Podcast
Questions and Answers
A patient with cirrhosis develops ascites. Which pathophysiological mechanism is the primary cause of this condition?
A patient with cirrhosis develops ascites. Which pathophysiological mechanism is the primary cause of this condition?
- Increased aldosterone secretion due to impaired liver metabolism, promoting sodium and water retention.
- Obstruction of hepatic lymph flow, resulting in lymphatic fluid accumulation in the abdomen.
- Increased portal venous pressure leading to renal sodium retention.
- Decreased synthesis of albumin by the liver, causing fluid shift into the peritoneal space. (correct)
A patient with chronic liver disease presents with increased bruising and bleeding tendencies. Which of the following best explains the etiology of this clinical manifestation?
A patient with chronic liver disease presents with increased bruising and bleeding tendencies. Which of the following best explains the etiology of this clinical manifestation?
- Increased production of clotting factors due to liver inflammation.
- Impaired absorption of iron, leading to decreased hemoglobin synthesis and impaired clotting.
- Accelerated destruction of platelets in the spleen due to portal hypertension.
- Decreased synthesis of vitamin K-dependent clotting factors by the liver. (correct)
A patient with cirrhosis experiences frequent episodes of hypoglycemia. What is the MOST likely reason for this?
A patient with cirrhosis experiences frequent episodes of hypoglycemia. What is the MOST likely reason for this?
- Decreased glycogen storage capacity in the liver. (correct)
- Increased insulin production due to impaired liver metabolism.
- Enhanced gluconeogenesis by the damaged liver.
- Impaired absorption of glucose from the intestines.
A patient with cirrhosis exhibits jaundice, dark urine, and clay-colored stools. Which pathophysiological process is responsible for these findings?
A patient with cirrhosis exhibits jaundice, dark urine, and clay-colored stools. Which pathophysiological process is responsible for these findings?
A patient with cirrhosis complains of severe itching (pruritus). Which of the following is the MOST likely cause of this symptom?
A patient with cirrhosis complains of severe itching (pruritus). Which of the following is the MOST likely cause of this symptom?
A patient with end-stage liver disease develops hepatic encephalopathy. Which of the following interventions is MOST appropriate to manage this condition?
A patient with end-stage liver disease develops hepatic encephalopathy. Which of the following interventions is MOST appropriate to manage this condition?
A patient with cirrhosis develops spontaneous bacterial peritonitis (SBP). Which of the following pathophysiological mechanisms contributes to the development of SBP?
A patient with cirrhosis develops spontaneous bacterial peritonitis (SBP). Which of the following pathophysiological mechanisms contributes to the development of SBP?
A patient with hepatitis A is being discharged from the hospital. Which of the following instructions is MOST important to include in the discharge teaching?
A patient with hepatitis A is being discharged from the hospital. Which of the following instructions is MOST important to include in the discharge teaching?
A healthcare worker sustains a needlestick injury from a patient who is positive for hepatitis B. What is the MOST appropriate immediate action?
A healthcare worker sustains a needlestick injury from a patient who is positive for hepatitis B. What is the MOST appropriate immediate action?
A patient is diagnosed with chronic hepatitis C. What is the PRIMARY goal of treatment for this patient?
A patient is diagnosed with chronic hepatitis C. What is the PRIMARY goal of treatment for this patient?
A patient is diagnosed with hepatitis D. What other hepatitis infection must be present for hepatitis D to occur?
A patient is diagnosed with hepatitis D. What other hepatitis infection must be present for hepatitis D to occur?
During the icteric phase of acute hepatitis, which clinical manifestations would the nurse expect to observe?
During the icteric phase of acute hepatitis, which clinical manifestations would the nurse expect to observe?
A patient with fulminant hepatitis is at high risk for which of the following complications?
A patient with fulminant hepatitis is at high risk for which of the following complications?
Which diagnostic test is MOST useful in determining the extent of liver damage in a patient with chronic hepatitis?
Which diagnostic test is MOST useful in determining the extent of liver damage in a patient with chronic hepatitis?
A patient with hepatitis A is being treated at home. Which of the following measures is MOST important for preventing the spread of infection to household contacts?
A patient with hepatitis A is being treated at home. Which of the following measures is MOST important for preventing the spread of infection to household contacts?
For which of the following groups is the hepatitis A vaccine MOST strongly recommended?
For which of the following groups is the hepatitis A vaccine MOST strongly recommended?
Which of the following individuals is at HIGHEST risk for contracting hepatitis B?
Which of the following individuals is at HIGHEST risk for contracting hepatitis B?
A patient with cirrhosis is prescribed a low-sodium diet. What is the PRIMARY rationale for this dietary restriction?
A patient with cirrhosis is prescribed a low-sodium diet. What is the PRIMARY rationale for this dietary restriction?
Which of the following medications is used to decrease endogenous ammonia production in a patient with hepatic encephalopathy?
Which of the following medications is used to decrease endogenous ammonia production in a patient with hepatic encephalopathy?
A patient with esophageal varices is scheduled for a transjugular intrahepatic portosystemic shunt (TIPS) procedure. What is the PRIMARY goal of this intervention?
A patient with esophageal varices is scheduled for a transjugular intrahepatic portosystemic shunt (TIPS) procedure. What is the PRIMARY goal of this intervention?
Flashcards
Cirrhosis
Cirrhosis
Chronic, progressive liver damage leading to decreased liver function.
Portal Hypertension
Portal Hypertension
Increased pressure in the portal vein, causing varicosities and ascites.
Ascites
Ascites
Accumulation of fluid in the peritoneal cavity due to hypoalbuminemia.
Altered Synthetic Function
Altered Synthetic Function
Signup and view all the flashcards
Hypoglycemia in Liver Disease
Hypoglycemia in Liver Disease
Signup and view all the flashcards
Jaundice
Jaundice
Signup and view all the flashcards
Pruritus in Liver Disease
Pruritus in Liver Disease
Signup and view all the flashcards
Hepatic Encephalopathy
Hepatic Encephalopathy
Signup and view all the flashcards
Spontaneous Bacterial Peritonitis
Spontaneous Bacterial Peritonitis
Signup and view all the flashcards
TIPS Procedure
TIPS Procedure
Signup and view all the flashcards
Lactulose
Lactulose
Signup and view all the flashcards
Hepatitis
Hepatitis
Signup and view all the flashcards
Hepatitis A
Hepatitis A
Signup and view all the flashcards
Hepatitis B
Hepatitis B
Signup and view all the flashcards
Hepatitis C
Hepatitis C
Signup and view all the flashcards
Hepatitis D
Hepatitis D
Signup and view all the flashcards
Prodromal Period (Hepatitis)
Prodromal Period (Hepatitis)
Signup and view all the flashcards
Icteric Period (Hepatitis)
Icteric Period (Hepatitis)
Signup and view all the flashcards
Fulminant Hepatitis
Fulminant Hepatitis
Signup and view all the flashcards
Treatment of Hepatitis
Treatment of Hepatitis
Signup and view all the flashcards
Study Notes
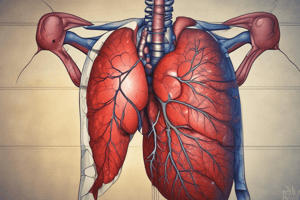
Cirrhosis
- Cirrhosis is a chronic, progressive, and irreversible condition causing decreased liver function due to diffuse liver damage.
- Key causes include viral hepatitis (B and C) and chronic alcohol abuse.
- In the US, chronic alcohol abuse is the most frequent cause, but worldwide it's viral hepatitis C.
- The liver becomes fibrotic with nodules, obstructing blood and bile flow leading to liver failure.
- Cirrhosis can take up to 40 years to develop.
Clinical Manifestations: Portal Hypertension
- Portal hypertension is a manifestation of cirrhosis.
- Portal hypertension causes varicosities in the esophagus and abdomen due to increased pressure, leading to bleeding (slow or severe).
- Ascites occur due to the liver's inability to produce albumin (hypoalbuminemia), causing fluid leakage into the peritoneal space.
Clinical Manifestations: Altered Synthetic Function
- Results in changes in clotting factors because the liver synthesizes vitamin K and clotting factors.
- Leads to bleeding tendencies.
- Muscle wasting occurs due to decreased protein levels and hypoalbuminemia.
Clinical Manifestations: Hypoglycemia
- The liver stores glycogen and releases glucose when blood sugar is low.
- Liver disease prevents glycogen storage, so patients experience chronic hypoglycemia.
Clinical Manifestations: Bile Accumulation
- Causes inflammation and necrosis, leading to jaundice (yellowing of the skin).
- Jaundice occurs when bilirubin backs up into the blood due to obstructed bile ducts.
- Results in brown urine and clay-colored stools.
Clinical Manifestations: Vitamin Deficiency and Pruritus
- Leads to fat-soluble vitamin (A, D, E, K) deficiencies due to impaired liver function.
- Intense itching (pruritus) occurs due to toxin buildup and ammonia buildup in the skin.
Clinical Manifestations: Hepatic Encephalopathy
- Ammonia builds up because the liver cannot convert it into urea (BUN).
- Increased ammonia levels affect the brain, causing confusion, loss of consciousness, and encephalopathy.
Clinical Manifestations: Spontaneous Bacterial Peritonitis
- The liver's Kupffer cells, responsible for phagocytosis, are impaired.
- Leads to increased bacteria in the GI tract and potential peritonitis.
Treatment for Cirrhosis
- Complex and depends on the underlying cause.
- Antiviral agents for hepatitis.
- Avoid alcohol and hepatotoxic drugs.
- Bile-acid binding agents aid in bile excretion.
Portal Hypertension Treatment
- Treated with surgically implanted shunts (TIPS procedure) to improve blood flow.
Ascites Treatment
- Fluid restriction and low-sodium diet.
- Diuretics.
- Paracentesis to remove fluid from the peritoneal cavity.
- Shunts may also be used.
Esophageal Varices Treatment
- Treated with endoscopic procedures (banding, shunts, sclerotherapy).
Encephalopathy Treatment
- Low-protein diet to eliminate the source of protein breakdown.
- Lactulose is prescribed to promote ammonia excretion in the stool.
- Antibiotics suppress intestinal flora and decrease endogenous ammonia production.
- Liver transplant is considered for end-stage liver disease.
Hepatitis Overview
- Hepatitis is an inflammation of the liver, usually caused by viral infections.
- Other causes include alcohol, medications (acetaminophen), and autoimmune diseases.
- Can be acute (e.g., hepatitis A, acetaminophen overdose) or chronic (e.g., hepatitis C).
Types of Hepatitis
- Non-viral hepatitis is not contagious, while viral hepatitis is.
- Hepatitis A, B, C, and D are endemic to the US, with B and C being the most common.
Hepatitis A
- Transmitted through the fecal-oral route (contaminated food/water).
- Does not cause chronic infection.
- There is a vaccine available.
Hepatitis B
- Transmitted through blood and body fluids (mucosa, sex, IV drug use).
- Can lead to chronic infection.
- There is a vaccine available.
Hepatitis C
- Transmitted through blood and body fluids (mucosa, sex, IV drug use).
- 80% of cases become chronic, leading to cirrhosis.
- Prevention includes blood donor screening and behavior modification.
Hepatitis D
- Transmitted through blood and body fluids (mucosa).
- Can lead to chronic infection.
- Requires pre-existing hepatitis B to occur.
- Rare in the US.
Hepatitis E
- Transmitted through the fecal-oral route (contaminated water).
- Does not cause chronic infection.
- Rare in the US, but can be severe in pregnant women.
Acute Hepatitis: Phases
- Prodromal period: Asymptomatic, lasts two weeks after exposure.
- Icteric period: Begins with jaundice (yellow skin, eyes), lasts two to six weeks, accompanied by enlarged, tender liver, dark urine, and clay-colored stools.
- Recovery period: Begins with the resolution of jaundice.
Chronic and Fulminant Hepatitis
- Chronic hepatitis: Lasts longer than six months, varies in severity, and can deteriorate quickly.
- Fulminant hepatitis: Rapidly progressing form leading to liver failure and death.
Hepatitis: Diagnosis
- History and physical exam.
- Liver profile (liver enzymes, clotting studies).
- Liver biopsy.
- Abdominal ultrasound.
Hepatitis: Treatment
- Vaccinations are the cornerstone of prevention.
- Limit exposure to the virus.
- Hepatitis A usually resolves with no treatment.
- Other viral hepatitis types are treated with interferon injections and antiviral medications.
- Rest, nutrition, increased hydration.
- Paracentesis.
- Liver transplant, if needed.
Hepatitis A Vaccine
- Recommended for children starting at one year of age and adults at risk (travelers, men who have sex with men, IV drug users, people with liver disease).
Hepatitis B Vaccine
- Recommended for all infants (started in the early 1990s) and adults at risk (healthcare workers, men who have sex with men, IV drug users).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.