Podcast
Questions and Answers
What is one of the primary functions of the circulatory system?
What is one of the primary functions of the circulatory system?
- Control body movements
- Store energy in muscles
- Regulate breathing rate
- Transport and distribute essential substances to the tissues (correct)
Which component is NOT a part of the circulatory system?
Which component is NOT a part of the circulatory system?
- Veins
- Arteries
- Nerves (correct)
- Capillaries
What structure in the heart ensures one-way blood flow?
What structure in the heart ensures one-way blood flow?
- Valves (correct)
- Arteries
- Muscle fibers
- Veins
Which circuit is specifically responsible for transporting blood to and from the lungs?
Which circuit is specifically responsible for transporting blood to and from the lungs?
What characteristic differentiates cardiac muscle from skeletal muscle?
What characteristic differentiates cardiac muscle from skeletal muscle?
What is the primary role of the heart's pump function?
What is the primary role of the heart's pump function?
How does the heart adapt blood delivery to changing metabolic needs?
How does the heart adapt blood delivery to changing metabolic needs?
What type of muscle cells make up cardiac muscle?
What type of muscle cells make up cardiac muscle?
What is the role of the tricuspid valve in the heart?
What is the role of the tricuspid valve in the heart?
Which chamber of the heart receives deoxygenated blood from the lungs?
Which chamber of the heart receives deoxygenated blood from the lungs?
During which phase of the cardiac cycle does active muscle contraction occur?
During which phase of the cardiac cycle does active muscle contraction occur?
What is the primary function of the semilunar valves in the heart?
What is the primary function of the semilunar valves in the heart?
Which side of the heart is responsible for pumping blood to the systemic circuit?
Which side of the heart is responsible for pumping blood to the systemic circuit?
How long does a typical cardiac cycle last?
How long does a typical cardiac cycle last?
What allows the heart to achieve the correct pressure relationships during the cardiac cycle?
What allows the heart to achieve the correct pressure relationships during the cardiac cycle?
What prevents backflow of blood from the ventricles to the atria?
What prevents backflow of blood from the ventricles to the atria?
What is one possible reason for a decrease in ejection fraction?
What is one possible reason for a decrease in ejection fraction?
Which wave corresponds to right atrial contraction in the jugular wave form?
Which wave corresponds to right atrial contraction in the jugular wave form?
How does aging affect pulse pressure in patients?
How does aging affect pulse pressure in patients?
What does the 'v' wave in the jugular wave form represent?
What does the 'v' wave in the jugular wave form represent?
What is the typical range for systolic blood pressure in a normal adult?
What is the typical range for systolic blood pressure in a normal adult?
What factor can cause increased arterial blood pressure in elderly individuals?
What factor can cause increased arterial blood pressure in elderly individuals?
What does the 'c' wave in the jugular wave form correspond to?
What does the 'c' wave in the jugular wave form correspond to?
What relationship does sex have on arterial blood pressure among adults?
What relationship does sex have on arterial blood pressure among adults?
What occurs during the repolarization phase of a cardiac action potential?
What occurs during the repolarization phase of a cardiac action potential?
Which of the following describes the absolute refractory period of cardiac muscle?
Which of the following describes the absolute refractory period of cardiac muscle?
According to the Frank-Starling law of the heart, what is the relationship between the stretch of heart muscle and the force of contraction?
According to the Frank-Starling law of the heart, what is the relationship between the stretch of heart muscle and the force of contraction?
Which of the following factors does NOT affect the rhythmicity of the heart?
Which of the following factors does NOT affect the rhythmicity of the heart?
What is the role of sodium in cardiac muscle function?
What is the role of sodium in cardiac muscle function?
Which structure is considered the pacemaker of the heart?
Which structure is considered the pacemaker of the heart?
What characterizes the contractility of cardiac muscle compared to skeletal muscle?
What characterizes the contractility of cardiac muscle compared to skeletal muscle?
What happens to the left ventricle during diastole when preload increases?
What happens to the left ventricle during diastole when preload increases?
What does afterload refer to in cardiovascular physiology?
What does afterload refer to in cardiovascular physiology?
During the contraction of cardiac muscle, what is the effect of calcium ions?
During the contraction of cardiac muscle, what is the effect of calcium ions?
Which formula represents cardiac output (CO)?
Which formula represents cardiac output (CO)?
How is stroke volume (SV) calculated?
How is stroke volume (SV) calculated?
What is a normal range for ejection fraction (EF) in healthy individuals?
What is a normal range for ejection fraction (EF) in healthy individuals?
What condition can lead to a reduced ejection fraction?
What condition can lead to a reduced ejection fraction?
What does cardiac reserve refer to?
What does cardiac reserve refer to?
Which chamber is primarily measured for ejection fraction?
Which chamber is primarily measured for ejection fraction?
What function does the AV node serve in the cardiac conduction system?
What function does the AV node serve in the cardiac conduction system?
Which type of cells initiate action potentials in the heart?
Which type of cells initiate action potentials in the heart?
How do sympathetic neurons affect heart rate?
How do sympathetic neurons affect heart rate?
What is the role of Purkinje fibers in the cardiac conduction system?
What is the role of Purkinje fibers in the cardiac conduction system?
What neurotransmitter is primarily involved in parasympathetic stimulation of the heart?
What neurotransmitter is primarily involved in parasympathetic stimulation of the heart?
What is the effect of epinephrine and norepinephrine on heart physiology?
What is the effect of epinephrine and norepinephrine on heart physiology?
Which of the following accurately describes the roles of the cardiac center in the medulla?
Which of the following accurately describes the roles of the cardiac center in the medulla?
What is a characteristic of auto-rhythmic cells in the heart?
What is a characteristic of auto-rhythmic cells in the heart?
Flashcards
What is the circulatory system?
What is the circulatory system?
The circulatory system is a closed loop, like a highway with the heart as the pump, using pressure to ensure blood flows from big arteries to small capillaries and back through veins.
What are the main functions of the circulatory system?
What are the main functions of the circulatory system?
The main functions of the circulatory system include transporting essential substances to tissues, removing waste products, regulating oxygen and nutrient supply based on needs, controlling body temperature, and enabling communication between organs.
What is the heart's role in the circulatory system?
What is the heart's role in the circulatory system?
The heart plays a crucial role in the circulatory system by generating blood pressure to ensure efficient blood flow. It also directs blood to different areas through separate circuits, and acts as a one-way valve using a system of chambers and valves.
What are the two major circuits of the circulatory system?
What are the two major circuits of the circulatory system?
Signup and view all the flashcards
Describe the movement of blood within the circulatory system.
Describe the movement of blood within the circulatory system.
Signup and view all the flashcards
What is special about cardiac muscle cells?
What is special about cardiac muscle cells?
Signup and view all the flashcards
What is the right atrium's function?
What is the right atrium's function?
Signup and view all the flashcards
Right Atrium
Right Atrium
Signup and view all the flashcards
Left Atrium
Left Atrium
Signup and view all the flashcards
Right Ventricle
Right Ventricle
Signup and view all the flashcards
Left Ventricle
Left Ventricle
Signup and view all the flashcards
Left ventricle - more muscular
Left ventricle - more muscular
Signup and view all the flashcards
Atrioventricular Valves
Atrioventricular Valves
Signup and view all the flashcards
Semilunar Valves
Semilunar Valves
Signup and view all the flashcards
Diastole
Diastole
Signup and view all the flashcards
Repolarization Phase
Repolarization Phase
Signup and view all the flashcards
Absolute Refractory Period
Absolute Refractory Period
Signup and view all the flashcards
Relative Refractory Period
Relative Refractory Period
Signup and view all the flashcards
Frank-Starling Law of the Heart
Frank-Starling Law of the Heart
Signup and view all the flashcards
End-Diastolic Volume
End-Diastolic Volume
Signup and view all the flashcards
Contractility
Contractility
Signup and view all the flashcards
Automaticity
Automaticity
Signup and view all the flashcards
Rhythmicity
Rhythmicity
Signup and view all the flashcards
What are auto-rhythmic cells?
What are auto-rhythmic cells?
Signup and view all the flashcards
Why is the AV node important?
Why is the AV node important?
Signup and view all the flashcards
What are Purkinje fibers?
What are Purkinje fibers?
Signup and view all the flashcards
What is the effect of sympathetic stimulation on the heart?
What is the effect of sympathetic stimulation on the heart?
Signup and view all the flashcards
What is the effect of parasympathetic stimulation on the heart?
What is the effect of parasympathetic stimulation on the heart?
Signup and view all the flashcards
How do hormones regulate heart function?
How do hormones regulate heart function?
Signup and view all the flashcards
What is the role of the cardioaccelerator center?
What is the role of the cardioaccelerator center?
Signup and view all the flashcards
What is the role of the cardioinhibitory center?
What is the role of the cardioinhibitory center?
Signup and view all the flashcards
Cardiac output (CO)
Cardiac output (CO)
Signup and view all the flashcards
Preload
Preload
Signup and view all the flashcards
Afterload
Afterload
Signup and view all the flashcards
Ejection Fraction (EF)
Ejection Fraction (EF)
Signup and view all the flashcards
Cardiac Reserve
Cardiac Reserve
Signup and view all the flashcards
End-Systolic Volume (ESV)
End-Systolic Volume (ESV)
Signup and view all the flashcards
End-Diastolic Volume (EDV)
End-Diastolic Volume (EDV)
Signup and view all the flashcards
Stroke Volume (SV)
Stroke Volume (SV)
Signup and view all the flashcards
Ejection Fraction: What is it?
Ejection Fraction: What is it?
Signup and view all the flashcards
Aorta's Role in Blood Pressure
Aorta's Role in Blood Pressure
Signup and view all the flashcards
Jugular Waveform: 'a' and 'c' Waves
Jugular Waveform: 'a' and 'c' Waves
Signup and view all the flashcards
Jugular Waveform: 'x' Descent
Jugular Waveform: 'x' Descent
Signup and view all the flashcards
Jugular Waveform: 'x' Prime ('x') Descent
Jugular Waveform: 'x' Prime ('x') Descent
Signup and view all the flashcards
Jugular Waveform: 'v' Wave
Jugular Waveform: 'v' Wave
Signup and view all the flashcards
Jugular Waveform: 'y' Descent
Jugular Waveform: 'y' Descent
Signup and view all the flashcards
Arterial Blood Pressure: What is it?
Arterial Blood Pressure: What is it?
Signup and view all the flashcards
Study Notes
The Cardiovascular System
- The cardiovascular system is a closed circuit.
- It contains a pump (the heart) that maintains a pressure gradient.
- This gradient sustains effective blood flow.
- Blood flows from distributing ducts (arteries) to thin vessels (capillaries).
- Blood flows back through collecting ducts (veins).
The Cardiovascular Circuit
- The main circuit has three components:
- Pump
- Distributing tubules
- Thin vessels/Collecting tubules
Main Functions of the Circulatory System
- Transports and distributes essential substances to tissues.
- Removes metabolic by-products.
- Adjusts oxygen and nutrient supply in various physiological states.
- Regulates body temperature.
- Facilitates humoral communication.
Functions of the Heart
- Generates blood pressure.
- Routes blood (separates pulmonary and systemic circulations).
- Ensures one-way blood flow (valves).
- Regulates blood supply (adjusts contraction rate and force to match metabolic needs).
Circuits of the Heart
- Pulmonary circuit: blood flow to and from the lungs
- Systemic circuit: blood flow to and from the rest of the body.
- Vessels carry blood through these circuits:
- Arteries carry blood away from the heart.
- Veins carry blood to the heart.
- Capillaries facilitate exchange.
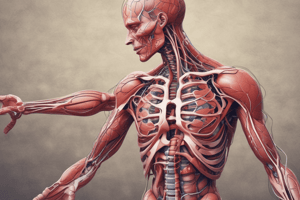
Cardiac Muscle
- Elongated, branching cells with centrally located nuclei.
- Contains actin and myosin myofilaments.
- Intercalated discs: specialized cell-cell contacts and gap junctions that allow action potentials to move from one cell to the next.
- Cardiac muscle of the atria and ventricles functions as a single unit.
- Mitochondria comprise 30% of the cell volume.
Chambers of the Heart
- Right atrium: Receives blood from systemic circulation. There is no valve between Vena Cava & the Right atrium.
- Left atrium: Receives deoxygenated blood from the lungs.
- Right ventricle: Pumps blood to the lungs via pulmonary arteries.
- Left ventricle: Pumps oxygenated blood to systemic circulation via the aorta.
- The left side of the heart is more muscular than the right side.
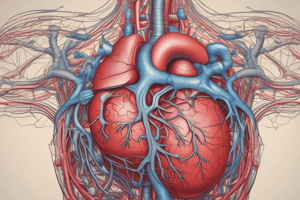
Heart Valves
- Atrioventricular (AV) valves are between atria and ventricles:
- Tricuspid (right side)
- Bicuspid (left side)
- Semilunar valves prevent backflow into the ventricles:
- Pulmonary
- Aortic
- AV valves stop blood from flowing back from the ventricles to the atria.
- Semilunar valves stop blood from flowing back into the ventricles.
- Valves and connective tissue make up the heart skeleton. They do not conduct electrical impulses.
Diastole and Systole
- Cardiac cycle: the electrical and physical events of a complete heartbeat (0.8 seconds).
- Diastole: resting phase, no active contraction.
- Systole: active muscle contraction and electrical impulses.
Cardiac Cycle
- Refers to all events associated with blood flow through the heart, from the start of one heartbeat to the next.
- Each heart chamber goes through systole and diastole.
- Correct pressure relationships depend on careful timing of contractions.
Phases of the Cardiac Cycle
- Atrial diastole and systole: Blood flows passively into the atria. Then atrial systole pumps the remaining blood into the ventricles.
- Ventricular filling (mid-to-late diastole): Heart blood pressure is low, blood passively enters ventricles
- Ventricular systole: Atrial relaxation. Ventricles will contract, pushing blood out into the arteries.
Characteristics of the Heart
- Excitability: cells respond to an electrical stimulus.
- Contractility: specialized cardiac muscle ability to contract.
- Rhythmicity: ability of the cardiac muscle to contract and relax regularly (automaticity: cells can depolarize without outside stimulus).
- Conductivity: cells can propagate electrical impulses from cell to cell.
Action Potentials in Skeletal and Cardiac Muscle
- Action potentials differ in skeletal and cardiac muscle. The plateau phase in the cardiac action potential is absent in skeletal muscle. This plateau differentiates the two and allows for a longer refractory period in the cardiac tissue.
Refractory Periods
- Relative refractory period: the cell can respond to an action potential, but it must be stronger.
- Absolute refractory period: cell does not respond to a re-stimulation, regardless of the strength of the stimulus (occurs during systole and part of diastole).
Contractility
- Frank-Starling law of the heart regulates stroke volume and force.
- The greater the stretch of the heart muscle, the stronger the contraction.
- End-diastolic volume represents measure of the blood flow into and stretch of the ventricles.
- The Frank-Starling law suggests that for normal healthy conditions, the heart pumps all of the blood that returns to it by way of the veins to the greatest extent during a heart beat.
- The heart muscle is stimulated by nerves and is self-excitable (automaticity).
- It contracts as a unit, no motor units.
- Has a long (250ms) absolute refractory period.
- Cardiac muscle contraction similar to skeletal muscle contraction, i.e., sliding filaments.
Rhythmicity
- Factors affecting rhythmicity:
- Autonomic innervation
- Electrolytes: Sodium (depolarization), Potassium (repolarization), Calcium (depolarization, myocardial contraction)
- Temperature
- Blood pH
Conducting System of the Heart
- SA node (pacemaker): generates spontaneous action potentials and initiates contractions.
- AV node: conducts action potentials more slowly to ensure atria contract before ventricles.
- AV bundle: carries action potentials to the ventricles.
- Bundle branches: extend to the apex of the ventricles.
- Purkinje fibers: conduct action potentials to ventricular muscle cells.
- Auto-rhythmic cells initiate action potentials and they have unstable resting potentials (pacemaker potentials), and use calcium influx rather than sodium for the action potential.
Extrinsic Innervation of the Heart
- Vital centers in the medulla (cardioacceleratory and cardioinhibitory centers): cardiac regulating centers
- Cardioacceleratory center activates sympathetic nerve fibers increasing heart rate.
- Cardioinhibitory center activates parasympathetic nerve fibers, decreasing heart rate.
Regulation of the Heart
- Neural Regulation
- Sympathetic stimulation is a positive chronotropic factor, increasing heart rate and force of contraction.
- Supplied by cardiac nerves.
- Innervates the SA and AV nodes, atrial, and ventricular myocardium.
- Hormonal Regulation
- Epinephrine and norepinephrine from the adrenal medulla are released.
- Increased activity, emotions, and stress, cause increased heart rate.
- Parasympathetic stimulation is a negative chronotropic factor, decreasing heart rate.
- Supplied by the vagus nerve.
- Secretes acetylcholine.
- Hyperpolarizes the heart.
Chemical Regulation of the Heart
- Epinephrine and thyroxine hormones increase heart rate.
- Intra- and extracellular ion concentrations must be maintained for healthy heart function.
Heart Rate
- Pulse = surge of pressure in artery
- Infants have high heart rate.
- Young adult females have 72-80 bpm.
- Young adult males avg. 64 to 72 bpm.
- Heart rate rises in the elderly.
- Tachycardia is a resting heart rate above 100.
- Bradycardia is a resting heart rate less than 60.
Regulation of Heart Rate
- Chronotropism: influence on heart rate.
- Positive chronotropic factors increase heart rate.
- Negative chronotropic factors decrease heart rate.
- Inotropism: influence on contractility.
- Positive inotropic factors increase contractility.
- Negative chronotropic factors decrease contractility.
Factors Affecting Heart Rate
- Cardiovascular control center in medulla (cardioexcitatory and cardioinhibitory centers, autonomic nervous system (ANS))
- Neural reflexes:
- Atrial stretch receptors reflex
- Proprioceptor reflex
- Chemoreceptor reflex
- Baroreceptor reflex
- Nociceptor reflex
- Cerebral Cortex
- Venous return
- Skeletal muscle pump
- Muscular contractions squeeze adjacent veins, causing a “milking” action.
- Valves prevent backward flow.
- Constriction of veins, through sympathetic stimulation or gravity
- Preload: diastolic volume load before contraction starts (related to venous filling pressure).
- Afterload: systolic load on the left ventricle after contraction (resistance against pumping).
Cardiac Output (CO)
- Amount of blood pumped by each ventricle per minute.
- Calculated as heart rate (HR) multiplied by stroke volume (SV).
- CO = HR x SV (ml/min = beats/min x ml/beat)
- Cardiac reserve is the difference between resting and maximal CO.
- SV = EDV - ESV (End diastolic Volume – End systolic Volume)
Ejection Fraction (EF)
- Fraction of blood pumped out of the ventricles per heartbeat.
- EF = SV/EDV.
- Healthy individuals have an EF between 55%-70%.
- Reduced ejection fraction can manifest as heart failure.
Arterial Blood Pressure (BP)
- Pressure inside large arteries.
- Components: Systolic (maximum pressure) and Diastolic (minimum pressure).
- Normal adult ≈ 120/80 mmHg.
Factors Affecting Arterial Blood Pressure (ABP)
- Sex
- Age
- Emotions
- Exercise
- Hormones
- Gravity
- Race
- Sleep
- Pregnancy
Renin-Angiotensin System
- Important mechanism for sodium retention and maintaining blood volume.
- Any drop in renal blood flow or sodium prompts the juxtaglomerular apparatus in the kidneys to release renin.
- Renin activates the angiotensin system which leads to aldosterone production.
Antidiuretic Hormone (ADH)
- Hypovolemia and dehydration stimulate osmoreceptors in the hypothalamus, leading to ADH release from the posterior pituitary.
- ADH causes water reabsorption in kidney tubules.
Low-Pressure Volume Receptors
- Atrial natriuretic peptide (ANP) hormone regulates sodium excretion from the wall of the right atrium.
Electrocardiogram (ECG/EKG)
- Records electrical events in the myocardium.
- Key components:
- P-wave: atrial depolarization
- QRS complex: ventricular depolarization
- T-wave: ventricular repolarization
- Intervals and segments: indicate timing and health of the conduction system
Laminar vs. Turbulent Flow
- Laminar flow: smooth, orderly flow
- Turbulent flow: disrupted flow, often associated with constrictions.
Jugular Wave Form
- Shows changes in venous pressure related to heart activity
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.