Podcast
Questions and Answers
What characterizes cervical radiculopathy?
What characterizes cervical radiculopathy?
- Symptoms only in the legs
- Only pain without sensory changes
- Bilateral muscle weakness and sensory normality
- Unilateral muscle weakness and sensory alterations (correct)
Which cervical nerve root is primarily responsible for shoulder elevation?
Which cervical nerve root is primarily responsible for shoulder elevation?
- C3
- C5
- C1
- C4 (correct)
What is a common symptom associated with disc herniation in the cervical spine?
What is a common symptom associated with disc herniation in the cervical spine?
- Isolated arm pain without neck involvement
- Severe neck pain that radiates into the arm (correct)
- Pain relief with movement
- Bilateral neck stiffness
In terms of upper crossed syndrome, which muscles are typically noted as weak?
In terms of upper crossed syndrome, which muscles are typically noted as weak?
What is indicated by an absence of one movement during neck flexion?
What is indicated by an absence of one movement during neck flexion?
What is the normal lordotic curvature of the cervical spine?
What is the normal lordotic curvature of the cervical spine?
Which cervical vertebra is the first palpable spinous process below the occipital bone?
Which cervical vertebra is the first palpable spinous process below the occipital bone?
Which joint is primarily responsible for the motion of rotation in the cervical spine?
Which joint is primarily responsible for the motion of rotation in the cervical spine?
What are the symptoms commonly associated with injuries in the cervicoencephalic region?
What are the symptoms commonly associated with injuries in the cervicoencephalic region?
Which ligament is primarily responsible for holding the dens in place?
Which ligament is primarily responsible for holding the dens in place?
What is the most common mechanism of injury for the cervical spine?
What is the most common mechanism of injury for the cervical spine?
What type of joints are the joints of Luschka and what is their primary function?
What type of joints are the joints of Luschka and what is their primary function?
What percentage of blood supply to the brain is provided by the vertebral artery?
What percentage of blood supply to the brain is provided by the vertebral artery?
What changes occur with the age group related to cervical spondylosis?
What changes occur with the age group related to cervical spondylosis?
What is the position of greatest flexion and extension of the facet joints in the cervical spine?
What is the position of greatest flexion and extension of the facet joints in the cervical spine?
What is a common cause for Whiplash Associated Disorder (WAD)?
What is a common cause for Whiplash Associated Disorder (WAD)?
Which grade of Whiplash Associated Disorder presents with neck complaints and neurological signs?
Which grade of Whiplash Associated Disorder presents with neck complaints and neurological signs?
What type of torticollis involves a painful unilateral shortening or spasm of neck muscles?
What type of torticollis involves a painful unilateral shortening or spasm of neck muscles?
Which type of torticollis is often corrected surgically or through stretching?
Which type of torticollis is often corrected surgically or through stretching?
What is a characteristic symptom of Spasmodic Torticollis?
What is a characteristic symptom of Spasmodic Torticollis?
Which cervical special test is used to assess foraminal compression?
Which cervical special test is used to assess foraminal compression?
Which treatment technique is contraindicated for a patient with torticollis?
Which treatment technique is contraindicated for a patient with torticollis?
What is an important treatment technique for managing torticollis?
What is an important treatment technique for managing torticollis?
What condition is commonly associated with brachial plexus injuries?
What condition is commonly associated with brachial plexus injuries?
What typically prompts the symptoms of whiplash to appear after an injury?
What typically prompts the symptoms of whiplash to appear after an injury?
What movement deficiency is present in Grade 2 of Whiplash Associated Disorder?
What movement deficiency is present in Grade 2 of Whiplash Associated Disorder?
What is the main goal of the heat application in torticollis treatment?
What is the main goal of the heat application in torticollis treatment?
What is a potential result of congenital torticollis in infants?
What is a potential result of congenital torticollis in infants?
How can Pseudotorticollis be identified?
How can Pseudotorticollis be identified?
Flashcards
Cervical Radiculopathy
Cervical Radiculopathy
Injury to nerve roots in the spine, causing unilateral muscle weakness (myotome), and sensory changes (dermatome).
Disc Herniation
Disc Herniation
A condition causing severe neck pain that may radiate to the shoulder/arm, limiting range of motion, and worsening with activities like coughing or straining.
Upper Crossed Syndrome
Upper Crossed Syndrome
A postural issue involving tightness in the upper trapezius and levator scapulae, along with weakness in the rhomboids, serratus anterior, and lower trapezius, and weak deep neck flexors.
Cervical Myotomes
Cervical Myotomes
Signup and view all the flashcards
Upper vs. Lower Cervical Spine Flexion
Upper vs. Lower Cervical Spine Flexion
Signup and view all the flashcards
Cervical Spine Mobility
Cervical Spine Mobility
Signup and view all the flashcards
Cervical Spine Injury Risk
Cervical Spine Injury Risk
Signup and view all the flashcards
Cervical Spine Landmarks
Cervical Spine Landmarks
Signup and view all the flashcards
Atlanto-occipital Joint
Atlanto-occipital Joint
Signup and view all the flashcards
Atlanto-axial Joint
Atlanto-axial Joint
Signup and view all the flashcards
Vertebral Artery
Vertebral Artery
Signup and view all the flashcards
Facet Joints (Cervical)
Facet Joints (Cervical)
Signup and view all the flashcards
Joints of Luschka
Joints of Luschka
Signup and view all the flashcards
Cervical Nerve Roots
Cervical Nerve Roots
Signup and view all the flashcards
Cervical SP (spinous process) landmark
Cervical SP (spinous process) landmark
Signup and view all the flashcards
Whiplash Associated Disorder (WAD)
Whiplash Associated Disorder (WAD)
Signup and view all the flashcards
Grade 1 WAD
Grade 1 WAD
Signup and view all the flashcards
Grade 2 WAD
Grade 2 WAD
Signup and view all the flashcards
Grade 3 WAD
Grade 3 WAD
Signup and view all the flashcards
Grade 0 WAD
Grade 0 WAD
Signup and view all the flashcards
Brachial Plexus Injuries
Brachial Plexus Injuries
Signup and view all the flashcards
Acute Acquired Torticollis
Acute Acquired Torticollis
Signup and view all the flashcards
Pseudotorticollis
Pseudotorticollis
Signup and view all the flashcards
Congenital Torticollis
Congenital Torticollis
Signup and view all the flashcards
Spasmodic Torticollis
Spasmodic Torticollis
Signup and view all the flashcards
Hold-relax technique
Hold-relax technique
Signup and view all the flashcards
Contract-relax technique
Contract-relax technique
Signup and view all the flashcards
Agonist contract technique
Agonist contract technique
Signup and view all the flashcards
Spurling's test
Spurling's test
Signup and view all the flashcards
Study Notes
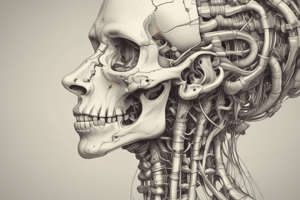
Cervical Spine Anatomy
- The cervical spine is designed for mobility, sacrificing stability. This makes it susceptible to injury due to its position between the head and the more stable thoracic spine.
- The spine exhibits a normal lordotic curve of approximately 30-35 degrees.
- Key landmarks include the second cervical vertebra (C2), which is the first palpable spinous process below the occipital bone, and C7 or T1, the most prominent spinous process at the base of the neck (C7 often slides forward with cervical extension).
Cervical Spine Divisions
- Cervicoencephalic (C0-C2): This region encompasses the upper cervical spine and is crucial because injuries here can affect the brain, brainstem, and spinal cord.
- Symptoms (Cervicoencephalic): Symptoms can range from headaches and fatigue to vertigo, poor concentration, hypertonia of the sympathetic nervous system, and irritability/mood changes.
- Atlanto-occipital Joint (C0-C1): Primarily responsible for flexion/extension (nodding).
- Atlanto-axial Joint (C1-C2): This is the most mobile joint in the spine, primarily involved in rotation. The transverse ligament of the atlas is a significant supporting ligament.
- Cervicobrachial (C3-C7): Pain from this region is often referred to the upper extremities. Symptoms characteristically include neck pain, arm pain, or both, headaches, restricted range of motion (ROM), paresthesia, altered myotomes/dermatomes, and radicular signs.
Cervical Spine Ligaments
- Alar Ligament: Originates from the lateral border of the dens and attaches to the dens.
- Transverse Ligament: Anchors the dens within the atlas.
- Cruciform/Cruciate Ligament: Composed of two projections stemming from the transverse ligament.
- Tectorial Membrane: Acts as a support structure for the cervical spine, transitioning from the posterior longitudinal ligament.
Vertebral Artery
- The vertebral artery passes through the transverse processes of the cervical vertebrae.
- It usually originates at C6 but may start as high as C4.
- It contributes 20% of the blood supply to the brain, supplementing the internal carotid artery (80%).
- The artery is located near facet joints and vertebral bodies, and its course can be compromised by osteophyte formation or facet injuries.
- Movement like rotation, extension, and traction can stress the artery.
- Common symptoms of vertebral artery compression are delayed and include vertigo, drop attacks, nausea, tinnitus, and visual disturbances.
Facet Joints
- Superior Facets: Face upward, backward, and medially.
- Inferior Facets: Face downward, forward, and laterally.
- These coupled movements allow for flexion and extension but limit individual rotation or side flexion.
- The greatest flexion/extension potential is at C4-C5 and C5-C6, and C6-C7 levels, with facet joint degeneration more likely to occur at these levels.
- The spinous processes at the facet joint level align with the same vertebrae.
- Resing Position: A midpoint between flexion and extension.
- Close-Pack Position: Full extension.
- CPR: Side flexion and rotation are equally limited in extension.
Joints of Luschka
- Located between C3-C7 and develop with age
- Pseudojoints resembling "vampire teeth" resembling joint formation.
- Develop due to degeneration of intervertebral discs.
- Contribute to limitation in side flexion.
- Provide stability.
Cervical Nerve Roots
- Named for the vertebrae below them.
History
- Age: Spondylosis prevalence typically increases with age, becoming significant past 25, present in 60% of those over 45, and 85% of those over 65.
- Symptoms: Bone pain usually immediate; muscle/ligament pain may be immediate (e.g., tear) or delayed (e.g., MVA); symptoms do not typically refer to the arm for C4 nerve root injuries or higher. Radiculopathy (nerve root injury) results in unilateral muscle weakness (myotome) and sensory alterations (dermatome). Disc herniation may cause severe neck pain radiating to the shoulder, scapula, or arm; ROM limitations; and increased pain with coughing, sneezing, jarring, or straining.
Observation
- Upper Crossed Syndrome: characterized by tight upper trapezius, levator scapulae muscles; and weak rhomboids, serratus anterior, and lower trapezius. Deep neck flexors (e.g., longus coli) are also sometimes weak.
Movement
- Upper vs. Lower Cervical Spine: During flexion, the upper cervical spine (C0-C2) nods, and the lower cervical spine (C2-C7) flexes.
Neurological
- Cervical Myotomes: Specific nerve roots control specific movements.
- Referred Pain: Facet joint pain referrals may mimic other conditions.
Pathologies and Common Dysfunctions
- Whiplash Associated Disorder (WAD): An acceleration/deceleration injury to the head and neck. It can include sprains, strains, facet irritation, disc herniation, and headaches.
- Brachial Plexus Injuries (Burners/Stingers): Result from stretching or compression of the brachial plexus.
- Torticollis: Abnormal head and neck position, commonly a unilateral head/neck flexion toward the affected side. Types exist (acute acquired, congenital, pseudotorticollis, spasmodic).
Special Tests for Cervical Spine
- Spurling's
- Distraction
- Valsalva
- Shoulder Abduction
- Lateral flexion Alar ligament stress test
- Transverse ligament
Treatment Techniques
- Various glides (anterior, lateral) and translations are commonly employed
- Passive and active stretching (including PNF), hold-relax, contract-relax, and agonist contract techniques.
Assessment for Torticollis
- Postural assessment.
- ROM assessment (active and passive).
- Agonist contracts are key.
- Heat therapy, O&I release, and trigger point work are indicated.
Contraindicated Techniques for Torticollis
- Passively stretching spasming muscles.
- Direct work on a spasming muscle belly.
- Deep contraction of the spasming muscle.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.