
Hyperglycemia Mechanisms
- Defined as elevated blood glucose levels exceeding 125 mg/dL.
- Caused by insufficient insulin secretion, insulin resistance, excessive glucose production by the liver, and reduced glucose uptake in tissues.
- Consequences include microvascular and macrovascular complications, such as nephropathy, retinopathy, and cardiovascular disease.
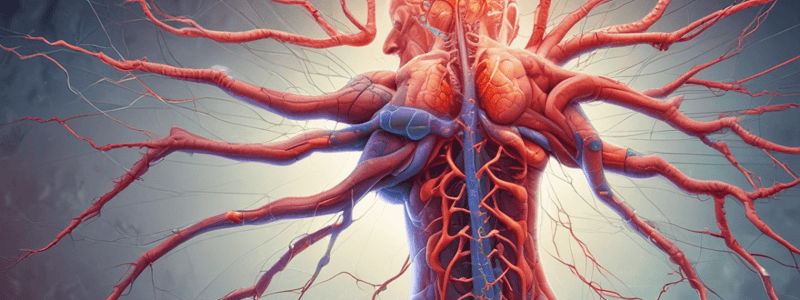
Microvascular Complications
- These complications are related to damage in small blood vessels, predominantly affecting the eyes, kidneys, and nerves.
- Major contributing factors include chronic hyperglycemia, oxidative stress, inflammation, and endothelial dysfunction.
- Consequences include diabetic retinopathy, diabetic nephropathy, diabetic neuropathy, and an increased risk of cardiovascular diseases.
Glucose Metabolism
- Glucose is absorbed from the intestines into the bloodstream.
- Insulin facilitates glucose uptake in muscle and liver cells.
- Glucose is converted to glycogen for short-term storage in the liver and muscles.
- Excess glucose is transformed into fat for long-term energy storage.
Abnormal Glucose Metabolism in Diabetes
- Diabetes is characterized by impaired insulin secretion or resistance to insulin's effects.
- Reduced glucose uptake in cells leads to elevated blood glucose levels.
- The liver produces increased amounts of glucose, contributing to hyperglycemia.
Lipid Profile Management
- Individuals with diabetes often present with elevated triglycerides and low levels of HDL (high-density lipoprotein) cholesterol.
- High levels of LDL (low-density lipoprotein) cholesterol increase cardiovascular risks.
- Dyslipidemia (abnormal lipid levels) is linked to accelerated atherosclerosis and a higher chance of pancreatitis.
Lipid-Lowering Therapies
- Statins are commonly used to lower LDL cholesterol levels.
- Fibrates help reduce triglyceride concentrations in the bloodstream.
- Omega-3 fatty acids are effective in decreasing triglyceride levels as well.
Insulin Resistance
- Insulin resistance is defined as a reduced responsiveness of target cells to insulin, resulting in lower glucose uptake.
- Major causes include obesity, lack of physical activity, genetic factors, and the influence of certain medications.
- Consequences include hyperinsulinemia, hyperglycemia, and an amplified risk of cardiovascular diseases.
Treatment Strategies for Insulin Resistance
- Lifestyle changes, such as diet improvements and increased exercise, are essential for management.
- Insulin sensitizers like metformin can help improve insulin sensitivity.
- GLP-1 receptor agonists are another class of medications that support blood glucose control.
HbA1c Interpretation
- HbA1c, or glycated hemoglobin, provides insight into average blood glucose levels over the previous 2-3 months, serving as a critical measure for diabetes management.
- Normal HbA1c levels indicate good long-term glucose control, while elevated levels suggest poor management and increased risk of complications.
Cranial Neuropathies
- Third cranial nerve involvement may cause diplopia, ptosis, and anisocoria.
- Fourth and sixth cranial nerve lesions lead to motor palsies.
- Mononeuropathies can result in finger weakness (median nerve) or foot drop (peroneal nerve).
- Diabetic patients are susceptible to nerve compression disorders like carpal tunnel syndrome.
- Mononeuropathies can occur in multiple locations (mononeuritis multiplex).
- Mainly affects older adults and often resolve spontaneously over months, unlike nerve compression disorders.
Diagnosis of Neuropathy
- Symmetric polyneuropathy is diagnosed via sensory deficits and diminished ankle reflexes.
- Loss of light touch sensation indicates high risk for foot ulceration.
- Vibratory sense can be evaluated with a 128-Hz tuning fork, typically on the first toe.
- Electromyography and nerve conduction studies are utilized for evaluating neuropathies and differentiating from other conditions like radiculopathy.
Diabetic Neuropathy Types
- Symmetric Polyneuropathy:
- Most common type, affects distal feet and hands (stocking-glove distribution).
- Symptoms include paresthesias, dysesthesias, and painless loss of sensation, leading to foot trauma and various foot complications.
- Small-Fiber Neuropathy:
- Characterized by pain, numbness, and loss of temperature sensation.
- Preserved vibration and position sense; high risk of foot ulcers and neuropathic joint degeneration.
- Predominant Large-Fiber Neuropathy:
- Presents as muscle weakness, loss of vibration and position sense, and absent deep tendon reflexes, leading to atrophy of foot muscles and foot drop.
- Autonomic Neuropathy:
- Manifests through symptoms like orthostatic hypotension, exercise intolerance, gastrointestinal disturbances, urinary issues, and sexual dysfunction.
- Radiculopathies:
- Affects proximal lumbar and thoracic nerve roots causing pain, weakness, and potential atrophy, with issues like diabetic amyotrophy.
Insulin Resistance
- State in which tissues fail to respond adequately to insulin, impairing glucose uptake.
- Caused by genetic factors, obesity, inactivity, age, and certain medications.
- Consequences include hyperinsulinemia, impaired glucose tolerance, and potential progression to type 2 diabetes.
Glucagon Regulation
- Produced by pancreatic alpha cells; it raises blood glucose levels through glycogenolysis and gluconeogenesis.
- Insulin inhibits glucagon secretion; glucose dysregulation occurs when glucagon is inappropriately elevated in diabetes.
Pancreatic Beta-cell Dysfunction
- Characterized by inadequate insulin production to meet glucose needs.
- Causes include genetic defects, autoimmune destruction, oxidative stress, and glucotoxicity.
- Results in impaired insulin secretion, hyperglycemia, and contributes to type 2 diabetes.
Hyperglycemia Mechanisms
- Defined as elevated blood glucose levels (>125 mg/dL).
- Normal glucose metabolism involves absorption, insulin-stimulated uptake, glycogen storage, and fat conversion.
- Abnormal metabolism in diabetes leads to impaired insulin action and increased hepatic glucose production.
Lipid Profile Management
- Dyslipidemia typically involves elevated triglycerides and altered cholesterol levels in diabetes.
- Consequences include heightened cardiovascular risk, accelerated atherosclerosis, and pancreatitis risk.
- Treatments involve statins, fibrates, and omega-3 fatty acids for lipid reduction.
HbA1c Interpretation
- Reflects average blood glucose over the previous 2-3 months.
- Important for monitoring glycemic control in diabetic patients, establishing targets for therapy.
Hyperglycemia Symptoms
- Polyuria, polydipsia, and polyphagia signify excessive urination, thirst, and hunger, respectively.
- Common symptoms also include fatigue, blurred vision, and slow wound healing.
- Severe manifestations may involve nausea, vomiting, abdominal pain, rapid heartbeat, confusion, and seizures.
Diabetic Retinopathy Diagnosis
- Diagnosis can include dilated eye exams, fluorescein angiography, and optical coherence tomography (OCT) for detailed retina imaging.
- Stages of diabetic retinopathy range from mild to advanced:
- Mild non-proliferative diabetic retinopathy (NPDR)
- Moderate NPDR
- Severe NPDR
- Proliferative diabetic retinopathy (PDR)
- Advanced PDR
Kidney Damage Evaluation
- Evaluation methods consist of urine protein testing for albuminuria, estimated glomerular filtration rate (eGFR) assessments, and creatinine clearance tests.
- Chronic kidney disease is categorized into five stages based on eGFR:
- Stage 1: kidney damage with normal/increased eGFR
- Stage 2: mild decrease in eGFR
- Stage 3: moderate decrease in eGFR
- Stage 4: severe decrease in eGFR
- Stage 5: end-stage kidney disease
Foot Ulcer Assessment
- Risk factors for foot ulcers include neuropathy, peripheral artery disease, deformities, and previous occurrences of foot ulcers.
- Assessment techniques include visual inspections, palpation of pedal pulses, sensory testing (monofilament), and ankle-brachial index (ABI) measurement.
Glycated Hemoglobin (HbA1c) Testing
- HbA1c measures average blood glucose levels over the last 2-3 months.
- Recommended target levels for HbA1c are < 7.0% for most and < 6.5% for individuals with a shorter duration of diabetes or no cardiovascular disease.
- Interpretation of results categorizes levels:
- HbA1c < 6.0%: normal
- HbA1c 6.0-6.4%: increased risk of diabetes
- HbA1c ≥ 6.5%: indicates diabetes
Canadian Lab Values
- Normal blood glucose levels are defined as fasting 3.9-5.5 mmol/L and postprandial < 8.0 mmol/L.
- HbA1c should ideally be < 6.0%.
- Lipid levels should be monitored:
- Total cholesterol: < 5.0 mmol/L
- LDL-C: < 2.0 mmol/L
- HDL-C: > 1.0 mmol/L
- Triglycerides: < 1.5 mmol/L
Canadian Lab Values for Diabetes
Glucose Measures
- Fasting Plasma Glucose (FPG):
- Normal levels: less than 5.6 mmol/L
- Impaired fasting glucose (IFG) range: 5.6 to 6.9 mmol/L
- Diabetes diagnosis: 7.0 mmol/L or higher
- 2-hour Oral Glucose Tolerance Test (OGTT):
- Normal levels: less than 7.8 mmol/L
- Impaired glucose tolerance (IGT) range: 7.8 to 11.0 mmol/L
- Diabetes diagnosis: 11.1 mmol/L or higher
Hemoglobin A1c (HbA1c)
- Normal HbA1c levels: less than 6.0%
- Increased risk of diabetes identified by levels between 6.0% and 6.4%
- Diabetes diagnosis indicated by HbA1c of 6.5% or higher
Lipid Profile Analysis
- Total Cholesterol:
- Desirable level: less than 5.0 mmol/L
- Borderline high range: 5.0 to 6.4 mmol/L
- High level: 6.5 mmol/L or higher
- High-Density Lipoprotein (HDL) Cholesterol:
- Low level: less than 1.0 mmol/L
- Normal level: 1.0 mmol/L or greater
- Low-Density Lipoprotein (LDL) Cholesterol:
- Optimal level: less than 2.0 mmol/L
- Near optimal range: 2.0 to 2.9 mmol/L
- Borderline high range: 3.0 to 3.9 mmol/L
- High level: 4.0 mmol/L or greater
- Triglycerides:
- Normal level: less than 1.7 mmol/L
- Borderline high range: 1.7 to 2.2 mmol/L
- High level: 2.3 mmol/L or greater
Blood Glucose Targets
- Fasting blood glucose should maintain levels between 4.0 and 7.0 mmol/L for optimal management.
- Blood glucose levels before meals should also range from 4.0 to 7.0 mmol/L, ensuring consistent control.
- Two hours post-meal, glucose levels should be between 5.0 and 10.0 mmol/L to reflect appropriate postprandial management.
- At bedtime, a target range of 5.0 to 10.0 mmol/L is recommended to prevent nighttime hypoglycemia or hyperglycemia.
Hemoglobin A1c (HbA1c)
- The target for HbA1c is set at ≤7.0%, which indicates effective long-term blood glucose control.
- HbA1c results reflect an individual's average blood glucose levels over the preceding 2 to 3 months, aiding in overall diabetes management assessment.
Lipid Profile
- A comprehensive lipid profile is crucial for diabetes management, providing insight into cardiovascular health expected levels for total cholesterol and other lipid components are essential for risk assessment.
Blood Glucose Levels
- Fasting plasma glucose (FPG) measures fasting blood sugar levels.
- Normal range is less than 5.6 mmol/L.
- Impaired fasting glucose (IFG) is between 5.6 and 6.9 mmol/L.
- Diagnosis of diabetes occurs at levels of 7.0 mmol/L or higher.
- The 2-hour oral glucose tolerance test (OGTT) assesses blood sugar after glucose intake.
- Normal results are below 7.8 mmol/L.
- Impaired glucose tolerance (IGT) ranges from 7.8 to 11.0 mmol/L.
- Diabetes is diagnosed at 11.1 mmol/L or above.
Hemoglobin A1c (HbA1c)
- HbA1c indicates average blood glucose levels over the past 2-3 months.
- Normal HbA1c values are below 6.0%.
- Prediabetes is indicated by an HbA1c of 6.0% to 6.4%.
- Diabetes is diagnosed with HbA1c levels of 6.5% or higher.
Lipid Profile
- Total cholesterol levels are critical for cardiovascular health.
- Desirable cholesterol level is under 5.0 mmol/L.
- Borderline high is 5.0 to 6.4 mmol/L.
- High cholesterol is defined as 6.5 mmol/L or higher.
- Low-density lipoprotein (LDL) cholesterol detail:
- Optimal level is less than 2.0 mmol/L.
- Near optimal is between 2.0 and 2.9 mmol/L.
- Borderline high is 3.0 to 3.4 mmol/L.
- High LDL is 3.5 mmol/L or above.
- High-density lipoprotein (HDL) cholesterol indicates protective cardiovascular effects.
- Levels below 1.0 mmol/L are considered low.
- Normal HDL ranges from 1.0 to 1.9 mmol/L.
- High HDL is considered at levels of 2.0 mmol/L or more.
- Triglycerides reflect current fat storage and energy in the body.
- Normal triglyceride levels are under 1.7 mmol/L.
- Borderline high is categorized as 1.7 to 2.2 mmol/L.
- High triglyceride levels are 2.3 mmol/L or greater.
Urine Albumin-to-Creatinine Ratio (UACR)
- UACR evaluates kidney function and protein levels in urine.
- Normal UACR is less than 2.0 mg/mmol.
- Microalbuminuria indicates levels between 2.0 and 20.0 mg/mmol.
- Macroalbuminuria is defined as levels of 20.1 mg/mmol or higher.
Role of Diabetic Nurses
- Specialized in caring for diabetes mellitus patients
- Essential for diabetes management, education, and complication prevention
Responsibilities
- Assess diabetes status to create personalized care plans
- Administer medications like insulin; monitor blood glucose levels
- Teach self-care techniques: glucose monitoring, insulin injections, foot care
- Advise on healthy lifestyle choices, focusing on diet and exercise
- Identify and address diabetes complications such as neuropathy and nephropathy
- Collaborate with healthcare professionals for holistic patient care
Skills and Qualifications
- Must be a Registered Nurse (RN) with a bachelor's degree in nursing or related area
- Certification in diabetes education (CDE) or equivalent specialty is preferred
- Strong communication and instruction skills are crucial
- Capable of independent work as well as teamwork in healthcare settings
- Comprehensive knowledge of diabetes management standards and ongoing research
Settings
- Employed in diverse environments: hospitals, clinics, community health organizations
- Also found in private practices and home health care contexts
Benefits of Diabetic Nurses
- Contribute to better patient outcomes and enhanced quality of life
- Improve patient education, leading to empowered and informed patients
- Help lower hospitalization rates and associated healthcare expenses
- Foster higher patient satisfaction and adherence to prescribed treatment plans
- Provide vital support to healthcare teams and primary care physicians
Types of Diabetes
- Type 1 Diabetes: Autoimmune disorder leading to destruction of pancreatic beta cells, resulting in total insulin deficiency. Commonly diagnosed in childhood or adolescence.
- Type 2 Diabetes: Characterized by insulin resistance and impaired secretion, leading to relative insulin deficiency. Generally develops in adulthood, often linked with obesity and lack of physical activity.
- Gestational Diabetes: Occurs during pregnancy, particularly in the second or third trimester. Insulin resistance is the main cause, with blood sugar levels typically normalizing afterward.
- LADA (Latent Autoimmune Diabetes in Adults): An autoimmune condition resembling Type 1 diabetes, occurring in individuals over 30. It involves insulin deficiency along with autoimmune markers.
- MODY (Maturity-Onset Diabetes of the Young): Genetic mutations affect insulin secretion, usually diagnosed in young adulthood. Patients display impaired insulin secretion while maintaining normal insulin sensitivity.
Risk Factors for Developing Diabetes
- Genetic Predisposition: Increased likelihood if there is a family history of diabetes.
- Obesity: Particularly central obesity around the abdomen raises risk.
- Physical Inactivity: Sedentary lifestyles contribute significantly to diabetes development.
- Age: Risk escalates after 45 years of age.
- Ethnicity: Higher prevalence in certain groups, notably African Americans, Hispanics/Latinos, and American Indians.
- History of Gestational Diabetes: Previous gestational diabetes increases future risk of Type 2 diabetes.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS face a heightened risk for Type 2 diabetes.
Environmental Factors Contributing to Diabetic Etiology
- Diet: High-calorie, high-fat, and sugar-laden foods correlate with increased diabetes risk.
- Lack of Physical Activity: Sedentary behaviors further exacerbate the probability of developing diabetes.
- Stress: Chronic stress can lead to insulin resistance and worsen glucose metabolism.
- Sleep Disturbances: Conditions like sleep apnea contribute to elevated diabetes risk.
- Pollutants: Exposure to pollutants such as pesticides and air pollution has been associated with a higher incidence of diabetes.
Hypoglycemia Management
- Common complication of diabetes, especially with insulin and sulfonylureas.
- Signs include tremors, sweating, hunger, dizziness, confusion, and in severe cases, seizures.
- Management involves administering 15-20 grams of rapid-acting glucose, repeating every 15 minutes until normal blood glucose is achieved.
- In unconscious patients, glucagon injection may be required.
Nurse-patient Communication
- Effective communication is vital for diabetic patients' understanding of their condition and self-care.
- Key communication strategies include using clear language, active listening, demonstrating empathy, and involving patients through open-ended questions.
- Barriers to effective communication can include language differences, low health literacy, cognitive impairments, and emotional distress.
Critical Thinking in Nursing Practice
- Critical thinking enables nurses to make informed decisions and provide high-quality patient care.
- Essential elements include analyzing data, identifying patterns, evaluating evidence, considering viewpoints, and reflecting on personal biases.
- In diabetes care, critical thinking is applied by assessing individual patient factors, recognizing medication interactions, and creating tailored care plans.
Medication Adherence
- Non-adherence to medication is a major issue among diabetics, contributing to poor glycemic control and increased complications.
- Influencing factors include the complexity of medication regimens, cost, side effects, and communication with healthcare providers.
- Strategies to enhance adherence include simplifying medication regimens, providing education, encouraging patient empowerment, and monitoring for side effects.
Bacterial Adhesion and Colonization
- Bacterial adhesion is the capacity of bacteria to attach to uroepithelial cells.
- Colonization refers to the establishment and growth of bacterial communities on these cells.
- Key bacterial adhesins essential for attachment include:
- FimH associated with type 1 fimbriae
- PapG associated with P fimbriae
- Dr adhesin linked to Dr fimbriae
- Uroepithelial cells possess specific receptors that facilitate bacterial binding.
- Biofilm formation during colonization enhances bacterial survival and persistence, complicating treatment.
- Biofilms contribute to reduced antibiotic effectiveness and promote inflammation and tissue damage.
Inflammation and Immune Response
- Urinary tract infections (UTIs) activate innate immune mechanisms:
- Toll-like receptors (TLRs) and NOD-like receptors (NLRs) initiate immune response.
- Pro-inflammatory cytokines like IL-6, IL-8, and TNF-α are produced.
- Immune cells such as neutrophils and macrophages are recruited to the site.
- The adaptive immune response features:
- Activation of T and B cells.
- Antibody production targeting bacterial antigens.
- Inflammation from UTIs can result in tissue damage, fibrosis, and scarring.
- Symptoms due to immune response include:
- Dysuria (painful urination)
- Increased frequency and urgency of urination
- Hematuria (presence of blood in urine)
Risk Factors and Predisposition
- Demographic Factors:
- Females are at higher risk due to having a shorter urethra and closer proximity to the anus.
- The elderly population faces increased susceptibility due to weakened immunity and underlying health issues.
- Behavioral Factors:
- Sexual activity can elevate UTI risk through potential bacterial transfer.
- Inadequate hygiene practices can lead to higher risks of bacterial introduction.
- Anatomical Factors:
- Vesicoureteral reflux (VUR) can allow bacteria to ascend the urinary tract, increasing UTI likelihood.
- Urinary tract obstructions can result in stasis, promoting bacterial growth.
- Medical Conditions:
- Diabetes compromises immune response and can lead to urinary retention, heightening UTI risk.
- Neurological disorders may result in complications like urinary retention and catheter use, further increasing susceptibility.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Learn about the causes and effects of diabetic neuropathy, including symmetric polyneuropathy, and its symptoms on nerve function. Understand the impact on the distal feet and hands.