Podcast
Questions and Answers
Which test requires the patient to respond 'yes' or 'no' regarding the application of the monofilament?
Which test requires the patient to respond 'yes' or 'no' regarding the application of the monofilament?
- Pinprick sensation
- Ankle Reflexes
- 10g Monofilament Exam (correct)
- Vibration perception threshold (VPT)
What should be avoided when testing for pressure perception during the 10g Monofilament Exam?
What should be avoided when testing for pressure perception during the 10g Monofilament Exam?
- Applying pressure too forcefully
- Testing on areas of callus (correct)
- Performing the test without patient instruction
- Using a softer material
What indicates an abnormal response when testing vibratory sensation using a 128-Hz tuning fork?
What indicates an abnormal response when testing vibratory sensation using a 128-Hz tuning fork?
- The patient feels the vibration while the examiner does not
- The examiner feels the vibration while the patient does not (correct)
- The vibration is perceived only on one toe
- Both the patient and examiner fail to perceive the vibration
What is the correct procedure for assessing the vibration perception threshold (VPT) using a biothesiometer?
What is the correct procedure for assessing the vibration perception threshold (VPT) using a biothesiometer?
What result is regarded as abnormal when measuring the vibration perception threshold (VPT)?
What result is regarded as abnormal when measuring the vibration perception threshold (VPT)?
What is the primary pathway leading to diabetic foot ulceration?
What is the primary pathway leading to diabetic foot ulceration?
What percentage of diabetic ulcers are likely to become infected?
What percentage of diabetic ulcers are likely to become infected?
Which of the following factors does NOT contribute to the risk of developing diabetic foot ulcerations?
Which of the following factors does NOT contribute to the risk of developing diabetic foot ulcerations?
What is the impact of regular foot exams on the rate of amputations related to diabetic foot complications?
What is the impact of regular foot exams on the rate of amputations related to diabetic foot complications?
In a diabetic foot exam, what should be assessed regarding the patient's footwear?
In a diabetic foot exam, what should be assessed regarding the patient's footwear?
Which of the following is a sign that may indicate Peripheral Artery Disease (PAD) during an exam?
Which of the following is a sign that may indicate Peripheral Artery Disease (PAD) during an exam?
Which statement correctly describes Loss of Protective Sensation (LOPS)?
Which statement correctly describes Loss of Protective Sensation (LOPS)?
What percentage of diabetes-related amputations are believed to be preceded by an ulceration?
What percentage of diabetes-related amputations are believed to be preceded by an ulceration?
What is the purpose of demonstrating the sensation of the 10g monofilament on a proximal site before testing on the foot?
What is the purpose of demonstrating the sensation of the 10g monofilament on a proximal site before testing on the foot?
Why should areas of callus be avoided during the 10g monofilament test?
Why should areas of callus be avoided during the 10g monofilament test?
Which condition would be indicated by an abnormal response during the pinprick sensation exam?
Which condition would be indicated by an abnormal response during the pinprick sensation exam?
What criteria is used to classify a vibration perception threshold (VPT) result as abnormal?
What criteria is used to classify a vibration perception threshold (VPT) result as abnormal?
Which test utilizes a tuning fork to assess a patient's vibratory sensation?
Which test utilizes a tuning fork to assess a patient's vibratory sensation?
What is the most common factor that precipitates diabetic foot ulceration?
What is the most common factor that precipitates diabetic foot ulceration?
Which of the following statistics reflects the global annual incidence of diabetic foot ulcerations?
Which of the following statistics reflects the global annual incidence of diabetic foot ulcerations?
Which pathway sequence is typically involved in the development of a diabetic foot ulcer?
Which pathway sequence is typically involved in the development of a diabetic foot ulcer?
What percentage reduction in amputation rates can regular foot exams achieve?
What percentage reduction in amputation rates can regular foot exams achieve?
Which of the following factors is NOT classified as a risk factor for diabetic foot ulceration?
Which of the following factors is NOT classified as a risk factor for diabetic foot ulceration?
During a diabetic foot exam, which specific skin condition should be checked for between the toes?
During a diabetic foot exam, which specific skin condition should be checked for between the toes?
What is a common physical sign of Peripheral Artery Disease (PAD) one should inspect for during the foot exam?
What is a common physical sign of Peripheral Artery Disease (PAD) one should inspect for during the foot exam?
What is the impact of uncontrolled blood glucose levels on foot health in diabetic patients?
What is the impact of uncontrolled blood glucose levels on foot health in diabetic patients?
What is the recommended action for patients during the 10g Monofilament Exam?
What is the recommended action for patients during the 10g Monofilament Exam?
When assessing vibratory sensation with a 128-Hz tuning fork, what indicates a loss of sensation?
When assessing vibratory sensation with a 128-Hz tuning fork, what indicates a loss of sensation?
Which of the following techniques is utilized to assess the vibration perception threshold (VPT)?
Which of the following techniques is utilized to assess the vibration perception threshold (VPT)?
What is considered an abnormal threshold result when measuring the vibration perception threshold (VPT)?
What is considered an abnormal threshold result when measuring the vibration perception threshold (VPT)?
What should be the approach if a patient cannot perceive pinprick sensation during the exam?
What should be the approach if a patient cannot perceive pinprick sensation during the exam?
What is a key precipitating factor in the pathogenesis of diabetic foot ulceration?
What is a key precipitating factor in the pathogenesis of diabetic foot ulceration?
Which of the following factors does NOT significantly increase the risk of developing diabetic foot ulcerations?
Which of the following factors does NOT significantly increase the risk of developing diabetic foot ulcerations?
In assessing lower extremity conditions, what should be inspected regarding a patient's footwear?
In assessing lower extremity conditions, what should be inspected regarding a patient's footwear?
What percentage of diabetic foot ulcers are likely to lead to infection?
What percentage of diabetic foot ulcers are likely to lead to infection?
Which sign could indicate peripheral artery disease during an assessment?
Which sign could indicate peripheral artery disease during an assessment?
What is the impact of regular foot examinations on amputation rates in diabetic patients?
What is the impact of regular foot examinations on amputation rates in diabetic patients?
Which of the following best describes the term 'Loss of Protective Sensation' (LOPS)?
Which of the following best describes the term 'Loss of Protective Sensation' (LOPS)?
Which risk factor is associated with previous diabetic foot complications leading to ulceration?
Which risk factor is associated with previous diabetic foot complications leading to ulceration?
What is the primary risk factor for the pathogenesis of diabetic foot ulceration?
What is the primary risk factor for the pathogenesis of diabetic foot ulceration?
Which of the following conditions has the highest risk for developing diabetic foot ulcerations?
Which of the following conditions has the highest risk for developing diabetic foot ulcerations?
What percentage of diabetic foot ulcers are known to lead to serious infections requiring amputation?
What percentage of diabetic foot ulcers are known to lead to serious infections requiring amputation?
In a comprehensive foot exam, which aspect is least likely to be part of the visual inspection?
In a comprehensive foot exam, which aspect is least likely to be part of the visual inspection?
How significant is the impact of regular foot examinations on diabetic amputation rates?
How significant is the impact of regular foot examinations on diabetic amputation rates?
Which of the following is a common sign of Peripheral Artery Disease (PAD) that should be assessed during foot exams?
Which of the following is a common sign of Peripheral Artery Disease (PAD) that should be assessed during foot exams?
At what annual global incidence rate do diabetic foot ulcerations occur?
At what annual global incidence rate do diabetic foot ulcerations occur?
Which condition is NOT typically assessed as part of risk for diabetic foot ulceration?
Which condition is NOT typically assessed as part of risk for diabetic foot ulceration?
What is the primary purpose of using the 10g monofilament test in diabetic foot examination?
What is the primary purpose of using the 10g monofilament test in diabetic foot examination?
Which procedure is recommended for ensuring accurate results during the pinprick sensation test?
Which procedure is recommended for ensuring accurate results during the pinprick sensation test?
In the context of vibration perception threshold (VPT) testing, what does a reading greater than 25 V indicate?
In the context of vibration perception threshold (VPT) testing, what does a reading greater than 25 V indicate?
Which site should the 10g monofilament test NOT be applied to during examination?
Which site should the 10g monofilament test NOT be applied to during examination?
When performing the vibration test with a 128-Hz tuning fork, what does an abnormal response suggest?
When performing the vibration test with a 128-Hz tuning fork, what does an abnormal response suggest?
Flashcards are hidden until you start studying
Study Notes
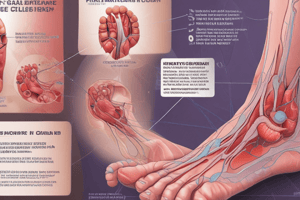
Diabetic Foot Statistics
- Diabetic foot ulcerations are a common complication of diabetes
- The global annual incidence of ulcerations is 6.3%
- More than 50% of diabetic ulcers become infected
- About 20% of diabetic ulcers with moderate to severe infection result in amputation
- Nearly 85% of diabetes-related amputations are preceded by ulceration
- Regular foot exams can reduce amputation rates by 45% to 85%
Pathogenesis of Ulceration
- Neuropathy is a key precipitating factor in ulceration
- Pedal deformity can lead to trauma, especially from repetitive microtrauma
- Other risk factors for ulceration:
- Previous ulceration/amputation
- PAD/PVD
- Foot Deformity
- Peripheral Neuropathy
- Poor glycemic control
- Visual impairment
- Nephropathy
- Smoking
Diabetic Foot Exam
- Should be performed at every visit for patients with sensory loss, previous foot ulcers, or amputations
Visual Inspection
- Dermatologic:
- Skin status (color, thickness, dryness, cracking)
- Sweating
- Infection (check between toes for fungal infection)
- Ulceration
- Calluses/Blistering (check for hemorrhage into callus)
- Musculoskeletal:
- Deformity (e.g., claw toes, prominent metatarsal heads, Charcot joint)
- Muscle wasting (guttering between metatarsals)
Footwear Assessment During Visual Inspection
- Check for signs of trauma:
- Shoes should be wide and deep enough to accommodate feet/deformities
- Shoes showing excessive wear or loss of protective padding (e.g., worn-out soles)
- Shoes that are too short (check for a finger length space between the longest toe and the end of the insole)
- Socks should be present, not worn out, and not constricting
Screening for PAD
- Check dorsalis pedis and posterior tibialis pulses
- Inspect for physical signs of PAD (hair loss, pallor/cyanosis, thinning of skin, ulceration)
- Check or refer for ABI if necessary, especially in patients with signs and symptoms of vascular disease or absent pulses
Neurologic/Protective Sensation
- Loss of protective sensation (LOPS) is a high risk factor for ulceration
- Perform the 10g monofilament test plus at least one of the following four:
- Vibration using a 128-Hz tuning fork
- Pinprick sensation
- Ankle Reflexes
- Vibration perception threshold (VPT)
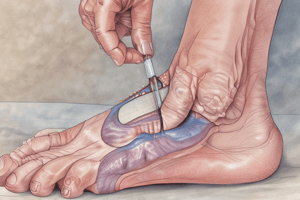
10g Monofilament Exam Instructions
- Patients should close their eyes while being tested
- Demonstrate the sensation of pressure using the monofilament on a proximal site (upper arm, thigh)
- Test the sites of the foot by asking the patient to respond "yes" or "no" when asked whether the monofilament is being applied
- Avoid areas of callus when testing for pressure perception
Vibration using 128-Hz Tuning Fork
- Test vibratory sensation over the tip of the great toe bilaterally
- Abnormal response: Patient loses vibratory sensation, but the examiner can still perceive it while holding the fork on the toe
Pinprick Sensation
- Apply a disposable pin just proximal to the toenail on the dorsal surface of the hallux, with enough pressure to deform the skin
- Inability to perceive pinprick over either hallux is an abnormal result
Vibration Perception Threshold (VPT)
- Use a biothesiometer to assess VPT semiquantitatively
- Place the stylus over the dorsal hallux and increase the amplitude until the patient can detect the vibration
- Record the resulting number as the VPT
- Take a mean of three readings over each hallux
- A VPT greater than 25 V is considered abnormal
Diabetic Foot Statistics
- Diabetic foot ulcers are a common complication of diabetes with a global annual incidence of 6.3%.
- Over half of diabetic ulcers become infected, and 20% of those with moderate to severe infection require amputation.
- Nearly 85% of amputations related to diabetes are preceded by ulceration.
- Regular foot exams can significantly decrease amputation rates by 45-85%.
Pathogenesis of Ulceration
- The most common pathway leading to diabetic foot ulcers begins with neuropathy, which often leads to foot deformities.
- These deformities make the foot susceptible to trauma, particularly repetitive microtrauma from pressure, friction, and shearing forces on soft tissue.
- Other contributing risk factors include:
- Previous ulceration or amputation
- Peripheral artery disease (PAD) or peripheral vascular disease (PVD)
- Foot deformities
- Peripheral neuropathy
- Poor glycemic control
- Visual impairment
- Nephropathy
- Smoking
Diabetic Foot Exam
- Patients with sensory loss, previous foot ulcers, or amputations should undergo a diabetic foot exam at every visit.
Visual Inspection
- Evaluate the skin for:
- Color changes
- Thickness
- Dryness
- Cracking
- Sweating
- Infection (especially between toes for fungal infections)
- Ulceration
- Calluses/Blistering: Note any evidence of hemorrhage into calluses.
- Examine the musculoskeletal system for:
- Deformities such as claw toes, prominent metatarsal heads, and Charcot foot deformities.
- Muscle wasting (guttering between the metatarsals).
Footwear Inspection
- Assess footwear for potential trauma:
- Are shoes wide and deep enough to accommodate the feet and any deformities?
- Do shoes show excessive wear, suggesting loss of protective padding?
- Are shoes too short? (Hint: Remove the insole and check the imprint of the longest toe. There should be a finger-length space between the toe and the end of the insole).
- Examine socks:
- Are they present?
- Are they worn out or constricting?
Screen for PAD
- Palpate the dorsalis pedis and posterior tibialis pulses.
- Inspect for physical signs of PAD:
- Hair loss
- Pallor or cyanosis
- Skin thinning
- Ulceration
- Obtain an ankle-brachial index (ABI) if:
- There are signs or symptoms of vascular disease.
- Pulses are absent on examination.
Neurologic/Protective Sensation
- Loss of protective sensation (LOPS) is a significant risk factor for ulceration.
- Perform the 10g monofilament test and at least one of the following four tests:
- Vibration using a 128-Hz tuning fork
- Pinprick sensation
- Ankle reflexes
- Vibration perception threshold (VPT)
10g Monofilament Exam
- The patient should close their eyes during the test.
- Demonstrate the sensation of pressure using the buckling 10-g monofilament on a proximal site (e.g. upper arm, thigh) to familiarize the patient.
- Test the foot by asking the patient to respond "yes" or "no" when asked if they feel the monofilament.
- Avoid calloused areas when testing for pressure perception.
Vibration using a 128Hz Tuning Fork
- Test vibratory sensation over the tip of the great toe bilaterally.
- An abnormal response occurs when the patient loses vibratory sensation, but the examiner can still feel the vibration while holding the tuning fork on the toe.
Pinprick Sensation
- Apply a disposable pin just proximal to the toenail on the dorsal surface of the hallux, using enough pressure to deform the skin.
- Inability to perceive pinprick on either hallux is an abnormal finding.
Ankle Reflexes
- Assess the ankle reflexes.
Vibration Perception Threshold (VPT)
- Use a biothesiometer to assess VPT semi-quantitatively.
- With the patient supine, place the stylus of the instrument over the dorsal hallux and increase the amplitude until the patient detects the vibration.
- The resulting number is the VPT.
- Obtain three readings over each hallux for an average.
- A VPT greater than 25 V is considered abnormal.
Diabetic Foot Statistics
- Diabetic foot ulcerations are a common diabetes complication
- The global annual incidence of diabetic foot ulcerations is 6.3%
- Over 50% of diabetic ulcers become infected, and 20% of those with moderate to severe infections lead to amputation
- Nearly 85% of diabetes-related amputations are preceded by ulceration
- Regular foot exams can reduce amputation rates by 45-85%
Pathogenesis of Ulceration
- The most common pathway to ulceration is neuropathy, leading to foot deformities and trauma
- Repetitive microtrauma from pressure, friction, and shearing forces on soft tissue contribute to ulceration
- Other risk factors include prior ulceration/amputation, PAD/PVD, foot deformities, peripheral neuropathy, poor glycemic control, visual impairment, nephropathy, and smoking
Diabetic Foot Exam
- A comprehensive medical evaluation and assessment of comorbidities is recommended for patients with sensory loss, previous foot ulcers, or amputations
- Diabetic foot exams should be performed at every visit
Visual Inspection
- Inspect for skin abnormalities: color, thickness, dryness, cracking, sweating, infection, ulceration, calluses/blistering
- Check between toes for fungal infections
- Examine musculoskeletal deformities such as claw toes, prominent metatarsal heads, Charcot joint
- Assess muscle wasting between metatarsals
- Inspect footwear for signs of trauma: shoes should be wide and deep enough to accommodate feet/deformities, without excessive wear, loss of protective padding, or being too short
- Inspect socks for signs of wear, constriction, or absence
Screen for PAD
- Check dorsalis pedis and posterior tibialis pulses
- Inspect for signs of PAD including hair loss, pallor/cyanosis, thinning of skin, ulceration
- If necessary, check or refer for ABI if there are signs and symptoms of vascular disease or absent pulses on exam
Neurologic/Protective Sensation
- Loss of protective sensation (LOPS) is a high-risk factor for ulceration
- Perform a 10g monofilament exam, plus one of the following four tests: vibration (128-Hz tuning fork), pinprick sensation, ankle reflexes, and vibration perception threshold (VPT)
10g Monofilament Exam
- The patient should close their eyes while being tested.
- Demonstrate the sensation of pressure using the buckling 10-g monofilament on a proximal site (e.g., upper arm, thigh)
- Examine foot sites by asking the patient if they feel the monofilament being applied
- Avoid areas of callus when testing
Vibration
- Test vibratory sensation over the tip of the great toe bilaterally
- An abnormal response is when the patient loses vibratory sensation, but the examiner can still perceive it while holding the fork on the tip of the toe
Pinprick Sensation
- Apply a disposable pin just proximal to the toenail on the dorsal surface of the hallux, with just enough pressure to deform the skin
- Inability to perceive pinprick over either hallux is considered an abnormal test result
Ankle Reflexes
- No details provided in the text on how to perform this.
Vibration Perception Threshold (VPT)
- Use a biothesiometer to assess VPT semi-quantitatively
- With the patient lying supine, place the stylus of the instrument over the dorsal hallux, increasing the amplitude until the patient can detect the vibration
- Record the VPT (amplitude at which vibration is detected)
- Take a mean of three readings over each hallux
- A VPT greater than 25 V is considered abnormal
Risk Classification & Follow-up
- No further information provided.
Diabetic Foot Statistics
- Diabetic foot ulcerations are one of the most common complications associated with diabetes.
- The annual global incidence of diabetic foot ulcerations is 6.3%.
- Over 50% of diabetic ulcers become infected, and 20% of those with moderate to severe infection result in amputation.
- Nearly 85% of diabetes-related amputations are preceded by an ulceration.
- Regular foot exams can reduce amputation rates by 45-85%.
Pathogenesis of Ulceration
- The most common pathway to ulceration starts with neuropathy, leads to foot deformities and then trauma.
- Trauma is often repetitive microtrauma involving pressure, friction, and shearing forces on the soft tissue.
- Other risk factors for ulceration include previous ulceration/amputation, PAD/PVD, foot deformity, peripheral neuropathy, poor glycemic control, visual impairment, nephropathy, and smoking.
Visual Inspection
- Examine skin status - color, thickness, dryness, cracking, sweating, infection, ulceration, calluses/blistering, hemorrhage into callus.
- Look between toes for signs of fungal infection.
- Examine musculoskeletal status for deformities (e.g., claw toes, prominent metatarsal heads, Charcot joint) and muscle wasting (guttering between metatarsals).
- Inspect footwear for signs of trauma. Look for shoes that are too narrow, too short, or have excessive wear.
- Inspect socks and ensure they are present, not worn out, and not too constricting.
Screening for PAD
- Check dorsalis pedis and posterior tibialis pulses.
- Inspect for physical signs of PAD (e.g., hair loss, pallor/cyanosis, thinning of skin, ulceration).
- If there are signs or symptoms of vascular disease or absent pulses on exam, check or refer for an ankle-brachial index (ABI).
Neurologic/Protective Sensation
- Loss of protective sensation (LOPS) is a high risk factor for ulceration.
- Recommend performing a 10g monofilament test plus one of the following 4 tests: vibration using a 128-Hz tuning fork, pinprick sensation, ankle reflexes, and vibration perception threshold (VPT).
10g Monofilament Exam
- Patients should close their eyes during the exam.
- Demonstrate the sensation of pressure using the buckling 10g monofilament on a proximal site (e.g., upper arm or thigh) before testing the foot.
- Ask the patient to respond "yes" or "no" when asked whether the monofilament is being applied to a particular site.
- Avoid areas of callus when testing for pressure perception.
Vibration using a 128-Hz Tuning Fork
- Test vibratory sensation over the tip of the great toe bilaterally.
- An abnormal response occurs when the patient loses vibratory sensation, but the examiner still perceives it while holding the fork on the tip of the toe.
Pinprick Sensation
- Apply a disposable pin just proximal to the toenail on the dorsal surface of the hallux with just enough pressure to deform the skin.
- Inability to perceive pinprick over either hallux indicates an abnormal test result.
Vibration Perception Threshold (VPT)
- Use a biothesiometer to assess VPT semi-quantitatively.
- Place the stylus of the instrument over the dorsal hallux and increase the amplitude until the patient can detect the vibration.
- Record the resulting number as the VPT.
- Take a mean of three readings over each hallux.
- A VPT >25 V is considered abnormal.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.