Podcast
Questions and Answers
What is the primary focus of implant therapy according to the presentation?
What is the primary focus of implant therapy according to the presentation?
- To enhance oral hygiene and maintenance
- To improve the aesthetics of dental arches
- To enable single-tooth replacement without restoring adjacent teeth (correct)
- To provide a permanent solution for dental caries
Which grade of complication involves a life-threatening situation requiring hospitalization?
Which grade of complication involves a life-threatening situation requiring hospitalization?
- Grade 2
- Grade 1
- Grade 3
- Grade 4 (correct)
What is a significant issue contributing to complications in implant therapy?
What is a significant issue contributing to complications in implant therapy?
- Increase in implant popularity among specialists
- Flawed success rates due to lack of scientific understanding (correct)
- Improved communication between patients and dentists
- High patient satisfaction rates
Which of these factors is NOT considered a local or systemic factor in complications during implant therapy?
Which of these factors is NOT considered a local or systemic factor in complications during implant therapy?
What is a key area of focus for prevention in implant therapy?
What is a key area of focus for prevention in implant therapy?
Which complication grade requires pharmacologic intervention?
Which complication grade requires pharmacologic intervention?
What major issue is highlighted regarding the training for implant therapy?
What major issue is highlighted regarding the training for implant therapy?
Which of the following best describes the classification of surgical complications?
Which of the following best describes the classification of surgical complications?
What characterizes an avoidable complication?
What characterizes an avoidable complication?
Which of the following represents a reversible complication?
Which of the following represents a reversible complication?
What is true about unavoidable complications?
What is true about unavoidable complications?
Which complication might occur immediately post-surgery?
Which complication might occur immediately post-surgery?
What is a common issue for patients on anticoagulants such as warfarin during dental procedures?
What is a common issue for patients on anticoagulants such as warfarin during dental procedures?
Which option refers to a complication related to the implant design?
Which option refers to a complication related to the implant design?
Which of the following complications is related to systemic issues?
Which of the following complications is related to systemic issues?
What is a characteristic of major complications compared to minor ones?
What is a characteristic of major complications compared to minor ones?
What is primarily the patient's responsibility in preventing peri-implantitis?
What is primarily the patient's responsibility in preventing peri-implantitis?
What is a common clinical feature of peri-implantitis?
What is a common clinical feature of peri-implantitis?
What should be done if probing depths exceed 6 mm despite significant bone loss?
What should be done if probing depths exceed 6 mm despite significant bone loss?
Which oral bacteria are commonly found in peri-implantitis lesions?
Which oral bacteria are commonly found in peri-implantitis lesions?
What action is recommended if the implant restoration is in occlusion?
What action is recommended if the implant restoration is in occlusion?
What is indicated for mild bone loss with probing depths of 4 to 6 mm?
What is indicated for mild bone loss with probing depths of 4 to 6 mm?
What happens if there is mobility of implants?
What happens if there is mobility of implants?
Which conditions can influence the diagnosis of peri-implantitis?
Which conditions can influence the diagnosis of peri-implantitis?
What factors should be optimized to increase primary stability in cases of low bone quality?
What factors should be optimized to increase primary stability in cases of low bone quality?
What is the potential consequence of injury to the inferior alveolar nerve (IAN) during dental implant surgery?
What is the potential consequence of injury to the inferior alveolar nerve (IAN) during dental implant surgery?
Which surgical technique has weak evidence suggesting it could enhance primary stability in sites of poor bone density?
Which surgical technique has weak evidence suggesting it could enhance primary stability in sites of poor bone density?
What is a common cause of IAN injury during dental implant procedures?
What is a common cause of IAN injury during dental implant procedures?
How does undersized drilling influence primary implant stability?
How does undersized drilling influence primary implant stability?
What is the reported incidence range of IAN injury following dental implant surgery?
What is the reported incidence range of IAN injury following dental implant surgery?
Which of the following techniques does NOT provide strong evidence for enhancing primary stability in poor bone density?
Which of the following techniques does NOT provide strong evidence for enhancing primary stability in poor bone density?
What effect does using a wrong implant drilling system have during surgery?
What effect does using a wrong implant drilling system have during surgery?
What is a potential consequence of the mental foramen location in an edentulous mandible?
What is a potential consequence of the mental foramen location in an edentulous mandible?
Which imaging technique is used for treatment planning to avoid the mandibular canal?
Which imaging technique is used for treatment planning to avoid the mandibular canal?
What should be done if a drill has gone too apical during an implant procedure?
What should be done if a drill has gone too apical during an implant procedure?
What is a sign of potential injury to the inferior alveolar nerve (IAN)?
What is a sign of potential injury to the inferior alveolar nerve (IAN)?
Which type of medication has been suggested to reduce inflammation at the site of injury?
Which type of medication has been suggested to reduce inflammation at the site of injury?
What class of drugs is commonly used for non-specific neuropathic pain (NP)?
What class of drugs is commonly used for non-specific neuropathic pain (NP)?
What is the recommended action for a gross injury observed in the mandibular canal or IAN?
What is the recommended action for a gross injury observed in the mandibular canal or IAN?
When is local infiltration preferred over a nerve block during drilling in the posterior mandible?
When is local infiltration preferred over a nerve block during drilling in the posterior mandible?
Study Notes
Introduction
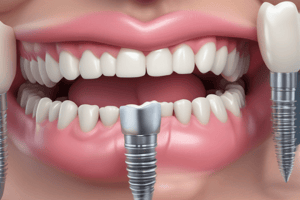
- Endosseous implants have revolutionized dental treatment
- Implants enable single-tooth replacement without restoring adjacent teeth
Definition and Scope of the Problem
- Huge upsurge in the number of implants placed
- Poor Treatment Planning
- Implants being provided in compromised patients and sites
- Flawed Success rates causing lack of scientific understanding
Classification of Complications
- Grade 1: Any deviation from the normal postoperative course that does not require pharmacologic intervention
- Grade 2: Any deviation from the normal postoperative course that does require pharmacologic intervention
- Grade 3: A deviation that requires surgical intervention
- Grade 4: Life-threatening complication requiring hospitalization
Complications
- Reversible: Usually resolve on their own and have no associated long-term morbidity
- Irreversible: Permanent and cannot be reversed, thus having increased severity and consequences
Types of Complications
- Assessment and Treatment Planning:
- Compromised Patients
- Compromised Sites
- Surgery Related:
- Immediate
- Delayed
- Prosthesis Related:
- Incorrect design
- Restorative failure
- Patient Related:
- Maintenance
- Habits
Immediate Complications
- Poor Stability
- Implant Exposure
- Wrong Position
- Implant Fracture
- Nerve Injury
- Oro-Antral Communication
- Bleeding
- Displacement
Late Complications
- Flap Necrosis
- Peri-Implantitis
- Loss of Graft
- Donor/Graft site Infection
Bleeding
- Minor bleed is common, major bleeding is uncommon and can be life-threatening
- Systemic issues relate to medications and coagulopathies
- For patients taking warfarin, the overall frequency of persistent bleeding (2%) is low when all dental procedures are considered.
- When extractions are combined with the placement of an implant, the incidence of persistent bleeding increases to 4.8%.
Implant Diameter and Length
- Aim: evaluate the influence of mechanical characteristics of the implant on primary stability in different bone types, based on resonance frequency analysis (RFA)
- Conclusion: In cases of low bone quality, the optimum increase in the implant length and diameter should be taken into account to achieve higher primary stability.
Surgical Techniques
- Undersized drilling: weak evidence that it could enhance the primary implant stability in sites of poor bone density
- Osteotome technique: weak evidence that in poor bone density could enhance the primary stability
- Flapless: There is a weak evidence suggesting that could enhance the primary stability
Nerve Injury
- Injury to the IAN can result in partial or complete paresthesia, analgesia, anesthesia, or in rare cases dysesthesia, to the structures it innervates
- The incidence of IAN injury secondary to dental implant surgery is variable, with a range of 0% to 44% in the literature.
- The etiology of IAN injury is usually associated with inadequate planning or overzealous implant placement.
Prevention of Nerve Injury
- Cone beam computerized tomograms (CBCTs) or conventional computed tomography (CT) scans can be utilized as part of the treatment planning phase to not only plan for implant size, location, and vector of placement, but also to identify and avoid the mandibular canal.
- Intraoperatively, utilizing CT-based surgical guides can also protect the IAN.
- Other options include taking radiographs step by step during the procedure.
- If the radiograph indicates that the canal is violated, clinical assessment can give clues to the extent of injury (if any).
- Use of local infiltration as opposed to nerve block can also maintain patient feedback while drilling in the posterior mandible.
- Topical dexamethasone has been suggested to reduce inflammation in the site of injury.
Treatment of Nerve Injury
- If there is witnessed gross injury to the mandibular canal or IAN, then immediate referral to a microsurgery specialist for treatment is indicated
- Pharmacotherapy for NP includes a variety of agents
- Tricyclic antidepressants drugs, such as amitriptyline, desipramine, and nortriptyline.
- Serotonin and norepinephrine reuptake inhibitors, such as duloxetine and venlafaxine
- Anticonvulsants drugs, such as gabapentin and pregabalin
- Local anesthetics are often used as a diagnostic tool
- Topical medications, such as lidocaine or benzocaine, can be helpful in reducing local pain.
Perforation
- perforation that occurs with the pilot drill is minor: shortening the length of the subsequent osteotomies is enough to avoid significant damage to the underlying membrane.
Peri-Implantitis
- This film has been shown to attach and colonize within minutes to an hour after placement and then exponentially proliferate
Clinical Features of Peri-Implantitis
- can be clinically stable or symptomatic:
- mobility of implant, purulent or serosanguinous drainage, foul odor, gingival bleeding, or rarely, pain.
- surrounding tissues may appear edematous or tender on examination
Radiographic Features of Peri-Implantitis
- Loss of alveolar bone
Prevention of Peri-Implantitis
- Prevention of peri-implantitis is primarily on the patient’s shoulders to maintain excellent oral hygiene. The surgeon, however, needs to educate the patient on hygiene importance and procedure.
- Once the endosseous implants have been restored, it is the responsibility of the restorative dentist to ensure that the dental prosthesis is easily cleansable and does not create areas for plaque build-up around the implants.
Treatment of Peri-Implantitis
- Minimal bone loss and probing depths of less than 4 mm usually require plaque and calculus removal, polishing of the implant crown, and increased oral hygiene visits annually.
- Mild bone loss and probing depths of 4 to 6mmrequire, in addition to increased hygiene visits, chlorhexidine rinses daily or the application of chlorhexidine gels to the affected area.
- If probing depths increase beyond 6 mm of significant bone loss (implant still stable), then in addition to hygiene and rinsing, systemic antibiotics focused on gram-negative coverage (metronidazole) is administered for 10 days.
- Once any suppuration, edema, and/or infection has resolved, it is reasonable to consider guided tissue regenerative procedures with allogenic bone grafting to restore bone height around the implant.
- If the implant is restored, the restoration should be taken out of occlusion to minimize functional loads.
- Mobility of implants results in implant failure, and removal is required with possible bone grafting if desired
Key Points Regarding Peri-Implantitis
- The diagnosis of peri-implantitis benefits from clinical, radiographic, microbiological, and biological information.
- Practitioners and patients can use biomarkers to identify risk of disease, disease activity, disease progression, and response to therapy.
- Peri-implantitis is a biofilm-induced condition. The microbial composition of periimplantitis lesions is mixed, nonspecific, and less diverse than that of periodontitis but includes Fusobacterium, Prevotella, Porphyromonas, Streptococcus, Campylobacter, and Neisseria species.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the essential aspects of endosseous implants in dental treatment, including their revolutionary impact, the definition and scope of related complications, and a classification of these complications. Test your understanding of the various grades of complications and their implications for patient care.