Podcast
Questions and Answers
What is a defining characteristic of Chronic Kidney Disease (CKD)?
What is a defining characteristic of Chronic Kidney Disease (CKD)?
- Presence of proteinuria less than 30 mg/day
- Abnormalities in kidney structure or function for more than 3 months (correct)
- Normal glomerular filtration rate (GFR)
- Presence of hyperglycemia
Which of the following is an example of a structural abnormality indicative of CKD?
Which of the following is an example of a structural abnormality indicative of CKD?
- Albuminuria greater than 30 mg/day (correct)
- Normal electrolyte levels
- Blood urea nitrogen levels less than 20 mg/dL
- GFR greater than 60 mL/min
What dietary recommendation is advised for patients with hypertension and CKD?
What dietary recommendation is advised for patients with hypertension and CKD?
- Low-sodium diet (correct)
- No dietary restrictions
- High-protein diet
- High-sodium diet
What is the maximum recommended daily intake of elemental calcium for patients using oral calcium salts to bind phosphate?
What is the maximum recommended daily intake of elemental calcium for patients using oral calcium salts to bind phosphate?
For CKD patients experiencing severe hyperphosphatemia, which is considered a first-line treatment option?
For CKD patients experiencing severe hyperphosphatemia, which is considered a first-line treatment option?
Flashcards are hidden until you start studying
Study Notes
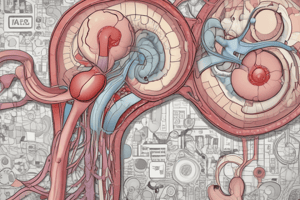
Definition of Chronic Kidney Disease (CKD)
- CKD is characterized by structural or functional kidney abnormalities lasting 3 months or longer.
- Structural abnormalities include:
- Albuminuria >30 mg/day
- Hematuria or red cell casts in urine sediment
- Electrolyte imbalances
- Decreased Glomerular Filtration Rate (GFR) is indicative of functional impairment.
Classification and Etiology of CKD
- CKD can be categorized based on cause, duration, and GFR levels.
- Common etiologies: diabetes, hypertension, glomerulonephritis, and polycystic kidney disease.
Pathophysiology of CKD
- Progression is often associated with glomerulosclerosis, nephron loss, and interstitial fibrosis.
- Complications include fluid overload, metabolic acidosis, and electrolyte disturbances.
Clinical Manifestations of CKD
- Symptoms vary but may include:
- Fatigue
- Swelling in limbs
- Changes in urine output
- Bone pain due to mineral and bone disorder
- Anemia
Diagnostic Tests for CKD
- Routine tests include:
- Serum creatinine to calculate GFR
- Urine test for protein, blood, and electrolytes
- Imaging to assess kidney structure.
Treatment Goals
- Slow progression of kidney disease.
- Manage complications and comorbid conditions.
- Delay the need for dialysis or transplantation.
Treatment
- Pharmacological options vary based on specific complications:
- Control hypertension and diabetes.
- Phosphate binders for hyperphosphatemia.
- Nonpharmacological interventions include lifestyle modifications and dietary restrictions.
Dialysis in CKD
- Dialysis becomes necessary when GFR falls below critical thresholds, typically around 15 mL/min.
- Hemodialysis and peritoneal dialysis are the two primary methods.
Renal Transplant
- Considered for eligible patients when CKD progresses to end-stage renal disease (ESRD).
- Offers improved quality of life and survival compared to long-term dialysis.
Nonpharmacological Treatment
- Renal diet restrictions are crucial in the management of CKD.
- Hypertensive patients should adhere to a low-sodium diet.
- Emphasis on smoking cessation and limited alcohol intake (2 drinks/day for men, 1 for women).
Management of Hyperphosphatemia
- Oral calcium salts as the first line for severe hyperphosphatemia, binding phosphorus in the GI tract.
- Elemental calcium intake should not exceed 1500 mg/day.
- Phosphate-Binding Agents include:
- Calcium Carbonate: 0.5-1g taken three times daily with meals.
- Sevelamer HCl/Sevelamer carbonate: 800–1600 mg three times a day with meals.
- Lanthanum Carbonate: 750–1500 mg/day, titrated up to 1000-3000 mg/day over time.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.