Podcast
Questions and Answers
According to CDC data from 2020, which age group has the highest incidence rate of diabetes?
According to CDC data from 2020, which age group has the highest incidence rate of diabetes?
- \≥65
- 18-44
- Total
- 45-64 (correct)
What percentage of adults with diabetes mellitus (DM) are estimated to be unaware that they have the disease?
What percentage of adults with diabetes mellitus (DM) are estimated to be unaware that they have the disease?
- 10%
- 23% (correct)
- 34%
- 50%
What is the most common problem associated with diabetes that leads to hospitalization?
What is the most common problem associated with diabetes that leads to hospitalization?
- Cardiovascular disease
- Kidney failure
- Foot disease/ulcer (correct)
- Retinopathy
Individuals with diabetes mellitus have an amputation rate that is how many times greater than individuals without diabetes?
Individuals with diabetes mellitus have an amputation rate that is how many times greater than individuals without diabetes?
According to the Centers for Disease Control and Prevention (CDC), what percentage range of non-traumatic lower extremity amputations (LE) in the United States, that are attributable to diabetes, could potentially be avoided with comprehensive diabetic foot care programs?
According to the Centers for Disease Control and Prevention (CDC), what percentage range of non-traumatic lower extremity amputations (LE) in the United States, that are attributable to diabetes, could potentially be avoided with comprehensive diabetic foot care programs?
Which of the following factors contributes to foot breakdown in individuals with diabetes?
Which of the following factors contributes to foot breakdown in individuals with diabetes?
The narrowing of arteries due to fatty plaque deposits in peripheral arterial disease (PAD) leads to:
The narrowing of arteries due to fatty plaque deposits in peripheral arterial disease (PAD) leads to:
How does the severity of peripheral arterial disease (PAD) relate to the onset of diabetes mellitus (DM)?
How does the severity of peripheral arterial disease (PAD) relate to the onset of diabetes mellitus (DM)?
The Ankle-Brachial Index (ABI) is calculated by:
The Ankle-Brachial Index (ABI) is calculated by:
What Ankle Brachial Index (ABI) range is considered normal?
What Ankle Brachial Index (ABI) range is considered normal?
While Ankle Brachial Index (ABI) is a useful tool, it might not be as reliable in diabetic patients because:
While Ankle Brachial Index (ABI) is a useful tool, it might not be as reliable in diabetic patients because:
What does an angiogram reveal about arterial occlusion?
What does an angiogram reveal about arterial occlusion?
What skin change is commonly associated with peripheral arterial disease (PAD)?
What skin change is commonly associated with peripheral arterial disease (PAD)?
Peripheral neuropathy can lead to which of the following?
Peripheral neuropathy can lead to which of the following?
Which of the following best describes the presentation of peripheral neuropathy?
Which of the following best describes the presentation of peripheral neuropathy?
What Semmes-Weinstein monofilament indicates a loss of protective sensation in the foot?
What Semmes-Weinstein monofilament indicates a loss of protective sensation in the foot?
Applying a Semmes Weinstein Monofilament involves:
Applying a Semmes Weinstein Monofilament involves:
Autonomic neuropathy can lead to deficits in sweating, which results in which of the following skin changes?
Autonomic neuropathy can lead to deficits in sweating, which results in which of the following skin changes?
According to the information provided, what type of pressure applied to insensitive skin can lead to injury?
According to the information provided, what type of pressure applied to insensitive skin can lead to injury?
In the development of a hammer toe deformity, what change occurs with ankle dorsiflexion?
In the development of a hammer toe deformity, what change occurs with ankle dorsiflexion?
Limited joint mobility in patients with diabetes can be indicated by:
Limited joint mobility in patients with diabetes can be indicated by:
Which symptom is associated with acute Charcot arthropathy?
Which symptom is associated with acute Charcot arthropathy?
What is the correct sequence of the developmental stages of Charcot arthropathy?
What is the correct sequence of the developmental stages of Charcot arthropathy?
What percentage of partial foot amputations develop a risk for more amputation?
What percentage of partial foot amputations develop a risk for more amputation?
What is a key factor to examine when screening a patient for diabetic foot problems?
What is a key factor to examine when screening a patient for diabetic foot problems?
According to the Wagner Scale, a grade 2 ulcer indicates:
According to the Wagner Scale, a grade 2 ulcer indicates:
According to the University of Texas Diabetic Foot Ulcer Classification, a wound that has penetrated a capsule or bone, but is not ischemic or infected, would be classified as what grade?
According to the University of Texas Diabetic Foot Ulcer Classification, a wound that has penetrated a capsule or bone, but is not ischemic or infected, would be classified as what grade?
During a patient examination, a monofilament reading of >5.07 indicates:
During a patient examination, a monofilament reading of >5.07 indicates:
It’s important to assess the quality of motion at the joints of the foot during a patient examination. Which of the following would be used to assess the quality of motion of the joints?
It’s important to assess the quality of motion at the joints of the foot during a patient examination. Which of the following would be used to assess the quality of motion of the joints?
What is an important consideration regarding the material of shoes recommended to patients with diabetic foot issues?
What is an important consideration regarding the material of shoes recommended to patients with diabetic foot issues?
Which of the following is a recommendation from the National Diabetes Education Program Risk Categories and Management Guidelines for High Risk Patients?
Which of the following is a recommendation from the National Diabetes Education Program Risk Categories and Management Guidelines for High Risk Patients?
Why implement a “High Risk Feet” sticker on a patient's medical record?
Why implement a “High Risk Feet” sticker on a patient's medical record?
Which of the following is a key aspect of patient education for diabetic foot care, according to the IWGDF guidelines?
Which of the following is a key aspect of patient education for diabetic foot care, according to the IWGDF guidelines?
What recommendation should diabetic patients follow regarding daily foot care?
What recommendation should diabetic patients follow regarding daily foot care?
When is the ideal time of day to shop for shoes to accommodate foot swelling?
When is the ideal time of day to shop for shoes to accommodate foot swelling?
The formula PRESSURE = FORCE/AREA is useful to remind us:
The formula PRESSURE = FORCE/AREA is useful to remind us:
In Category 1 for footwear recommendations, individuals have:
In Category 1 for footwear recommendations, individuals have:
Total Contact Casting is utilized for treating:
Total Contact Casting is utilized for treating:
High ulcer recurrence rates occur within:
High ulcer recurrence rates occur within:
What percentage of the US population was estimated to have diabetes in 2020?
What percentage of the US population was estimated to have diabetes in 2020?
Which of the following is a potential consequence of narrowed arteries due to peripheral arterial disease (PAD)?
Which of the following is a potential consequence of narrowed arteries due to peripheral arterial disease (PAD)?
How is the Ankle-Brachial Index (ABI) affected in diabetic patients with calcified tibial arteries?
How is the Ankle-Brachial Index (ABI) affected in diabetic patients with calcified tibial arteries?
What visual skin change is most indicative of peripheral arterial disease (PAD)?
What visual skin change is most indicative of peripheral arterial disease (PAD)?
Which of the following is associated with autonomic neuropathy?
Which of the following is associated with autonomic neuropathy?
According to Dr. Paul Brand's research, what type of pressure applied to insensitive skin is most likely to cause injury?
According to Dr. Paul Brand's research, what type of pressure applied to insensitive skin is most likely to cause injury?
What clinical sign indicates limited joint mobility in patients with diabetes?
What clinical sign indicates limited joint mobility in patients with diabetes?
Which of the following is a characteristic of the inflammatory stage (Stage 0) of acute Charcot arthropathy?
Which of the following is a characteristic of the inflammatory stage (Stage 0) of acute Charcot arthropathy?
According to the IWGDF guidelines, what is a common cause of ulceration?
According to the IWGDF guidelines, what is a common cause of ulceration?
What is the current ADA goal for HbA1c levels in diabetic control?
What is the current ADA goal for HbA1c levels in diabetic control?
Why is it important to assess skin changes as part of patient screening for diabetic foot problems?
Why is it important to assess skin changes as part of patient screening for diabetic foot problems?
Which of the following skin changes is not typically associated with neuropathic wounds?
Which of the following skin changes is not typically associated with neuropathic wounds?
When assessing vascular status in patients with diabetic foot ulcers, which finding would be more indicative of arterial disease rather than neuropathy?
When assessing vascular status in patients with diabetic foot ulcers, which finding would be more indicative of arterial disease rather than neuropathy?
What is the primary recommendation for the management for Category 1 footwear?
What is the primary recommendation for the management for Category 1 footwear?
Which of the following is the goal for activity guidelines in patients with diabetes?
Which of the following is the goal for activity guidelines in patients with diabetes?
Which characteristic is consistent with a neuropathic foot?
Which characteristic is consistent with a neuropathic foot?
What recommendation should you make to a patient with insensitive feet who likes to garden?
What recommendation should you make to a patient with insensitive feet who likes to garden?
What advice should be given about nail care to a patient with diabetic foot?
What advice should be given about nail care to a patient with diabetic foot?
What should a patient know about choosing appropriate socks if they have diabetic foot?
What should a patient know about choosing appropriate socks if they have diabetic foot?
What footwear characteristic is important for diabetic foot patients?
What footwear characteristic is important for diabetic foot patients?
If a patient presents with a foot ulcer, where should they NOT apply moisturizer?
If a patient presents with a foot ulcer, where should they NOT apply moisturizer?
The formula PRESSURE = FORCE/AREA reminds us that to reduce the risk of foot ulcers, a clinician should aim to:
The formula PRESSURE = FORCE/AREA reminds us that to reduce the risk of foot ulcers, a clinician should aim to:
A patient with no protective sensation, no history of ulcers, and no foot deformity would fall into which footwear category?
A patient with no protective sensation, no history of ulcers, and no foot deformity would fall into which footwear category?
When is Total Contact Casting most effective?
When is Total Contact Casting most effective?
Following initial ulcer healing, when is the greatest risk for ulcer recurrence?
Following initial ulcer healing, when is the greatest risk for ulcer recurrence?
Peripheral neuropathy affects what components?
Peripheral neuropathy affects what components?
What percentage have symptoms of Peripheral neuropathy after 25 years?
What percentage have symptoms of Peripheral neuropathy after 25 years?
What pressures are seen with walking in patients?
What pressures are seen with walking in patients?
What occurs with MTPJ flexion during the development of hammer toe?
What occurs with MTPJ flexion during the development of hammer toe?
What should patients avoid to desensitize feet?
What should patients avoid to desensitize feet?
What are the most common amputation causes?
What are the most common amputation causes?
According to Table 1, what is the difference in Frequency between LOPS or PAD and LOPS + PAD, or PAD+ foot deformity?
According to Table 1, what is the difference in Frequency between LOPS or PAD and LOPS + PAD, or PAD+ foot deformity?
What is a key education point that should told to patients?
What is a key education point that should told to patients?
Why is Total Contact Casting indicated?
Why is Total Contact Casting indicated?
How often should you change shoes once or twice daily?
How often should you change shoes once or twice daily?
According to the CDC, how has the percentage of the US population with diabetes changed between 2015 and 2020?
According to the CDC, how has the percentage of the US population with diabetes changed between 2015 and 2020?
What is the potential impact of comprehensive diabetic foot care programs, according to the CDC?
What is the potential impact of comprehensive diabetic foot care programs, according to the CDC?
How does peripheral arterial disease (PAD) directly contribute to the risk of foot breakdown in individuals with diabetes?
How does peripheral arterial disease (PAD) directly contribute to the risk of foot breakdown in individuals with diabetes?
Which vascular change is most indicative of PAD when the foot is in a dependent position?
Which vascular change is most indicative of PAD when the foot is in a dependent position?
A patient with diabetes mentions that their foot pain is worse at night. How does this correlate with peripheral neuropathy?
A patient with diabetes mentions that their foot pain is worse at night. How does this correlate with peripheral neuropathy?
Why are patients unable to sense a 5.07 Semmes-Weinstein monofilament at a 10x higher risk of developing foot ulcers?
Why are patients unable to sense a 5.07 Semmes-Weinstein monofilament at a 10x higher risk of developing foot ulcers?
In performing a monofilament test, how is the monofilament applied to the patient's foot?
In performing a monofilament test, how is the monofilament applied to the patient's foot?
How does autonomic neuropathy contribute to skin changes that increase the risk of foot problems?
How does autonomic neuropathy contribute to skin changes that increase the risk of foot problems?
According to the concept of injury mechanisms related to pressure, what types of pressure most likely causes injury to insensitive skin?
According to the concept of injury mechanisms related to pressure, what types of pressure most likely causes injury to insensitive skin?
In the development of a hammer toe deformity, what happens to the intrinsic muscles?
In the development of a hammer toe deformity, what happens to the intrinsic muscles?
What clinical sign suggests limited joint mobility, increasing the risk of foot complications in patients with diabetes?
What clinical sign suggests limited joint mobility, increasing the risk of foot complications in patients with diabetes?
During the inflammatory stage of acute Charcot arthropathy, what signs are typically observed?
During the inflammatory stage of acute Charcot arthropathy, what signs are typically observed?
What is Stage 1 of Charcot Arthropathy called?
What is Stage 1 of Charcot Arthropathy called?
What is the likelihood of more amputation after a partial foot amputation?
What is the likelihood of more amputation after a partial foot amputation?
According to the IWGDF guidelines, what is often the cause of ulceration in insensitive feet?
According to the IWGDF guidelines, what is often the cause of ulceration in insensitive feet?
What is the ADA goal for HBA1c levels in diabetic control?
What is the ADA goal for HBA1c levels in diabetic control?
What are non-modifiable factors to consider when assessing a patient during screening for foot problems?
What are non-modifiable factors to consider when assessing a patient during screening for foot problems?
After incision has healed in patients with a transmetatarsal amputation (TMA), what type of footwear is recommended?
After incision has healed in patients with a transmetatarsal amputation (TMA), what type of footwear is recommended?
What are causes for amputation?
What are causes for amputation?
Following ulcer healing, when is the greatest risk of ulcer recurrence?
Following ulcer healing, when is the greatest risk of ulcer recurrence?
Flashcards
Peripheral Arterial Disease (PAD)
Peripheral Arterial Disease (PAD)
Narrowing of arteries due to fatty plaque deposits, leading to reduced circulation.
Decreased Blood Supply in PAD
Decreased Blood Supply in PAD
Decreased blood supply to muscles, especially during activity, resulting in reduced oxygen supply.
Ischemia in PAD
Ischemia in PAD
Condition in PAD where ischemia leads to lactic acid buildup, causing pain.
Posterior Tibial and Dorsalis Pedis Pulses
Posterior Tibial and Dorsalis Pedis Pulses
Common, but with poor reliability. Assesses the presence/absence of pulses in the feet.
Signup and view all the flashcards
Ankle Brachial Index (ABI)
Ankle Brachial Index (ABI)
ABI is the ratio of systolic blood pressure at the ankle to brachial systolic pressure.
Signup and view all the flashcards
Normal ABI Value
Normal ABI Value
Normal ABI range; gold standard for diagnosing Peripheral Arterial Disease (PAD).
Signup and view all the flashcards
Angiogram
Angiogram
Diagnostic procedure to locate and determine the degree of occlusion from plaques in an artery.
Signup and view all the flashcards
Ischemic Pain
Ischemic Pain
Occurs due to narrowed arteries, causing reduced blood flow and oxygen to tissues.
Signup and view all the flashcards
Peripheral Neuropathy
Peripheral Neuropathy
Includes motor, sensory, and autonomic components, affecting foot muscles, sensation, and sweating.
Signup and view all the flashcards
Muscular Wasting in Neuropathy
Muscular Wasting in Neuropathy
Muscle wasting of intrinsic foot muscles due to neuropathy.
Signup and view all the flashcards
Sensory Loss in Neuropathy
Sensory Loss in Neuropathy
Decreased ability to feel touch, vibration, temperature, and pain due to nerve damage.
Signup and view all the flashcards
Semmes Weinstein Monofilaments
Semmes Weinstein Monofilaments
A tactile test using nylon monofilaments to assess protective sensation in the foot.
Signup and view all the flashcards
5.07 Monofilament Test
5.07 Monofilament Test
Loss of protective sensation; indicates increased risk of foot ulcers and amputation.
Signup and view all the flashcards
Autonomic Neuropathy Skin Changes
Autonomic Neuropathy Skin Changes
Loss of sweating, leading to dry and cracked feet, increasing risk of fungal infections.
Signup and view all the flashcards
Excessive pressures to insensitive skin
Excessive pressures to insensitive skin
Can result from low pressures over long durations, high pressures over short durations or moderate pressures repeated many times.
Signup and view all the flashcards
Foot Deformities
Foot Deformities
Factors such as hammer toes and prominent metatarsal heads leading to high pressures and ulcers.
Signup and view all the flashcards
Limited Joint Mobility
Limited Joint Mobility
Associated with several joint problems, including hands, wrists, shoulders, and feet, impacting mobility.
Signup and view all the flashcards
Charcot Stage 0
Charcot Stage 0
Inflammatory period with erythema, warmth, swelling, and pain; no radiographic changes.
Signup and view all the flashcards
Charcot Stage 1
Charcot Stage 1
Fragmentation/destruction period with bone and cartilage breakdown, joint capsule distension, and deformity.
Signup and view all the flashcards
Charcot Stage 2
Charcot Stage 2
Coalescence, diminishing inflammation, callus formation, and fracture consolidation.
Signup and view all the flashcards
Charcot Stage 3
Charcot Stage 3
Reconstruction with bony ankylosis, hypertrophic bone formation, and fixed deformity or persistent instability.
Signup and view all the flashcards
Extrinsic Footwear Factors
Extrinsic Footwear Factors
Poorly fitting shoes and walking barefoot, common causes of ulceration in insensitive feet.
Signup and view all the flashcards
Diabetic Control Levels
Diabetic Control Levels
Normal is less than 6.5%. ADA treatment goal is < 7.0%.
Signup and view all the flashcards
Patient Screening
Patient Screening
Checking for diabetes history, vascular disease, neuropathy, skin changes, and foot deformities.
Signup and view all the flashcards
Patient Examination: Wounds
Patient Examination: Wounds
Examine the wound for edema, drainage, and staging of diabetic foot ulcer using Wagner or Texas San Antonio Scale.
Signup and view all the flashcards
Patient History
Patient History
Ask about past ulcers, vascular disease, neuropathy, and other diabetic complications.
Signup and view all the flashcards
Sensation & PAD Assessment
Sensation & PAD Assessment
Assessing sensation using Semmes Weinstein monofilaments and measures of PAD.
Signup and view all the flashcards
Functional Assessment
Functional Assessment
Check functional ability, heel/toe raises, and vascularity to plan treatment.
Signup and view all the flashcards
Footwear Assessment
Footwear Assessment
Assess footwear for length, width, depth, material, and construction to avoid problems.
Signup and view all the flashcards
Low-Risk Management Guidelines
Low-Risk Management Guidelines
Includes annual foot exam, appropriate footwear, and preventive self-care education.
Signup and view all the flashcards
High-Risk Management
High-Risk Management
Patient needs annual exams, foot inspections, self-care education, plus specialist referral.
Signup and view all the flashcards
Patient Education Key Points
Patient Education Key Points
Key components include daily foot inspections, early detection, and shoe wear.
Signup and view all the flashcards
Daily foot inspection and care
Daily foot inspection and care
Includes inspecting feet, monofilament, shoes, loosening, wash, feet, avoid heat.
Signup and view all the flashcards
Patient Education shoe fitting
Patient Education shoe fitting
Shoe fitting which includes shoe attributes for longest toe and light materials
Signup and view all the flashcards
Shoe Fitting
Shoe Fitting
Leather, suede, tracing, swelling.
Signup and view all the flashcards
Ulcer Management Scheme
Ulcer Management Scheme
Wound care, off-loading pressure, remodeling support, and protective footwear.
Signup and view all the flashcards
Total Contact Casting
Total Contact Casting
Helps wounds heal in 42 days
Signup and view all the flashcards
Removable Pressure Relief Walker
Removable Pressure Relief Walker
Comparable to TCC with pressure reduction.
Signup and view all the flashcards
Cutout of healing
Cutout of healing
Used for foot ulcers
Signup and view all the flashcards
Physical state
Physical state
In a patient ability to increase activity in the feet.
Signup and view all the flashcards
Surgeon General and Diabetes
Surgeon General and Diabetes
10.000 steps per day
Signup and view all the flashcards
Surgical Interventions include
Surgical Interventions include
Include diabetes, vascular disease, etc..
Signup and view all the flashcards
TMA
TMA
Heel strike shoe and studies showing use of shoes.
Signup and view all the flashcards
Key protection
Key protection
Screen diabetic foot for risk factors!
Signup and view all the flashcardsStudy Notes
Objectives
- Learners should be able to describe potential injury mechanisms for the insensitive foot.
- Based on patient characteristics, individuals should be able to choose physical therapy management for an insensitive foot, including footwear prescriptions and examination components.
Diabetes and Diabetic Foot Incidence
- In the US, the CDC reported that in 2015, 30.3 million or 9.4% of the population had diabetes.
- In 2020, that number increased to 34.2 million or 10.5% of the population.
- Twenty-three percent of adults with DM did not know or report they had the disease.
- Foot disease/ulcer is a common problem leading to hospitalization.
- 34% of patients with DM develop an ulcer during their lifetime.
- The annual incidence of foot ulcers in the non-diabetic population is approximately 2%.
- Amputation rates are 10-13 times higher than in controls.
- 50% of lower extremity amputations could be prevented.
- The CDC reports that 45% to 85% of non-traumatic lower extremity amputations in the US attributable to diabetes could have been avoided with proper foot care programs.
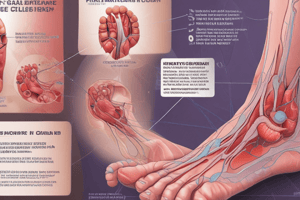
Contributing Factors to Foot Breakdown
- Peripheral Arterial Disease (PAD)
- Peripheral Neuropathy
- Joint Deformity (limited joint mobility)
- Physical stresses
Peripheral Arterial Disease (PAD)
- Arteries narrow from fatty plaque deposits, decreasing circulation.
- Muscles require decreased blood supply, especially during activity, which decreases the oxygen supply.
- Ischemia occurs, leading to excessive lactic acid accumulation and pain.
- Patients with more severe PAD may experience earlier onset of Diabetes Mellitus (DM).
- Distal vessels are affected
- There is a greater than 4x incidence in DM.
- Those with a 20-year duration of DM have a 45% prevalence.
PAD Testing
- Common reliability tests include posterior tibial and dorsalis pedis pulses, but these have poor reliability.
- The relative risk is 1.90 if absent or present.
- Ankle Brachial Index (ABI) and Angiogram are more reliable.
- ABI is the ratio of systolic blood pressure at the ankle to the brachial systolic pressure.
- Ankle Systolic Blood Pressure is taken using the posterior tibial artery or dorsalis pedis with a Doppler.
- ABI is the gold standard for diagnosing PAD, with 95% sensitivity and 99% specificity.
- Normal ABI is >0.9 to <1.3
- <.8 is problematic, < .4 may lead to wound healing issues.
- ABI does not work as well in diabetic patients with calcified tibial arteries due to falsely high values of >1.3, which is a problem.
- Angiograms locate and determine how much occlusion from plaques exist in the artery.
- Dye is injected in the artery, and an x-ray of the blood vessels determines the extent and location of the occlusion.
Other Effects of PAD
- Ischemic pain
- Visual changes in the skin such as dry skin, thickened nails, wounds distally, and poor wound healing.
- Rubor of dependency
Neuropathy
- Peripheral neuropathy includes motor, sensory, and autonomic components.
- It involves muscular wasting of intrinsic foot muscles.
- Sensory deficits lead to decreased touch, vibration sense, proprioception, temperature, and pain sensation.
- Pain may worsen at night or at rest, burning, tingling, and progressing to no pain.
- Distal and symmetric polyneuropathy can involve stocking-glove presentation that involves toes and progresses to feet and lower extremities.
- Often, there is no pain or subjective complaints.
- 50% have symptoms after 25 years with DM.
- The Semmes Weinstein Monofilaments test measures peripheral neuropathy.
- A reading of 5.07 indicates a loss of protective sensation (~10 grams).
- 4.17 is intact and >6.10 is essentially absent.
- Patients unable to sense 5.07 SW monofilament were 10 times more likely to develop foot ulcers and 17 times more likely to require amputation.
- The Semmes Weinstein Monofilaments test should be applied for 1 second on and 1 second off, applying enough pressure for the monofilament to bend.
- Deficits in sweating can lead to dry, cracking feet.
- Other symptoms involve deficits in vascular/thermoregulation.
- Fungal infections can develop.
- Lotion is used
Mechanisms of Injury
- Excessive pressures can lead to injury of insensitive skin.
- Low pressures for long durations, high pressures for short durations, or moderate pressures repeated many times can cause injury.
- Dr. Paul Brand researched Hanson's Disease.
- The Physical Stress Theory (MJM et al. 2002) also relates to injury mechanisms.
- Neuropathy and minor trauma can lead to amputation.
- Excessive stress to the plantar foot contributes to injuries.
- High pressure (1,300 PSI) with low duration, low pressure (5-8 psi) with long duration (6-8 hours), and moderate pressure (40-70 PSI) repeated can all cause injury.
Foot Deformities
- Hammer toes and prominent metatarsal heads are associated with high pressures and ulcers at the dorsal Interphalangeal joints and plantar Metatarsophalangeal joints.
- Development of hammer toe deformity involves decreased ankle dorsiflexion, decreased intrinsic muscle function, decreased MTPJ flexion, and increased MTPJ extension movement pattern.
- Claw toes are also considered a foot deformity.
Limited Joint Mobility
- It may indicate a systematic problem and multiple joint involvement, including hands, wrists, shoulders, ankle STJ, and MTPs.
- Positive Prayer Sign
- Advanced Glycated End Products (AGEs)
- The First MTP can cause Hallux limitus and an ulcer on the 1st toe.
- The Subtalar joint can cause a forefoot ulcer.
- The ankle joint leads to a forefoot ulcer.
Acute Charcot Arthropathy
- Neuropathic bone destruction can cause swelling, redness, heat, and may not have pain.
- Immobilization is needed because there is a risk for skin breakdown and deformity.
- Stage 0: Inflammatory period - response to injury, no radiographic changes, onset of erythema, warmth, swelling, pain;
- Stage 1: Fragmentation/destruction period – fragmentation of subchondral bone and cartilage, distension of joint capsule and ligamentous laxity, joint subluxation/dislocation with deformity;
- Stage 2: Coalescence – diminishing inflammation, absorption of cartilaginous and subchondral debris, formation of bone callus, and consolidation of fractures;
- Stage 3: Reconstruction - bony ankylosis, hypertrophic bone formation, fixed deformity, or persistent instability.
Partial Foot Amputation
- Higher pressure is placed on the residuum
- More likely to develop an ulcer on the residuum
- 30% develop a risk for more amputation
Extrinsic Factors of Footwear
- Poor fitting shoes and walking barefoot with insensitive feet are common causes of ulceration
Other Factors
- Diabetic control: HbA1c normal range <6.5% with the current ADA goal is <7.0
- Diet and nutrition consult
Patient Screening
- Check for diabetes or prediabetes history
- Vascular disease: check pulse and look for skin changes.
- Neuropathy: inability to sense the 5.07 monofilament.
- Assess skin changes in the Autonomic Nervous System.
- Foot deformities such as hammer toe, claw toe, prominent metatarsal heads, partial foot amputation, Charcot, and bunions.
- Ulcer: blister, gangrene.
Patient Examination Considerations
- It is vital to examine the wound, including a description of edema, drainage, and the periwound area and wound bed.
- It is vital to look at current wound management.
- Healthcare providers should understand staging of diabetic foot ulcers by Wagner Scale and University of Texas San Antonio Scale.
- The patient history is vital, including past history of ulceration, vascular disease, amputation, Charcot joint, and angioplasty.
- Neuropathic symptoms should also be noted like burning pain, numbness, and the inability to feel the feet.
- Vascular symptoms like claudication, resting pain, and non-healing ulcers
- Additional diabetic complications like retina vision, renal-dialysis, and transplant
- Health management with DM and smoking; hemoglobin A1C, nutrition, tobacco use, and bone density.
- Examine for sensation, specifically if monofilament is >5.07, as this equals a loss of protection.
- Look for ankle reflexes, pinprick, and use a 128 Hz tuning fork, or biothesiometer.
- Check for measures of PAD, including pulses, the posterior tibial, and dorsalis pedis pulses.
- Perform an ABI.
- The functional assessment includes ambulation, transfers, and stairs, as well as quality of motion at the joints of the foot.
- Heel toe raises should be documented.
- Note the current activity level based on step activity monitor.
- Ask if there is a history of vascular disease or claudication pain.
- Ask about fall history, including falls in the past year if patients feel unsteady when standing or walking, or if they worry about falling.
- Balance checks should be performed
- Footwear should be examined
Footwear Assessments
- The current shoes should be examined on both feet. Length, width, depth, shape, material, and construction shall be noted.
- There should be a half inch (1.27 cm) between the longest toe's end and the shoe's front.
- Light-colored materials are preferred to black for cooler temperatures.
- The accommodation of swelling- Velcro, a hook/loop closure, should be adjustable with laces.
- Linings should be soft with no loose edges or prominent seams.
- Insoles should not have wrinkles or curling but provide shock absorption.
- Orthotics should be semi-flexible.
- Materials should be leather, suede, canvas, and breathable synthetics.
- Avoid plastics/vinyl, sandals, thongs, high heels, and open toes.
- Materials should be leather, suede, canvas, and breathable synthetics.
- Shop for shoes at the end of the day when feet tend to be swollen.
- Match the shoe shape to the shape of the foot to avoid pressure on bony prominences.
- Use orthotists to make specialized diabetic footwear for those with foot deformity.
- Change shoes once or twice daily to avoid prolonged pressure over any areas of the foot.
- Making a tracing of the foot may be needed.
National Diabetes Education Program Risk
Categories include
- Low Risk Patients with none of the five high-risk characteristics below. Perform an annual comprehensive foot exam, assess/recommend appropriate footwear, provide the patient with selfcare information for prevention, and perform visual foot inspection.
- High-Risk Patients with one or more of the following: loss of protective sensation, absent pedal pulses, foot deformity, history of foot ulcer, or prior amputation. Perform annual comprehensive foot exam, visual foot inspection at every visit, demonstrate preventative self-care of the feet, and refer to specialists and an educator. Assess and prescribe appropriate footwear and certify Medicare patients for therapeutic shoe benefits while placing a “High-Risk Feet” sticker on the medical record.
- The IWGDF 2019 Risk Stratification System stratifies to determine foot screening frequency. Note the screening frequency is based on expert opinion, since there is no published evidence to support these intervals.
Assessment
- Asses for signs and symptoms consistent with neuropathic ulcers secondary to insensitivity and foot deformities.
- Medical diagnosis: Neuropathic Ulcer
- MSI Diagnosis: Tissue Impairment, Stage 1
- Determine the contributing factors to excessive pressure on the ulcer and how those factors can be modified to reduce the pressure.
- #1 reason for hospitalizations for people with DM.
- What is the most common way to assess lower extremity in clinic?
- Is an ABI of 0.7 okay and what if the ABI is 1.4 and what could be the cause?
- What are the normal ranges of ABI?
- Which monofilament is protective sensation?
- What is the common mechanism of injury to the foot?
- What is a good clinical test of systematic limited joint mobility?
- ADA goals for glucose control.
- Factors contributing to skin breakdown on the diabetic foot.
- Examination components for clients with diabetes and suspected neuropathy.
Interventions
- Patient education
- Footwear
- Wound management
- Surgical
Patient Education:
- Daily foot inspection by family members.
- early detection and treatment.
- Wearing shoes that fit to avoid going barefoot.
- Wash feet daily in warm water and dry.
- Avoid direct heat to desensitize the foot.
- Cut toenails straight across after bathing with nails softened.
- Wear white cotton or synthetic, moisture-wicking socks(soft, padded, not prominent toe seams, tight elastic or holes).
- Apply moisturizer to feet.
- Avoid going barefoot
- Look at current shoes on both feet for length, width, depth, shape, material and construction.
- Allow ½” (1.27 cm) between the end of the longest toe and the front of the shoe.
- Light-colored materials are preferred to black (lower temperatures).
- Swelling can be accommodated with Velcro, a hook or loop closure, or adjustable laces.
- Linings should be soft, without seams.
- Insoles should be free of wrinkles or curling and provide shock absorption.
- Orthotics should be semi-flexible.
- Select materials that are leather, suede, canvas, or breathable synthetics and avoid plastics/vinyl, sandals, thongs, high heels, and open toes
- There is a key to protecting the foot with pressure being the force divided by the area.
- Decrease force or increase the area.
Footwear Guidelines
- It must be the best fitting shoe possible
- Work closely with an orthotist who has shoe-maker experience.
- Accommodate deformity and reduce stress while distributing pressures with a total contact insert.
- The rigid rocker bottom sole should have ADA Consensus, 2008; and IWGDF Guidelines 2019.
- AFO is needed for foot-drop
Main Points
- The contributing factors to skin breakdown on the diabetic foot include peripheral neuropathy, peripheral vascular disease, and joint deformity limited joint mobility due to physical stresses.
- Primary treatment and preventive interventions for neuropathic prevention of skin include protecting the insensitive foot from excessive stress.
- Main important education needed with patients
- Type of intervention needed for each risk
Ulcer Management
- Wound care
- Off-loading
- Remodeling
- Protective footwear
Tissue Impairment Management
- In stage 1, total contact casting is the most effective off-loading method.
- 90% of wounds heal in 42 days.
- There is an 82% pressure reduction at the site of the ulcer.
- Removable pressure relief walkers have comparable pressure reduction, although lower healing rates of 58% vs. 90% have been observed.
- Patients tend to only wear them 25% of the time.
Custom Footwear
- Custom rocker bottom shoes with custom insoles can reduce pressure ~30% and are often fitted with apex proximal to the met heads
Other Findings
- High ulcer recurrence rates such as 34%, 61% and 70% in years 1,3,5 that can be mitigated with Tendo Achilles Lengthening and weakness and with Pressure having been decreased after the procedure with Lin 96, Mueller et al, 2003.
- Walking Goal: 10,000 steps /day (Surgeon General)
- People with Type 2 DM should perform 30 minutes per day of moderate exercise (50% of max heart rate) at least 5x per week or 150 minutes per week of moderate intensity.
- People with DM and PN have historically limited prolonged weight-bearing exercise, with ADA position statements for 2006, 2009, and 2016.
- Surgical causes of amputation are diabetes (at least 90%), peripheral vascular disease, trauma, cancer, and congenital problems.
- Surgical procedures can include toe amputation, transmetatarsal amputation (TMA), below the knee amputation (BKA), and above the knee amputation (AKA).
- Of LEAs, 41% are in DM; 26% in other; Report from Reiber, 2001;
- In TMA, 11% of all occur in DM cases while 6% will result in others.
- In immediate post-op TMA treatment, there should be a heel strike offloader shoe rather than the patient being non-weight bearing (NWB).
- StudIes show there is less peak plantar pressure when incisions are healed in DM patients.
- Key practice includes total contact insert.
- And includes use of rigid rocker-bottom sole is very useful and is included in the (Snacore).
Key Points
- Screen diabetic foot risk
- Protect the sensitive Always
- Reduce excessive Skin (Tissue wound, and limit excessive stress
Review
- Is footwear appropriate for patients with surgery or TMA
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.