Podcast
Questions and Answers
What is the rationale behind prescribing specific footwear for individuals with an insensitive foot, considering their patient characteristics?
What is the rationale behind prescribing specific footwear for individuals with an insensitive foot, considering their patient characteristics?
- To avoid the examination of the foot
- To increase the risk of injury.
- To promote physical therapy management and reduce risk of injury. (correct)
- To disregard examination components.
According to the CDC 2020 data, what percentage of the US population was estimated to have diabetes in 2020?
According to the CDC 2020 data, what percentage of the US population was estimated to have diabetes in 2020?
- Approximately 9.4%
- Approximately 10.5% (correct)
- Approximately 12.1%
- Approximately 8.2%
How does the lack of awareness of having diabetes mellitus (DM) impact foot health, considering preventative measures?
How does the lack of awareness of having diabetes mellitus (DM) impact foot health, considering preventative measures?
- It decreases the likelihood of developing foot ulcers due to increased vigilance.
- It has no significant impact, as foot health is primarily determined by genetic factors.
- It encourages proactive foot care, leading to early detection of foot diseases.
- It may lead to delayed diagnosis and treatment, increasing the risk of foot ulcers and complications. (correct)
Why are individuals with diabetes mellitus at a significantly higher risk for lower extremity amputations compared to the general population?
Why are individuals with diabetes mellitus at a significantly higher risk for lower extremity amputations compared to the general population?
The Centers for Disease Control and Prevention (CDC) have identified that a substantial percentage of non-traumatic lower extremity amputations could be avoided with comprehensive diabetic foot care. What is the estimated avoidable range?
The Centers for Disease Control and Prevention (CDC) have identified that a substantial percentage of non-traumatic lower extremity amputations could be avoided with comprehensive diabetic foot care. What is the estimated avoidable range?
Beyond the presence of Peripheral Arterial Disease (PAD) and Peripheral Neuropathy, what additional factor significantly contributes to foot breakdown in individuals with diabetes?
Beyond the presence of Peripheral Arterial Disease (PAD) and Peripheral Neuropathy, what additional factor significantly contributes to foot breakdown in individuals with diabetes?
How does peripheral arterial disease (PAD) contribute to the development of ischemic pain in the lower extremities?
How does peripheral arterial disease (PAD) contribute to the development of ischemic pain in the lower extremities?
When assessing the severity of Peripheral Arterial Disease (PAD) using the Ankle Brachial Index (ABI), which range is typically considered normal, assuming no calcification of tibial arteries?
When assessing the severity of Peripheral Arterial Disease (PAD) using the Ankle Brachial Index (ABI), which range is typically considered normal, assuming no calcification of tibial arteries?
Why might the Ankle Brachial Index (ABI) be unreliable in diabetic patients when assessing peripheral artery disease (PAD)?
Why might the Ankle Brachial Index (ABI) be unreliable in diabetic patients when assessing peripheral artery disease (PAD)?
How does peripheral neuropathy impact the intrinsic muscles of the feet, and what are the potential consequences of this impact?
How does peripheral neuropathy impact the intrinsic muscles of the feet, and what are the potential consequences of this impact?
What does a Semmes-Weinstein monofilament value of 5.07 indicate in the context of peripheral neuropathy assessment?
What does a Semmes-Weinstein monofilament value of 5.07 indicate in the context of peripheral neuropathy assessment?
How does autonomic neuropathy contribute to skin changes in the feet, and what specific issues may arise as a result?
How does autonomic neuropathy contribute to skin changes in the feet, and what specific issues may arise as a result?
What type of mechanical stress to the foot could lead to skin breakdown in a patient with diabetic neuropathy:
What type of mechanical stress to the foot could lead to skin breakdown in a patient with diabetic neuropathy:
How do activities with moderate repetitive pressures contribute to the risk of foot injury in individuals with diabetic neuropathy?
How do activities with moderate repetitive pressures contribute to the risk of foot injury in individuals with diabetic neuropathy?
What is the clinical relevance of recognizing specific foot deformities, such as hammer toes, in the context of diabetic foot care?
What is the clinical relevance of recognizing specific foot deformities, such as hammer toes, in the context of diabetic foot care?
How does limited joint mobility increase the risk of foot complications, especially in conjunction with sensory neuropathy?
How does limited joint mobility increase the risk of foot complications, especially in conjunction with sensory neuropathy?
What are some key characteristics that differentiate neuropathic ulcers from venous or arterial ulcers?
What are some key characteristics that differentiate neuropathic ulcers from venous or arterial ulcers?
What is the significance of recognizing Charcot arthropathy in its early stages and why is early intervention critical?
What is the significance of recognizing Charcot arthropathy in its early stages and why is early intervention critical?
What specific footwear characteristics are recommended for individuals with diabetes to minimize the risk of foot complications and what materials should be avoided?
What specific footwear characteristics are recommended for individuals with diabetes to minimize the risk of foot complications and what materials should be avoided?
What are the critical components of patient education for individuals with diabetes regarding daily foot care practices?
What are the critical components of patient education for individuals with diabetes regarding daily foot care practices?
What is the most crucial element in managing a diabetic foot ulcer to prevent further complications and promote healing?
What is the most crucial element in managing a diabetic foot ulcer to prevent further complications and promote healing?
What is the primary goal of total contact casting (TCC) in the management of diabetic foot ulcers?
What is the primary goal of total contact casting (TCC) in the management of diabetic foot ulcers?
What are the limitations of using removable cast walkers instead of total contact casts for offloading diabetic foot ulcers?
What are the limitations of using removable cast walkers instead of total contact casts for offloading diabetic foot ulcers?
Following the healing of a diabetic foot ulcer, what is the primary concern regarding ulcer recurrence and what strategies can be employed to address this concern?
Following the healing of a diabetic foot ulcer, what is the primary concern regarding ulcer recurrence and what strategies can be employed to address this concern?
Historically, individuals with diabetes mellitus and peripheral neuropathy were often advised to limit prolonged weight-bearing exercises. How has this recommendation evolved, and what is the current stance on physical activity for these individuals?
Historically, individuals with diabetes mellitus and peripheral neuropathy were often advised to limit prolonged weight-bearing exercises. How has this recommendation evolved, and what is the current stance on physical activity for these individuals?
What is the most common underlying cause of lower extremity amputations in individuals with diabetes mellitus?
What is the most common underlying cause of lower extremity amputations in individuals with diabetes mellitus?
After a transmetatarsal amputation (TMA), what is the most important consideration in terms of post-operative care and footwear to ensure proper healing and prevent further complications?
After a transmetatarsal amputation (TMA), what is the most important consideration in terms of post-operative care and footwear to ensure proper healing and prevent further complications?
What is a critical recommendation for post-operative care, especially concerning footwear, immediately after a transmetatarsal amputation (TMA)?
What is a critical recommendation for post-operative care, especially concerning footwear, immediately after a transmetatarsal amputation (TMA)?
Flashcards
Objective
Objective
Learners will be able to describe the possible mechanisms of injury to the insensitive foot.
Objective
Objective
Individuals will be able to choose the physical therapy management of patient with an insensitive foot (including prescription of proper footwear) and examination components.
Diabetes Incidence in US (CDC)
Diabetes Incidence in US (CDC)
In 2015, 30.3 million, 9.4% of the population; In 2020, 34.2 million, 10.5% of population.
Diabetes and Amputation
Diabetes and Amputation
Signup and view all the flashcards
Preventable Amputations
Preventable Amputations
Signup and view all the flashcards
Peripheral Arterial Disease (PAD)
Peripheral Arterial Disease (PAD)
Signup and view all the flashcards
PAD and Muscle Activity
PAD and Muscle Activity
Signup and view all the flashcards
Ischemia in PAD
Ischemia in PAD
Signup and view all the flashcards
PAD Testing - Pulses
PAD Testing - Pulses
Signup and view all the flashcards
Ankle Brachial Index (ABI)
Ankle Brachial Index (ABI)
Signup and view all the flashcards
Angiogram
Angiogram
Signup and view all the flashcards
Peripheral Neuropathy
Peripheral Neuropathy
Signup and view all the flashcards
Neuropathy Symptoms
Neuropathy Symptoms
Signup and view all the flashcards
Mechanism of Injury- Pressures
Mechanism of Injury- Pressures
Signup and view all the flashcards
Mechanism of Injury
Mechanism of Injury
Signup and view all the flashcards
Foot Deformities
Foot Deformities
Signup and view all the flashcards
Development of Hammer Toe
Development of Hammer Toe
Signup and view all the flashcards
Limited Joint Mobility
Limited Joint Mobility
Signup and view all the flashcards
Limited Joint Mobility - First MTP
Limited Joint Mobility - First MTP
Signup and view all the flashcards
Acute Charcot Arthropathy
Acute Charcot Arthropathy
Signup and view all the flashcards
Partial Foot Amputation
Partial Foot Amputation
Signup and view all the flashcards
Extrinsic Factors - Footwear
Extrinsic Factors - Footwear
Signup and view all the flashcards
Patient Screening
Patient Screening
Signup and view all the flashcards
Venous ulcer
Venous ulcer
Signup and view all the flashcards
Arterial ulcer
Arterial ulcer
Signup and view all the flashcards
Neuropathic
Neuropathic
Signup and view all the flashcards
Ischemic Foot - Sign & Symptoms
Ischemic Foot - Sign & Symptoms
Signup and view all the flashcards
Wagner Scale - Class 3
Wagner Scale - Class 3
Signup and view all the flashcards
Patient Examination- Foot wear
Patient Examination- Foot wear
Signup and view all the flashcards
Patient Education
Patient Education
Signup and view all the flashcards
Study Notes
Objectives for Learners
- Learners can describe the possible mechanisms of injury to the insensitive foot.
- Individuals can choose the physical therapy management of a patient with an insensitive foot, including footwear prescriptions and examination components, based on patient characteristics.
Diabetes and the Diabetic Foot
- In 2015, 30.3 million people in the US, which represents 9.4% of the population, had diabetes.
- By 2020, the number increased to 34.2 million, or 10.5% of the population
- Twenty-three percent of adults with diabetes are unaware they have it or did not report it.
- Foot disease and ulcers are the most common issue leading to hospitalization.
- 34% of patients with diabetes mellitus develop a foot ulcer in their lifetime.
- The annual incidence of foot ulcers in the non-diabetic population is about 2%.
- The amputation rate for individuals with diabetes is 10-13 times higher than that of controls.
- 50% of lower extremity amputations could be prevented
- 45% to 85% of non-traumatic lower extremity amputations in the US, attributable to diabetes, could have been avoided with comprehensive diabetic foot care programs, according to the CDC.
Contributing Factors to Foot Breakdown
- Peripheral arterial disease (PAD), peripheral neuropathy, & joint deformity (limited joint mobility) contributes to foot breakdown.
- Physical stresses may also cause foot breakdown, so the physical stresses need managed.
- Screening and primary treatment interventions, as well as prevention strategies for neuropathic skin breakdown, are required.
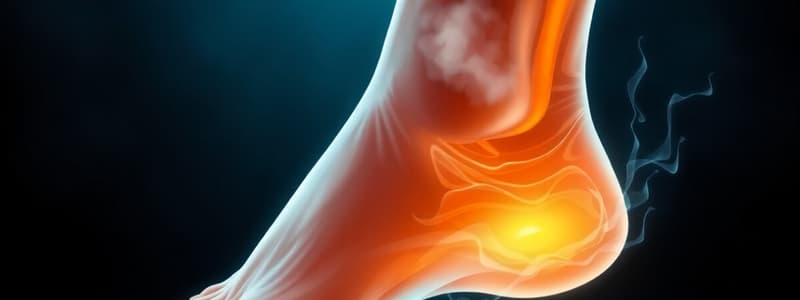
Peripheral Arterial Disease (PAD)
- PAD involves narrowed arteries caused by fatty plaque deposits, which leads to decreased circulation.
- Decreased blood supply is especially required by muscles during activity, leading to reduced oxygen supply.
- Ischemia occurs, which results in excessive lactic acid accumulation and pain.
- If PAD is more severe, it presents earlier onset in those with diabetes mellitus.
- PAD affects distal vessels and has over 4x the incidence in those with diabetes mellitus.
- For those with a 20-year duration of diabetes mellitus, 45% have PAD.
PAD Testing
- A common PAD testing method is but has poor reliability. -Assess posterior tibial and dorsalis pedis pulses, noting if they are absent or present -Relative risk = 1.90 (1.4-2.4)
- Better reliability can be achieved using an Ankle Brachial Index (ABI) or angiogram.
- The Ankle Brachial Index (ABI) is the ratio of systolic blood pressure at the ankle to the brachial systolic pressure.
- Ankle systolic blood pressure is taken using the posterior tibial artery or dorsalis pedis; blood pressure is obtained by using Doppler.
- The ABI is the gold standard for diagnosing the presence or severity of PAD with a sensitivity of 95% and a specificity of 99%.
- 0.9-1.3 is considered normal.
- Values less than .8 are problematic
- Values less than .4 may mean wound healing issues
- In those with diabetes mellitus with calcified tibial arteries, the ABI is not as effective where it can see falsely high values >1.3, a serious problem.
Angiogram
- This locates and determines the amount of occlusion from plaques in the artery- dye is injected in the artery and an x-ray determines the extent and location of the occlusion.
Other Effects of PAD
- Painful ischemic pain can occur.
- Visual changes include dry skin, thickened nails, wounds distally, poor wound healing, and rubor of dependency.
Neuropathy
- With peripheral neuropathy there is motor, sensory, and autonomic components.
- Muscular wasting of intrinsic muscles of the feet, which sensory-wise, leads to decreased touch, vibration sense, proprioception, temperature, and pain, can occur.
- Pain may be worse at night or at rest, with burning and tingling progressing to no pain.
- Peripheral neuropathy is distal and symmetric polyneuropathy.
- Stocking gloves presentation occurs, involving toes and progressing to feet and lower extremities.
- Often, no pain or subjective complaints are experienced, and after 25 years with diabetes mellitus, 50% have symptoms.
- Semmes Weinstein Monofilaments can measure peripheral neuropathy.
- 5.07 indicates loss of protective sensation (~10 grams)
- 4.17 is intact
-
6.10 is essentially absent
- A predictive of ulcer/amputation occurs at 1.80-2.03 Risk Ratio.
- Patients unable to sense 5.07 SW monofilament were 10x more likely to develop foot ulcers and 17x more likely for amputation.
- Semmes Weinstein Monofilaments should be applied for 1 second on and 1 second off, applying enough pressure so the monofilament bends.
- Deficits in sweating can occur and also dry, cracking feet
- Deficits in vascular/thermoregulation can occur and fungal infections
- Lotion is a treatment that can be applied.
Mechanism of Injury
- Excessive pressures on insensitive skin can be caused by low pressures for long durations, a high pressure for short durations, and moderate pressures repeated many times.
- Paul Brand originated the physical stress theory.
- High pressure (1,300 PSI) with low duration and low pressure (5-8 PSI) with long duration (6-8 hours) can result in injury.
Role of Neuropathy and Minor Trauma
- Neuropathy + minor trauma = baseline pathology + environmental event + ulceration = faulty healing + intercurrent pathophysiology = gangrene + intercurrent pathophysiology = completed causal chain to amputation.
Foot Deformities
- Hammer toes and prominent metatarsal heads lead to high pressures and ulcers at the dorsal interphalangeal joint and plantar metatarsophalangeal joint.
- Hallux limitus of the first metatarsophalangeal joint.
- Ulcer of 1st toe
- In development of hammer toe deformity
- Ankle dorsiflexion decreases
- Intrinsic muscle decreases
- Metatarsophalangeal joint flexion decreases
- Metatarsophalangeal joint extension movement pattern increases
- Claw toes also occur
Limited Joint Mobility
- Limited joint mobility is a systematic problem
- Multiple joint involvement affects hands, wrists, shoulders, ankles, subtalar joint, & metatarsophalangeal joints.
- a positive prayer sign can also be seen.
- Advanced Glycated End Products accumulate
- Subtalar Joint
- Forefoot Ulcer
- Ankle Joint
- Forefoot Ulcer
Acute Charcot Arthropathy
- Neuropathic bone destruction occurs.
- Signs: Swelling, redness, heat and sometimes pain
- Immobilization, risk for skin breakdown, risk of deformity become highly important
Developmental Stages of Charcot
- Stage 0 involves an inflammatory period with no radiographic changes, but onset of erythema, warmth, swelling, and pain occur.
- Stage 1 has fragmentation/destruction period. with fragmentation of subchondral bone & cartilage, distension of joint capsule & ligamentous laxity, joint subluxation/dislocation with deformity.
- Stage 2 goes through coalescence with diminishing inflammation; absorption of cartilaginous and subchondral debris, formation of bone callus, consolidation of fractures also occur.
- Stage 3 goes through reconstruction with bony ankylosis, hypertrophic bone formation, fixed deformity or persistent instability taking place.
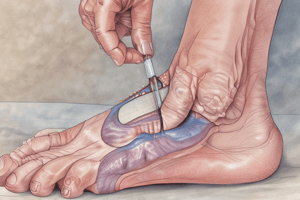
Partial Foot Amputation
- Partial foot amputation can cause higher pressure on the residuum.
- More likely to develop an ulcer on residuum
- 30% develop risk for more amputation.
Extrinsic Factors: Footwear
- Poor-fitting shoes and walking barefoot with insensitive feet most commonly cause ulceration.
Patient Screening
- Check for diabetes or prediabetes history, check pulses and skin, test for neuropathy/inability to sense 5.07 monofilament
Other Factors
- HBA1c: normal range <6.5% with a current American Diabetes Association goal.
- Consulting a dietician/nutrition professional is an important factor.
Patient Examination
- Skin changes – check Autonomic Nervous System, Assess Skin Changes.
- Foot deformity: hammer toe, claw toe, prominent metatarsal heads, partial foot amputation, Charcot, bunions.
- Ulcer- blister, gangrene.
- Sensation - use monofilament - >5.07 = loss of protective sensation
- Other sensation exams Ankle reflexes, pinprick, Tuning fork, biothesiometer.
- The ankle brachial index should be checked -pulses- posterior tibial & dorsalis pedis pulses, Check for ABI.
- Check fall history; has there been falls in the past year? do you feel unsteady standing or walking?
- Asses balance, footwear (take a look), and Functional assessment.
- With Functional assessment - Ambulation, transfers, stairs needs assessed; Quality motion at the joints foot (sit to stand).
- Check heel toe raises, Current activity level (step activity monitor), history vascular dz- claudication pain & also Check fall history.
- Assess current shoes Length, width, depth, shape, material & construction.
- Allow ½” (1.27 cm) between end of the longest toe and front of shoe.
- Look for Light color materials vs black (lower temps), Accommodating Swelling- Velcro, hook/loop closure, Linings- soft, no loose edges & Insoles- no wrinkles when assessing
- In addition assess Orthotics (semi-flexible) Also Assess:
- Materials- leather, suede, canvas or breathable synthetics (may trace their feet)
- Avoid: plastics/vinyl, sandals, high heels, open toes & thongs
- Match shoe shape to shape foot (orthotist)
- Change shoes once or twice daily.
Neuropathic Wounds
- With Decreased sebaceous gland release; sudomotor dysfunction, there is Dry skin, skin risk and skin risk is Increased callus formation & likelihood fissures; increased areas pressure & likelihood skin breakdown.
- With Loss protective sensation there is Inability to perceive harmful levels pressure/force & skin risk Increases likelihood skin and breakdown.
- With Muscle atrophy, deformity (e.g., claw toe, hammer toe) there is Increased & Motor system involved gradient; increased likelihood of skin breakdown.
- Past history of varicose veins orsurgery is venous ulcer.
- History of smoking, intermittent claudication is an arterial ulcer.
- His Numbness; Loss sensation in the foot: Common diabetes mellitus in neuropathic.
Other characteristics of wound/feet (Venous vs arterial vs Neuropathic)
- Past history of varicose veins +/- DVT, trauma, surgery to leg or multiple pregnancies (Venous), History smoking or PAINFUL leg with elevating (Arterial),His of Numbness; Loss sensation- DM. (Neuropathic).
- Between malleolus and the lower calf with Medial Mallolus (Venous), Distally & Boney promises (arterial)
- Normal ABI is (3 seconds) in Venous, Prolonged is (4-5 senconds) Artery
- Pale feet, Shiny &/or atrophy (of skin or feet), cool-weak or absent dorsalis pedis pulse = artery involved
Signs & Symptoms of feet
- Neuropathic feet: Burning, Tingling, Pins And needles, numbness, Sharp/Eletric shock, stabbing & deep achy is experienced (mostly feet & toes but also the legs) & most of the pain ↑’s with rest (& @ night, with Cramps).
- Ischemic: LE’s exhibit aching: with hanging them off the bed at night or walking. Other signs/Symptoms/Deformities:
- Palpate for the diminished, cool & usually shiny and hairless skin on ischemic feet (venous have warm, dry and palpable pulses)
- Absent sensation on “Neoropathic” feet with: Intrinsic muscle feet leading to claw toes, hammer toes &/or Prominent heads which lead to “thick/soft” calluses &/or ulcerations. What about location?
- Nero- feet ulcer is the: “Tips” of the toes & Plantar Metatarsal heads
- Ischemic foot Is mostly on the feet margin and at the tips of toes and heels
Patient examination
- Examine wounds describingEdema, Drainage, Periwound, Wound bed.
- Use Wagner scale for Staging (0) Pre- or Post lesions or cellulitis: (1) Superficial ulcer; (2)Deep ulcer; (3) Abscess or bone involvement; (4)Gangrene digits/Forefoot
Patient history
- History: check the ulcer, vascular dx, amputation, Charcot joints as you examine past dx and records
- Burning and/or numbness is symptoms of Neuropathic feet and examine them
- Claudication &/or Resting Pain is symptoms of Ischemic ft examine for non-hearing ulcer and if they hurt with palpations Diabetes, poor blood sugars can cause Kidney/eye issues to retina.
- Health Management: Manage all health problems, Dm , smoking which includes tobacco, diet- Nutrition which all involve Bone Density.
National Diabetes Education Program Risk Categories and Management Guidelines-
- Those most at risk for High Risks one being One or more from: Loss protective sensation Absent pedal pulses or Foot deformity as well a
- History of past ulcer or past amputees should especially be checked
- Those in renal end stage are at high risk.
Assessment of feet with skin breakdown
Wbat would factor In contributing pressures on ulcer? -What modifies to reduce ulcer problems.
Review all interventions in feet with complications
- What education to provide and risk for each those at risk and How toe check ft.
Pt teaching and more interventions from that teaching:
- Foot wear is important and mg can help a lot.
Ulcer mgmt and teaching to Pt’s
- Daily ft inspection from pt’s
- And footcare instructions that show safe and dry ft after cleaning.
- Avoid bare ft, avoid cutting toe nails after bathing How well should feet be cared for at home.
Shoe Fitting at home by pts and education
- Shoe width, and construction need be correct; allow 1/2” from longest tow
- The best color and shoe to were , best ways accommodate swelling and type of closures that are pt oriented
- Have smooth lining and support absorption from semi rigid support.
Here list additional resources;
- CDC Diabetes - Take Charge Your Feet
- LEAP in feet and
- diabetes/foot issues and teaching
Key To Preventing Pts From Ft Problems -
- The main problem Is the Pressure -So the less resistance on feet and more surface available the easier is to have good outcomes.
Ft exam:
- Is the pt protected ( Good foot - Yes that Is Mandatory to check?
- Do they have any extra needs ( good shoes / inserts. & can they be comfortable w/ those inserts.
- Medicare helps by covering costs with above guidelines. - Good shoes, (optional ) w/ support inserts.
- Also remember (as stated previously ) the risk high if there an ulcer, If there multiple problems with healing or not (special boots need with casts).
The best way to care for is:
- The right gear at all levels when need
The shoe types are:
- The more protection & less protection is needed to help (the more Hx.
-If an ulcer is present than they are consider “High Risk” and will need custom shoe with insert and bottom rocker to prevent issues
Goals to help Pt’s when using any of the above interventions
- Use best gear at all stages with Pts
- But it always more serious If they had ulceration & and will need help.
A better understanding how to help; look to goals when using proper gear
-
Reduce risk factors and teach the ways from pt to pt.
-
How to use it can help
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.