Podcast
Questions and Answers
What is the primary effect of CKD on the kidneys?
What is the primary effect of CKD on the kidneys?
- Decrease in the volume of urine produced
- Increase in the filtration rate of the glomeruli
- Increase in the number of functional nephrons
- Decrease in the number of functional nephrons (correct)
What is the primary mechanism by which CKD progresses to end-stage renal disease (ESRD)?
What is the primary mechanism by which CKD progresses to end-stage renal disease (ESRD)?
- Increased blood flow to the kidneys
- A vicious cycle of injury and adaptation (correct)
- Overproduction of erythropoietin
- Decreased levels of creatinine in the blood
Which of the following is NOT a factor that can contribute to the development of CKD?
Which of the following is NOT a factor that can contribute to the development of CKD?
- Increased production of erythropoietin (correct)
- Tubular disorders
- Lower urinary tract disorders
- Glomerular disorders
What is the primary mechanism by which increased pressure in the glomeruli contributes to CKD progression?
What is the primary mechanism by which increased pressure in the glomeruli contributes to CKD progression?
How does the loss of functional nephrons in CKD impact the remaining nephrons?
How does the loss of functional nephrons in CKD impact the remaining nephrons?
What is the most effective method to slow down the progression of CKD to ESRD?
What is the most effective method to slow down the progression of CKD to ESRD?
CKD can be caused by disorders related to which of the following?
CKD can be caused by disorders related to which of the following?
Which of the following is NOT a common cause of end-stage renal disease (ESRD)?
Which of the following is NOT a common cause of end-stage renal disease (ESRD)?
What is the primary characteristic of nephrotic syndrome?
What is the primary characteristic of nephrotic syndrome?
What is the primary cause of protein loss in the urine in nephrotic syndrome?
What is the primary cause of protein loss in the urine in nephrotic syndrome?
Which of the following is NOT a common cause of nephrotic syndrome?
Which of the following is NOT a common cause of nephrotic syndrome?
What is the primary difference between acute and chronic glomerulonephritis in terms of streptococcal infections?
What is the primary difference between acute and chronic glomerulonephritis in terms of streptococcal infections?
What is the primary consequence of the progressive damage of renal tubules, glomeruli, and other structures in chronic glomerulonephritis?
What is the primary consequence of the progressive damage of renal tubules, glomeruli, and other structures in chronic glomerulonephritis?
What happens to the glomerular capillary filtration coefficient in the later stages of chronic glomerulonephritis?
What happens to the glomerular capillary filtration coefficient in the later stages of chronic glomerulonephritis?
What is the main characteristic of interstitial nephritis?
What is the main characteristic of interstitial nephritis?
Why is the glomerular filtration coefficient reduced in the final stages of chronic glomerulonephritis?
Why is the glomerular filtration coefficient reduced in the final stages of chronic glomerulonephritis?
What is the primary cause of damage to the kidneys in this specific type of AKI?
What is the primary cause of damage to the kidneys in this specific type of AKI?
What happens to the glomerular cells once the immune complex is deposited?
What happens to the glomerular cells once the immune complex is deposited?
What is a likely consequence of the inflammatory reaction in the glomeruli?
What is a likely consequence of the inflammatory reaction in the glomeruli?
Which of the following is NOT a cause of the specific type of AKI described in the text?
Which of the following is NOT a cause of the specific type of AKI described in the text?
What is the primary cell type that proliferates in the glomeruli after immune complex deposition?
What is the primary cell type that proliferates in the glomeruli after immune complex deposition?
What effect does the blockage of glomeruli have on the filtration process?
What effect does the blockage of glomeruli have on the filtration process?
What is the timeframe for potential repair of the tubules, assuming the basement membrane remains intact?
What is the timeframe for potential repair of the tubules, assuming the basement membrane remains intact?
What is the name of the category of AKI described in the text?
What is the name of the category of AKI described in the text?
What happens to the sodium-potassium–adenosine triphosphatase pump (Na+-K+ ATPase pump) when sodium entry into the epithelial cells is decreased?
What happens to the sodium-potassium–adenosine triphosphatase pump (Na+-K+ ATPase pump) when sodium entry into the epithelial cells is decreased?
What is the main reason for the high blood flow to the kidneys?
What is the main reason for the high blood flow to the kidneys?
What is the primary consequence of decreased renal blood flow?
What is the primary consequence of decreased renal blood flow?
Which of the following conditions can lead to prerenal acute kidney injury (AKI) by causing intravascular volume depletion?
Which of the following conditions can lead to prerenal acute kidney injury (AKI) by causing intravascular volume depletion?
Why are sodium channel blockers considered potassium-sparing diuretics?
Why are sodium channel blockers considered potassium-sparing diuretics?
What is the primary cause of postrenal AKI?
What is the primary cause of postrenal AKI?
Which of the following conditions is NOT a direct cause of prerenal AKI?
Which of the following conditions is NOT a direct cause of prerenal AKI?
Which of the following statements is TRUE about the relationship between sodium and potassium regulation in the kidney?
Which of the following statements is TRUE about the relationship between sodium and potassium regulation in the kidney?
Which of these are metabolic disorders that can cause chronic kidney disease?
Which of these are metabolic disorders that can cause chronic kidney disease?
What are the primary causes of chronic kidney disease?
What are the primary causes of chronic kidney disease?
Which of the following is NOT a renal vascular disorder that can cause chronic kidney disease?
Which of the following is NOT a renal vascular disorder that can cause chronic kidney disease?
What is the name of the primary kidney disease that can result in a vicious cycle of glomerular sclerosis, hypertrophy, and vasodilation of surviving nephrons?
What is the name of the primary kidney disease that can result in a vicious cycle of glomerular sclerosis, hypertrophy, and vasodilation of surviving nephrons?
What is the most likely outcome of untreated chronic kidney disease?
What is the most likely outcome of untreated chronic kidney disease?
Which of the following is NOT a primary tubular disorder?
Which of the following is NOT a primary tubular disorder?
Which of the following is a factor that can contribute to the vicious cycle of chronic kidney disease?
Which of the following is a factor that can contribute to the vicious cycle of chronic kidney disease?
What is the primary difference between acute kidney injury (AKI) and chronic kidney disease (CKD)?
What is the primary difference between acute kidney injury (AKI) and chronic kidney disease (CKD)?
As the number of nephrons decreases below 5% to 10% of normal, what is the primary consequence for the patient?
As the number of nephrons decreases below 5% to 10% of normal, what is the primary consequence for the patient?
Why do waste products like urea and creatinine accumulate in proportion to the number of nephrons lost?
Why do waste products like urea and creatinine accumulate in proportion to the number of nephrons lost?
How does the body maintain relatively constant plasma concentrations of electrolytes like sodium and chloride despite a decrease in GFR?
How does the body maintain relatively constant plasma concentrations of electrolytes like sodium and chloride despite a decrease in GFR?
Which of the following is TRUE regarding creatinine excretion?
Which of the following is TRUE regarding creatinine excretion?
When 75% of the nephrons are lost, how does the workload change for the remaining nephrons?
When 75% of the nephrons are lost, how does the workload change for the remaining nephrons?
What is the relationship between the decline in GFR and the rise in plasma concentrations of electrolytes?
What is the relationship between the decline in GFR and the rise in plasma concentrations of electrolytes?
Which of the following best describes the mechanism by which the body maintains relatively constant plasma concentrations of urea and creatinine as GFR declines?
Which of the following best describes the mechanism by which the body maintains relatively constant plasma concentrations of urea and creatinine as GFR declines?
What is the primary difference between the way the body manages the accumulation of electrolytes and waste products like urea and creatinine in the setting of declining GFR?
What is the primary difference between the way the body manages the accumulation of electrolytes and waste products like urea and creatinine in the setting of declining GFR?
Flashcards
Postrenal Acute Kidney Injury
Postrenal Acute Kidney Injury
Kidney injury caused by obstruction of urinary flow.
Sodium-Potassium Pump
Sodium-Potassium Pump
A pump that transports sodium out and potassium into cells.
Potassium-Sparing Diuretics
Potassium-Sparing Diuretics
Diuretics that reduce potassium excretion.
Prerenal Acute Kidney Injury
Prerenal Acute Kidney Injury
Signup and view all the flashcards
Causes of Prerenal AKI
Causes of Prerenal AKI
Signup and view all the flashcards
Normal Renal Blood Flow
Normal Renal Blood Flow
Signup and view all the flashcards
Glomerular Filtration Rate (GFR)
Glomerular Filtration Rate (GFR)
Signup and view all the flashcards
Urine Output
Urine Output
Signup and view all the flashcards
AKI after infection
AKI after infection
Signup and view all the flashcards
Immune complexes
Immune complexes
Signup and view all the flashcards
Glomeruli damage
Glomeruli damage
Signup and view all the flashcards
Mesangial cell proliferation
Mesangial cell proliferation
Signup and view all the flashcards
Tubular obstruction
Tubular obstruction
Signup and view all the flashcards
Basement membrane integrity
Basement membrane integrity
Signup and view all the flashcards
Excessive permeability
Excessive permeability
Signup and view all the flashcards
Postrenal AKI
Postrenal AKI
Signup and view all the flashcards
Acute Kidney Injury (AKI)
Acute Kidney Injury (AKI)
Signup and view all the flashcards
Chronic Kidney Disease (CKD)
Chronic Kidney Disease (CKD)
Signup and view all the flashcards
Renal Poisons
Renal Poisons
Signup and view all the flashcards
Diabetes Mellitus and CKD
Diabetes Mellitus and CKD
Signup and view all the flashcards
Hypertension in CKD
Hypertension in CKD
Signup and view all the flashcards
Nephrotoxins
Nephrotoxins
Signup and view all the flashcards
Glomerulonephritis
Glomerulonephritis
Signup and view all the flashcards
Urinary Tract Obstruction
Urinary Tract Obstruction
Signup and view all the flashcards
Chronic Glomerulonephritis
Chronic Glomerulonephritis
Signup and view all the flashcards
Nephrotic Syndrome
Nephrotic Syndrome
Signup and view all the flashcards
Glomerular Capillary Filtration Coefficient
Glomerular Capillary Filtration Coefficient
Signup and view all the flashcards
Fibrous Tissue Invasion
Fibrous Tissue Invasion
Signup and view all the flashcards
Increased Permeability of Glomerular Membrane
Increased Permeability of Glomerular Membrane
Signup and view all the flashcards
Interstitial Nephritis
Interstitial Nephritis
Signup and view all the flashcards
End-Stage Renal Disease (ESRD)
End-Stage Renal Disease (ESRD)
Signup and view all the flashcards
Vicious Cycle of CKD
Vicious Cycle of CKD
Signup and view all the flashcards
Increased Arterial Pressure
Increased Arterial Pressure
Signup and view all the flashcards
Glomerular Injury
Glomerular Injury
Signup and view all the flashcards
Nephron Sclerosis
Nephron Sclerosis
Signup and view all the flashcards
Functional Vasodilation
Functional Vasodilation
Signup and view all the flashcards
Adaptive Changes in Nephrons
Adaptive Changes in Nephrons
Signup and view all the flashcards
Nephron Loss Effects
Nephron Loss Effects
Signup and view all the flashcards
Waste Product Accumulation
Waste Product Accumulation
Signup and view all the flashcards
Creatinine Excretion Mechanics
Creatinine Excretion Mechanics
Signup and view all the flashcards
Sodium and Chloride Stability
Sodium and Chloride Stability
Signup and view all the flashcards
Increased Nephron Load
Increased Nephron Load
Signup and view all the flashcards
Tubular Reabsorption Role
Tubular Reabsorption Role
Signup and view all the flashcards
Creatinine Non-Reabsorption
Creatinine Non-Reabsorption
Signup and view all the flashcards
Glomerular Filtration Rate (GFR) Relation
Glomerular Filtration Rate (GFR) Relation
Signup and view all the flashcards
Study Notes
Diuretics and Their Mechanisms of Action
- Diuretics increase urine output and excretion of solutes, mainly sodium and chloride.
- Most diuretics work by reducing renal tubular sodium reabsorption, leading to increased water and solute excretion.
- Diuretics are clinically used to reduce extracellular fluid volume (edema) and in hypertension.
- Some diuretics can increase urine output significantly (20-fold) after administration.
Osmotic Diuretics
- Osmotic diuretics are substances filtered by the glomeruli but not readily reabsorbed in the renal tubules (e.g., urea, mannitol, sucrose).
- They increase the concentration of osmotically active molecules in the tubules, reducing water reabsorption and increasing urine output.
- Elevated blood glucose in diabetes mellitus can lead to osmotic diuresis, with excess glucose remaining in the tubules, increasing urine flow.
Loop Diuretics
- Powerful diuretics like furosemide, ethacrynic acid, and bumetanide.
- They block the sodium-chloride-potassium co-transporter in the thick ascending limb of the loop of Henle.
- This reduces sodium, chloride, and potassium reabsorption, significantly increasing urine output.
- Loop diuretics affect the countercurrent multiplier system, decreasing medullary interstitial fluid concentration, reducing the kidneys' ability to concentrate or dilute urine.
Thiazide Diuretics
- Thiazide derivatives (e.g., chlorothiazide) mainly act on the early distal tubules.
- They block the sodium-chloride co-transporter, decreasing sodium and chloride reabsorption and increasing urine output.
- The maximum effect of these diuretics is typically 5-10% of the glomerular filtrate.
Carbonic Anhydrase Inhibitors
- Acetazolamide inhibits the carbonic anhydrase enzyme essential for bicarbonate reabsorption in the proximal tubules.
- This decreases sodium reabsorption leading to increased urine output.
- Side effect: causes acidosis due to excessive bicarbonate loss in urine.
Mineralocorticoid Receptor Antagonists
- Spironolactone and eplerenone compete with aldosterone for receptor sites in the collecting tubules.
- Decreasing sodium reabsorption and increasing potassium secretion.
- Referred to as potassium-sparing diuretics.
Sodium Channel Blockers
- Amiloride and triamterene block sodium entry into the sodium channels of collecting tubule cells.
- Decreasing sodium reabsorption and potassium secretion.
- Potassium-sparing diuretics.
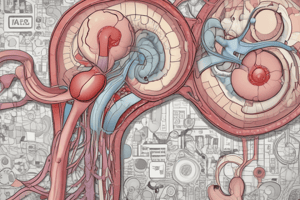
Kidney Diseases
- Kidney diseases are significant causes of mortality and morbidity worldwide.
- Acute kidney injury (AKI) is an abrupt loss of kidney function.
- Chronic kidney disease (CKD) involves progressive loss of nephron function and function. -Prerenal, Intrarenal, Postrenal
- Causes of AKI include decreased blood supply, intrarenal abnormalities, and postrenal obstructions.
- CKD's causes include factors like diabetes, hypertension, glomerulonephritis, and other conditions.
Acute Kidney Injury (AKI)
- AKI results from decreased blood supply, intrarenal or postrenal conditions.
- Pre-renal AKI: reduced kidney supply, e.g., heart failure, or reduced blood volume.
- Intrarenal AKI: conditions within the kidney itself, e.g., tubular necrosis, vasculitis.
- Postrenal AKI: obstruction to urine flow, e.g., kidney stones.
Chronic Kidney Disease (CKD)
- CKD results in progressive loss of nephron function, often leading to end-stage renal disease (ESRD).
Other Kidney Disorders
- Tubular Necrosis, Nephrotic Syndrome
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.