Podcast
Questions and Answers
Which of the following is NOT a primary function of connective tissue?
Which of the following is NOT a primary function of connective tissue?
- Connecting and binding tissues and organs.
- Facilitating nutrient absorption in the digestive system. (correct)
- Providing structural support for the body.
- Transporting substances throughout the body.
What distinguishes connective tissue from other tissue types in terms of its composition?
What distinguishes connective tissue from other tissue types in terms of its composition?
- The consistent presence of contractile proteins for movement.
- A singular cell type specialized for rapid electrical signaling.
- A prominent extracellular matrix (ECM) composed of protein fibers and ground substance. (correct)
- A high concentration of tightly packed cells with minimal extracellular matrix (ECM).
How do resident cells in connective tissue proper differ functionally from migrant cells?
How do resident cells in connective tissue proper differ functionally from migrant cells?
- Resident cells primarily participate in immune responses, while migrant cells maintain the ECM.
- Resident cells and migrant cells are different names for the same cells.
- Resident cells permanently inhabit the tissue performing maintenance, while migrant cells move in and out for specific needs like defense and repair. (correct)
- Migrant cells regulate the ECM, whereas resident cells act in transport.
Which of the following is the primary role of fibroblasts in connective tissue?
Which of the following is the primary role of fibroblasts in connective tissue?
In what way does connective tissue contribute to the body's immune function?
In what way does connective tissue contribute to the body's immune function?
If a patient has a condition that impairs their ability to produce collagen, which type of cell is most likely affected?
If a patient has a condition that impairs their ability to produce collagen, which type of cell is most likely affected?
Which of these tissues is considered a connective tissue?
Which of these tissues is considered a connective tissue?
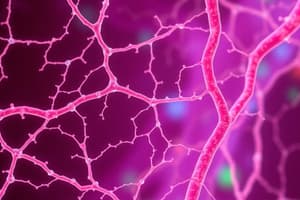
Which connective tissue type transports nutrients and waste throughout the body?
Which connective tissue type transports nutrients and waste throughout the body?
Which of the following best describes the primary function of fibroblasts in connective tissue proper?
Which of the following best describes the primary function of fibroblasts in connective tissue proper?
How do mast cells contribute to the body's defense mechanisms in connective tissue proper?
How do mast cells contribute to the body's defense mechanisms in connective tissue proper?
Which characteristic distinguishes adipocytes from other cells found in connective tissue proper?
Which characteristic distinguishes adipocytes from other cells found in connective tissue proper?
How do macrophages contribute to the function of connective tissue proper?
How do macrophages contribute to the function of connective tissue proper?
What is the primary difference between resident and migrant immune cells in connective tissue proper?
What is the primary difference between resident and migrant immune cells in connective tissue proper?
Which of the following is NOT considered a basic type of connective tissue proper?
Which of the following is NOT considered a basic type of connective tissue proper?
A sample from a tissue biopsy shows a large number of cells with granules containing histamine. Which cell type is most likely prevalent in this sample?
A sample from a tissue biopsy shows a large number of cells with granules containing histamine. Which cell type is most likely prevalent in this sample?
In a tissue undergoing repair, which cell type would you expect to be most active in synthesizing new extracellular matrix?
In a tissue undergoing repair, which cell type would you expect to be most active in synthesizing new extracellular matrix?
Which type of connective tissue proper is characterized by predominantly parallel-oriented elastic fibers and randomly oriented collagen fibers?
Which type of connective tissue proper is characterized by predominantly parallel-oriented elastic fibers and randomly oriented collagen fibers?
The walls of large blood vessels need to stretch to accommodate changes in blood volume. Which type of connective tissue is most likely found in their walls?
The walls of large blood vessels need to stretch to accommodate changes in blood volume. Which type of connective tissue is most likely found in their walls?
Reticular tissue forms a network to trap old and foreign cells. Where is reticular tissue typically found performing this function?
Reticular tissue forms a network to trap old and foreign cells. Where is reticular tissue typically found performing this function?
Which type of fiber is predominant in reticular tissue?
Which type of fiber is predominant in reticular tissue?
Besides fat storage, what are the other key functions of adipose tissue?
Besides fat storage, what are the other key functions of adipose tissue?
Adipose tissue primarily consists of adipocytes and what other components?
Adipose tissue primarily consists of adipocytes and what other components?
What is a primary role of reticular tissue found in the liver and bone marrow?
What is a primary role of reticular tissue found in the liver and bone marrow?
How does the structure of dense regular elastic connective tissue contribute to its function?
How does the structure of dense regular elastic connective tissue contribute to its function?
Which of the following is a primary function of loose connective tissue in relation to epithelial tissue?
Which of the following is a primary function of loose connective tissue in relation to epithelial tissue?
Which characteristic of elastic cartilage makes it suitable for structures like the external ear?
Which characteristic of elastic cartilage makes it suitable for structures like the external ear?
Considering the structure of dense irregular connective tissue, what property makes it suitable for the dermis of the skin?
Considering the structure of dense irregular connective tissue, what property makes it suitable for the dermis of the skin?
Which of the following describes the inorganic component of bone extracellular matrix?
Which of the following describes the inorganic component of bone extracellular matrix?
How does the arrangement of collagen fibers in dense regular connective tissue contribute to its primary function?
How does the arrangement of collagen fibers in dense regular connective tissue contribute to its primary function?
How does increased tension affect bone remodeling?
How does increased tension affect bone remodeling?
Which component of loose connective tissue provides the most significant contribution to the body's immune response?
Which component of loose connective tissue provides the most significant contribution to the body's immune response?
Which of the following processes is primarily carried out by osteoblasts?
Which of the following processes is primarily carried out by osteoblasts?
If a tissue sample shows predominantly disorganized collagen bundles, placing it under stress in multiple directions would most likely demonstrate:
If a tissue sample shows predominantly disorganized collagen bundles, placing it under stress in multiple directions would most likely demonstrate:
What is the primary role of osteocytes within bone tissue?
What is the primary role of osteocytes within bone tissue?
Considering the structure and location of dense regular connective tissue, which injury is most likely to damage this type of tissue?
Considering the structure and location of dense regular connective tissue, which injury is most likely to damage this type of tissue?
How do osteoclasts contribute to bone remodeling?
How do osteoclasts contribute to bone remodeling?
How does the composition of loose connective tissue contribute to its role beneath epithelial tissue?
How does the composition of loose connective tissue contribute to its role beneath epithelial tissue?
In a comparison between dense regular and dense irregular connective tissues, which best describes their structural difference and functional consequence?
In a comparison between dense regular and dense irregular connective tissues, which best describes their structural difference and functional consequence?
If a patient experiences prolonged inactivity, which cellular activity would be expected to increase in their bones?
If a patient experiences prolonged inactivity, which cellular activity would be expected to increase in their bones?
Which of the following best describes the periosteum's relationship with osteoblasts?
Which of the following best describes the periosteum's relationship with osteoblasts?
Why is the limited thickness of living cartilage related to its avascular nature?
Why is the limited thickness of living cartilage related to its avascular nature?
How does the composition of hyaline cartilage contribute to its function in joints?
How does the composition of hyaline cartilage contribute to its function in joints?
What is the primary difference between hyaline cartilage and fibrocartilage in terms of ECM composition?
What is the primary difference between hyaline cartilage and fibrocartilage in terms of ECM composition?
In which of the following locations would you expect to find hyaline cartilage?
In which of the following locations would you expect to find hyaline cartilage?
How does the presence of fibroblasts in fibrocartilage contribute to its unique properties?
How does the presence of fibroblasts in fibrocartilage contribute to its unique properties?
What is the functional significance of fibrocartilage forming articular discs in joints?
What is the functional significance of fibrocartilage forming articular discs in joints?
What property of cartilage is most affected by its avascularity?
What property of cartilage is most affected by its avascularity?
Why is hyaline cartilage present in the fetal skeleton?
Why is hyaline cartilage present in the fetal skeleton?
Flashcards
Histology
Histology
The study of tissues.
Connective Tissue Groups
Connective Tissue Groups
Connective tissue divided into two basic groups, differing in cell types and ECM components.
Connective Tissue Functions
Connective Tissue Functions
Includes connecting, supporting, protecting, and transporting.
Connective Tissue Components
Connective Tissue Components
Cells surrounded by protein fibers & ground substance.
Signup and view all the flashcards
Extracellular Matrix (ECM)
Extracellular Matrix (ECM)
Plays a role in the function of connective tissue type.
Signup and view all the flashcards
Connective Tissue Proper
Connective Tissue Proper
Widely distributed and connects tissues and organs.
Signup and view all the flashcards
Resident Cells
Resident Cells
Reside in the tissue. Examples: fibroblasts, adipocytes, mast cells, phagocytes.
Signup and view all the flashcards
Migrant Cells
Migrant Cells
Migrate to different areas of the body based on situation.
Signup and view all the flashcards
Fibroblasts
Fibroblasts
Most common resident cell in connective tissue proper that make ECM components.
Signup and view all the flashcards
Adipocytes
Adipocytes
Connective tissue cells filled with a large lipid inclusion.
Signup and view all the flashcards
Mast Cells
Mast Cells
The largest resident immune cell filled with inflammatory mediators.
Signup and view all the flashcards
Phagocytes
Phagocytes
Immune cells that ingest foreign substances, microorganisms, and dead cells via phagocytosis.
Signup and view all the flashcards
Macrophages
Macrophages
A type of phagocyte that can be resident or migrant.
Signup and view all the flashcards
Neutrophils
Neutrophils
Migrant phagocytic immune cells.
Signup and view all the flashcards
Loose connective tissue
Loose connective tissue
A basic type of connective tissue proper.
Signup and view all the flashcards
Dense connective tissue
Dense connective tissue
A basic type of connective tissue proper known for its strength.
Signup and view all the flashcards
Location of Loose Connective Tissue
Location of Loose Connective Tissue
Beneath skin epithelium, lines body cavities, and within hollow organ walls.
Signup and view all the flashcards
Function of Loose Connective Tissue
Function of Loose Connective Tissue
It contains and supports blood vessels vital to avascular epithelial tissues and houses immune system cells.
Signup and view all the flashcards
Dense Irregular Connective Tissue
Dense Irregular Connective Tissue
Predominantly disorganized collagen bundles.
Signup and view all the flashcards
Function of Dense Irregular Tissue
Function of Dense Irregular Tissue
Resists tension in all three planes of movement.
Signup and view all the flashcards
Location of Dense Irregular Tissue
Location of Dense Irregular Tissue
In high tension areas such as dermis, surrounding organs, and joints
Signup and view all the flashcards
Dense Regular Connective Tissue
Dense Regular Connective Tissue
Organized into parallel collagen bundles.
Signup and view all the flashcards
Dense Regular Elastic Connective Tissue
Dense Regular Elastic Connective Tissue
Mostly parallel-oriented elastic fibers with randomly oriented collagen fibers. Found in walls of organs that stretch, like blood vessels and certain ligaments.
Signup and view all the flashcards
Reticular Tissue
Reticular Tissue
A type of connective tissue proper, forms a fine network to support small structures.
Signup and view all the flashcards
Reticular Cells
Reticular Cells
Reticular fibers produced by these cells form supporting networks.
Signup and view all the flashcards
Function of Reticular Tissue
Function of Reticular Tissue
Supports blood and lymphatic vessels/Supports epithelia and internal structure of liver and bone marrow
Signup and view all the flashcards
Adipose Tissue
Adipose Tissue
Connective tissue with fat-storing adipocytes, fibroblasts, and ECM.
Signup and view all the flashcards
Functions of Adipose Tissue
Functions of Adipose Tissue
Fat storage (major energy reserve), insulation (retains warmth), and shock absorption/protection.
Signup and view all the flashcards
Fat Storage
Fat Storage
Major energy reserve of body
Signup and view all the flashcards
Avascular Cartilage
Avascular Cartilage
Cartilage lacks blood vessels; nutrients diffuse from the perichondrium.
Signup and view all the flashcards
Perichondrium
Perichondrium
Outer sheath of dense irregular collagenous connective tissue providing limited blood supply to cartilage.
Signup and view all the flashcards
Hyaline Cartilage
Hyaline Cartilage
Most common type of cartilage; glossy bluish-gray appearance due to fine collagen bundles.
Signup and view all the flashcards
Articular Cartilage
Articular Cartilage
Cartilage found on the ends of bones in joints.
Signup and view all the flashcards
Sternocostal Cartilage
Sternocostal Cartilage
Hyaline cartilage that connects the sternum to the ribs.
Signup and view all the flashcards
Fibrocartilage
Fibrocartilage
Cartilage filled with collagen fibers; great tensile strength.
Signup and view all the flashcards
Fibroblasts in Cartilage
Fibroblasts in Cartilage
Cells found in fibrocartilage that produce collagen and some elastic fibers.
Signup and view all the flashcards
Articular Discs
Articular Discs
Joint structures made of fibrocartilage that improve bone fit.
Signup and view all the flashcards
Elastic Cartilage
Elastic Cartilage
Mostly elastic fibers in ECM. Allows tissue to vibrate.
Signup and view all the flashcards
Bone ECM Composition
Bone ECM Composition
ECM is 35% organic (collagen fibers and osteoid) and 65% inorganic calcium phosphate crystals.
Signup and view all the flashcards
Bone Remodeling
Bone Remodeling
Dynamic tissue capable of remodeling in response to stress or inactivity.
Signup and view all the flashcards
Osteoblasts
Osteoblasts
"Bone-builders" on outer surface of bones that carry out bone deposition.
Signup and view all the flashcards
Osteoblast Function
Osteoblast Function
Synthesize and secrete organic ECM and chemicals to trap calcium in the ECM.
Signup and view all the flashcards
Osteocytes
Osteocytes
Osteoblasts surrounded by ECM in lacunae; mostly inactive, but maintain bone.
Signup and view all the flashcards
Osteoclasts
Osteoclasts
Large, multinucleated cells that destroy bone via bone resorption.
Signup and view all the flashcards
Osteoclast Function
Osteoclast Function
Secrete hydrogen ions and enzymes to break down inorganic and organic ECM.
Signup and view all the flashcardsStudy Notes
Module 4.3 Connective Tissues
- Connective tissues are divided into two basic groups and differ in both cell types and ECM components. Categories are connective tissue proper and specialized connective tissue.
Connective Tissue Functions
- Anchor tissue layers in organs and link organs together, also known as connecting and binding.
- Bones and cartilage support the body.
- Bone tissue protects internal organs; cartilage and fat provide shock absorption; components of the immune system are throughout connective tissues and provide protection.
- Blood is fluid connective tissue, and the primary transport medium in the body, for transport.
Connective Tissue Components
- Consists of cells and extracellular matrix (ECM).
- Cells are surrounded by protein fibers and embedded in the ground substance.
- ECM is a crucial feature that plays an extensive role in connective tissue type function.
Connective Tissue Proper
- Widely distributed throughout the body and connects tissues and organs.
- A component of the internal architecture of some organs and is known as general connective tissue.
Connective Tissue Proper Cells
- Resident cells inhabit tissue permanently, and migrant cells migrate depending on the current situation.
- Fibroblasts are a type of cell.
- Adipocytes are a type of cell.
- Mast cells are a type of cell.
- Phagocytes are a type of cell.
- Other immune system cells are a type of cell.
Connective Tissue Proper Cells continued
- Fibroblasts are the most common resident cell, and they have mature cells with properties like immature "blast" cells. Fibroblasts make protein fibers and ground substance (components of ECM). Fibroblasts continually produce collagen proteins.
- Adipocytes (fat cells) are present in many different connective tissues, and the cytoplasm is filled with a single large lipid inclusion.
- Mast cells are the largest resident cell and immune system cells filled with cytosolic inclusions (granules) of inflammatory mediators (histamine). Mast cells release mediators (degranulate) when stimulated, causing inflammation that activates the immune system.
- Phagocytes are immune system cells, and they ingest foreign substances, microorganisms, and dead or damaged cells by phagocytosis. Macrophages (resident or migrant) and neutrophils (migrant cells) are also phagocytes.
- Other immune system cells are available and migrate depending on the body’s current needs.
Types of Connective Tissue Proper
- Loose connective tissue, dense connective tissue, reticular tissue, and adipose tissue.
Connective Tissue Types Explained
- Loose connective tissue (areolar tissue) includes mostly ground substance; contains all three types of protein fibers, fibroblasts, and occasionally adipocytes, suspended in ground substance. Located beneath epithelium of skin, in membranes lining body cavities, and within walls of hollow organs and contains/supports blood vessels vital to avascular epithelial tissues, and houses immune system cells.
- Dense connective tissue (fibrous connective tissue) is made of mostly protein fibers and comes in three classes.
Categories of Dense Connective Tissue
- Dense irregular connective tissue is primarily disorganized collagen bundles. It is strong and resists tension in all three planes of movement, especially in high tension areas such as the dermis (deep to the skin) and surrounding organs and joints.
- Dense regular connective tissue is organized into parallel collagen bundles that are subjected to tension in one plane of movement within tendons and ligaments.
- Dense regular elastic connective tissue (elastic tissue) and has mostly parallel-oriented elastic fibers, plus randomly oriented collagen fibers in the walls of organs that stretch to function, such as large blood vessels and certain ligaments.
- The arrangement of fibers in both the dense regular and irregular connective tissues is an example of structure-function core principle.
- Reticular tissue is mostly made of reticular fibers produced by fibroblasts (reticular cells). Reticular tissue forms fine networks that support small structures such as blood and lymphatic vessels. Reticular tissue is in lymph nodes and the spleen, forming web-like nets that trap old and foreign cells, and forms part of the basement membrane. Reticular tissue supports all epithelia and the internal structure of the liver and bone marrow.
- Adipose Tissue (Fat Tissue) consists of fat-storing adipocytes and is surrounded by fibroblasts and ECM. Adipocytes can increase to a point where fibroblasts and ECM are not visible, and its functions include fat storage (major energy reserve), insulation, and shock absorption/protection.
Adipose Tissue and Obesity
- Obesity is an excess of adipose tissue in proportion to lean body mass, and there are two forms.
Forms of Obesity
- Hypertrophic is when lipid inclusions accumulate fatty acids, increasing in size up to 4x normal size. The number of adipocytes remains unchanged.
- Hypercellular is generally more severe, with the number of adipocytes increasing. Hypercellular correlates with developing obesity in infancy or early childhood (not adulthood), and adult adipocytes cannot divide to form new cells.
- Both of these forms increase the risk of health problems. The development of related disorders is complex and depends on the distribution of adipose tissue and genetic factors.
Specialized Connective Tissues
- Specialized connective tissues have specified functions.
- Cartilage, bone tissue (osseous tissue), and blood are specialized connective tissue.
- Cartilage is located in joints between bones, ear, nose, and respiratory tract segments.
- Bone tissue supports the body, protects organs, provides attachments for muscles to allow movement, stores calcium, and contains bone marrow to store fat and produces blood cells.
Additional Information on the Types of Specialized Connective Tissues
- Cartilage is a tough, flexible tissue that supports the body. Cartilage absorbs shock and resists tension/compression/shearing forces. Its ECM consists of collagen and elastic fibers, proteoglycans, and glycosaminoglycans.
- Two cell types populate cartilage: chondroblasts and chondrocytes. Chondroblasts are immature cells that divide by mitosis and produce most of the ECM. Eventually, chondroblasts surround themselves in small cavities (lacunae) in the ECM to become mature, largely inactive chondrocytes.
Cartilage Properties
- Essentially avascular, unlike most connective tissues; blood supply is limited to the outer sheath (perichondrium) of dense irregular collagenous connective tissue.
- Oxygen and nutrients must diffuse from blood vessels in the perichondrium through the ECM to chondroblasts/chondrocytes. It limits the thickness of living cartilage.
- Cartilage can be of three types: hyaline cartilage, fibrocartilage, and elastic cartilage; categorized by ECM composition.
Cartilage Types Defined
- Hyaline cartilage, the more abundant cartilage, has ECM made of ground substance with small bundles of fine collagen. It gives the tissue a glossy bluish-gray appearance present on ends of bones in joints (articular cartilage), linking sternum to ribs, framing sections of respiratory tract, and in the nose.
- Fibrocartilage is filled with bundles of collagen fibers, so there is little room for substance in the ECM and is located between bones of fibrous joints, forming articular discs that improve the fit of bones in joints.
- Elastic cartilage has mostly elastic fibers in the ECM. The tissue vibrates. Elastic cartilage is limited to one part of the body, with the external ear assisting with the detection of sound in the air and the larynx assisting with the production of sound.
Bone
- The ECM contains about 35% organic components (collagen fibers and ground substance (osteoid)), and the remaining 65% is inorganic calcium phosphate, making bone one of the hardest substances in the body.
- Bone is dynamic tissue with the capability of being remodeled. Remodeling occurs in regions of stress or inactivity. Tension increases osteoblast activity/bone deposition, while compression increases the osteoclast activity and bone resorption.
Bone Cells
- Osteoblasts (bone-builders) are on the outer surface of the bones associated with a dense irregular collagenous connective tissue covering (periosteum).Osteoblasts perform bone deposition by synthesizing/secreting organic ECM plus chemicals to trap calcium in the ECM.
- Osteocytes are osteoblasts that have surrounded themselves with ECM in lacunae. They are known as mature cells, mostly inactive, and continue making/secreting substances important for bone maintenance.
- Osteoclasts are large, multinucleated bone destroyers that perform bone resorption by secreting hydrogen ions and enzymes that break down both inorganic and organic ECM.
- Blood’s ECM is fluid; unlike most, the ECM is fluid (plasma).
- Not like fibers found in other connective tissues, the smaller plasma proteins have functions including the transport of materials and blood clotting.
- Erythrocytes (red blood cells) bind to and transport oxygen throughout the body.
- Leukocytes (white blood cells) function for immunity in the body.
- Platelets are cell fragments and play a role in blood clotting.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.